Surgical alternatives in irreparable ruptures of the posterosuperior cuff
Alternativas quirúrgicas en roturas irreparables del manguito posterosuperior
Resumen:
Las roturas irreparables posterosuperiores de manguito suelen conllevar una importante pérdida de función del hombro y dolor asociado. Para mejorar esta sintomatología y la calidad de vida de estos pacientes, así como para tratar de evitar la evolución de estas roturas en una posible artropatía secundaria a roturas del manguito rotador, el manejo quirúrgico puede estar indicado en aquellos pacientes en los que el tratamiento conservador haya fracasado.
Existen múltiples técnicas quirúrgicas descritas para el manejo de esta patología, tales como el desbridamiento con tenotomía/tenodesis del bíceps, las reparaciones parciales, la implantación del balón subacromial, la reconstrucción capsular superior, las transferencias tendinosas o la prótesis invertida de hombro. El éxito quirúrgico estará relacionado con la correcta elección por parte del cirujano de la técnica más indicada para cada paciente.
En la última década se ha popularizado el uso del balón subacromial y de la reconstrucción capsular superior para el manejo de este tipo de roturas. A continuación, se presentan estas dos técnicas quirúrgicas, sus indicaciones, funcionamiento y resultados clínicos hasta la fecha con el fin de aclarar las indicaciones de estos tratamientos para el manejo de las roturas posterosuperiores irreparables de manguito rotador en determinados pacientes.
Abstract:
Irreparable posterosuperior cuff ruptures usually result in important loss of shoulder function with associated pain. In order to improve the symptoms and patient quality of life, and to try to prevent progression towards possible arthropathy secondary to rotator cuff rupture, surgical management may be indicated in those individuals where conservative treatment has failed.
A number of techniques have been described for the management of this disorder, such as debridement with tenotomy / tenodesis of the biceps, partial repairs, the placement of a subacromial balloon, the superior capsule reconstruction, tendon transfers or reverse shoulder replacement procedures. Surgical success is related to a correct surgeon choice of the most adequate technique for each individual patient.
In the last decade, the subacromial balloon and superior capsule reconstruction have become popular for the management of ruptures of this kind. The present study describes these two techniques, their indications, functioning and clinical outcomes to date, with the purpose of clarifying their indications for dealing with irreparable posterosuperior rotator cuff ruptures in certain patients.
Introduction
Irreparable posterosuperior massive rupture is defined as rupture affecting the tendons of the supra- and infraspinatus (Collin type D)(1,2,3), and is associated to retraction of these tendons at glenoid level (Patte 3)(4) with fatty infiltration and high grade muscle atrophy (Goutalier 3-4)(5). Ruptures of this kind usually manifest clinically in the form of important shoulder dysfunction, including loss of mobility and pain. In addition, lack of integrity of the posterosuperior rotator cuff can give rise to eccentric loading of the humeral head over the glenoid cavity and acromion, with wear and consequent arthropathy secondary to rotator cuff rupture(6).
In order to revert the clinical manifestations and improve patient quality of life, posterosuperior massive cuff ruptures that fail to improve with conservative management usually require surgical procedures such as debridement with tenotomy / tenodesis of the biceps, partial repairs, the placement of a subacromial balloon, superior capsular reconstruction (SCR), tendon transfers or reverse shoulder replacement. Deciding which treatment option is best for a given patient may prove challenging. Therefore, in order to secure good results, each shoulder surgeon should have adequate knowledge of the indications, functioning and clinical outcomes of the different therapeutic modalities available(7). In this regard, the present study describes treatment with the subacromial balloon, superior capsular reconstruction and its bio-SCR variant.
Subacromial balloon
In 2012, Savarese et al.(8) published the technical description of the arthroscopic placement of a biodegradable balloon in the subacromial space (Figure 1)(9). Following insufflation, the balloon acts as a spacer, avoiding superior migration of the humeral head (Figure 2)(8). In irreparable cuff rupture, it has been reported that the balloon can restore glenohumeral biomechanics and improve shoulder function thanks to a descent of the humeral head and its centralization with respect to the glenoid cavity, restoration of the torque generated by the subscapularis and teres minor, and an increase in tension of the deltoid muscle(10,11,12). Lobao et al., through the simulation of irreparable cuff rupture in cadaver models, were able to demonstrate that the subacromial balloon appears to restore glenohumeral biomechanics during the immediate postoperative period(12).
The biodegradable balloon is composed of a polylactic compound and caprolactone copolymer with a half-life of about 12 months, and its weight is reduced to 60%, with a return to its initial size 6 months after placement(13). A magnetic resonance imaging study showed that 24 months after implantation, only a thick fibrotic layer could be distinguished between the humeral head and the acromion(14). Such fibrosis is a consequence of the inflammatory response around the implant and appears to be responsible for the fact that the restoration of glenohumeral function persists after disintegration of the balloon(14,15). To date, the histological studies have not evidenced the appearance of complications due to the chronic inflammation and/or systemic toxicity of the device(16).
During placement of the subacromial balloon, it is not advisable to perform an extensive bursectomy in order to avoid possible displacement of the balloon in the subacromial space. Debridement must be performed of all the soft tissue immediately above the supraglenoid tubercle in order to perform the required measurement. In some cases, we may need to add tenotomy / tenodesis of the long portion of the biceps(17). The balloon is inserted through the lateral portal, with the medial portion located above the superior glenoid margin (and remnant cuff, if any) and the lateral portion beneath the acromion, without extending beyond its lateral border. Once in the correct position, the device is insufflated with the volume of saline solution recommended by the manufacturer. Filling the balloon to above the recommended volume may result in increased tension of the deltoid muscle, pain, and an increased risk of displacement of the device. In this regard, if it is not possible to insufflate the entire volume, it is advisable for the balloon to be left less inflated in order to avoid such complications(8).
No consensus has been reached to date regarding the definitive indications of the technique, mainly because of the heterogeneity of the different studies in terms of the conditions for placing the subacromial balloon, and the lack of long term studies and/or controlled trials(18).
This surgical technique was initially described in patients showing no improvement with conservative management, and who met one of the following requirements(8):
- Isolated irreparable rupture of the tendon of the supraspinatus.
- Irreparable rupture of the tendon of the supraspinatus associated to reparable rupture of the tendon of the infraspinatus.
- Irreparable posterosuperior rupture of the rotator cuff, with an intact or reparable ruptured tendon of the subscapularis.
In order to guarantee the effectiveness of the surgical technique, the tendon of the subscapularis and the tendon of the teres minor must be normally functioning and intact(18). In this way we can guarantee restoration of the rotational torque of the humeral head with the glenoid cavity. Nevertheless, other authors indicate that in order to ensure the recovery of active flexion of the arm, these tendons, if ruptured, must be repaired first before the spacer is implanted(17).
Furthermore, subsequent studies have shown that the best outcomes can be expected in those patients with an intact and/or partially reparable tendon of the infraspinatus(18).
Thus, taking into account the current literature and the recommendations of the experts, it seems that the ideal patient for placement of the subacromial spacer balloon is an individual failing to respond to conservative management, with massive rotator cuff rupture, intact tendons of the subscapularis and teres minor, a preferably reparable infraspinatus, with complete passive mobility and no glenohumeral arthropathy(18,19). Burnier et al., on the basis of a systematic review conducted in 2019, added that a low functional demand was another feature to be taken into account in defining the ideal patient for this technique(20).
In contrast, there are greater contraindications for the use of this technique in irreparable massive cuff ruptures(17). These are:
- Patients allergic to any of the components of the device.
- Active infection.
- Glenohumeral arthropathy. Patients with erosive lesions of the joint surfaces will experience persistence of the pain and limited mobility secondary to the formation of osteophytes.
- Deltoid muscle dysfunction. The deltoid muscle becomes the main elevator of the arm after placement of the subacromial balloon; it therefore must exhibit normal function in order to afford good outcomes.
- Pseudo-paralysis of the affected extremity. The poor results reported by different authors in patients with pseudo-paralytic shoulder have presently caused this latter condition to be regarded as a contraindication to the use of the technique(17,18).
The most frequently reported complications are persistent pain and displacement of the device. Reconversion to reverse shoulder replacement is the most common type of revision surgery(6,19). Ruiz Iban et al., in their series of 16 cases with a minimum follow-up of two years, reported reconversion to reverse shoulder replacement in one out of every three patients(21).
Twelve years after its introduction on the European market, there is not enough scientific evidence to confirm that the subacromial balloon is an effective treatment for dealing with irreparable massive ruptures. The study designs are very heterogeneous, and most of the publications present low level evidence (III-IV); it is therefore difficult to draw firm conclusions(22,23). For this reason, in the United Kingdom, its use has been restricted to the research setting only(19). A randomized, double-blind multicenter study has recently been published(24) reporting that arthroscopic debridement is superior to this same technique combined with use of a subacromial balloon. Thus, with high quality evidence, the authors conclude that the subacromial balloon is not an effective treatment, may prove harmful, and is not cost effective. They consequently exclude this technique as a surgical treatment option for patients with irreparable rotator cuff rupture.
Superior capsular reconstruction
The anatomical structure of the superior glenohumeral capsule was first described by Clark et al. in 1990(25), defining it as a deep extension of the coracohumeral ligament. It is a fine fibrous structure inserted in the upper part of the glenoid neck and laterally in the greater tuberosity, and may occupy the entire footprint of the tendon of the supraspinatus. It is intimately related to the "rotator cable" (defined by Burkhart et al.) or humeral semicircular ligament(26). Pouliart et al. postulated that the superior capsule plays a "safety" role in the anchoring of the rotator cable and in maintaining its function(27). Patients with massive rotator cuff rupture present a defect in the superior capsule and in the rotator cable. This results in reverse fulcrum loss and loss of joint stability, giving rise to ascent of the humeral head during abduction which, over time, leads to secondary osteoarthrotic changes.
reacae.30279.fs2301005en-figure5.png

Figure 5. A: arthroscopic view of the left shoulder. Lateral view of superior capsular reconstruction (SCR) with a graft anchored medially to the glenoid cavity and subsequently convergence knotted to the tendon of the infraspinatus; B: arthroscopic view of the left shoulder. Posterior view of SCR anchored laterally to the greater tuberosity in a knotless double row; C: schematic view of the SCR anchored medially to the glenoid cavity and laterally to the greater tuberosity.
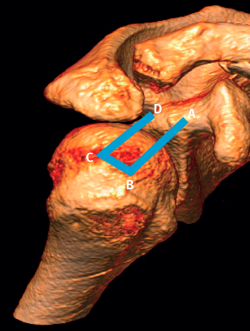
Mihata et al.(28), in a study in cadavers, postulated that reconstructing the superior capsule with a graft anchored medially in the glenoid cavity and laterally in the tuberosity would be able to restore joint stability and thus shoulder function (Figure 2).
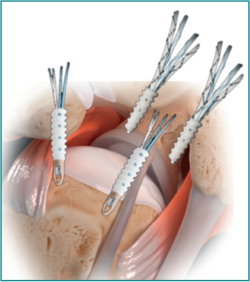
The surgical technique is performed arthroscopically(29). The first step involves extensive debridement and bursectomy of the entire subacromial space to facilitate visualization and expand the working space. Then, we place the first four implants, two at the upper level of the glenoid neck and the other two at medial level of the footprint of the supraspinatus (previously prepared) (Figure 3). This step is crucial for performing the measurements of the distances between anchorings (anterior, posterior, medial and lateral distance) and for calculation of the final size of the graft (Figure 4). Once the definitive graft has been obtained with the calculated size, and before inserting it in the subacromial space, the latter must be perforated with four orifices at a pre-established distance in order to retrieve the extremities of the implants through each of them. Then, we interconnect two ends of the medial anchorings (one end for each anchoring). At this point we insert the graft into the subacromial space, pulling on the two medial extremities that have not been interconnected, and which act as a descending pulley mechanism. To complete positioning of the graft at lateral level, a double row transosseous-equivalent (TOE) placement is carried out with two new implants - preferably knotless implants. Most surgeons perform this final fixation of the graft with the shoulder in abduction of about 10-45º(30), though despite the different studies carried out in this regard(31,32), there is not enough evidence to recommend a concrete abduction angle for fixing the graft.
The recommended last step before completing surgery is to perform convergence sutures between the graft and the tendon of the infraspinatus, since this has been suggested to favor increased stability(33) and better integration of the graft(34) - the latter being one of the most important factors for improving the middle and long term outcomes(35,36) (Figure 5).
It is indicated in those patients that present symptomatic irreparable rupture of the tendon of the supraspinatus, and where conservative management has failed and all the following characteristics are met:
- Intact tendon of the infraspinatus or with reparable damage.
- Absence or minimum presence of glenohumeral osteoarthrosis (Hamada 1 or 2)(37).
- Intact tendon of the subscapularis or with reparable damage.
- Normally functioning deltoid muscle.
- No severe osteoporosis.
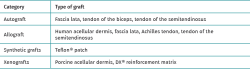
To secure improved results with the surgical technique, we must be very careful in selecting the patients, and furthermore, in this technique, the characteristics of the graft also appear to play an important role in terms of the outcomes obtained. The initial technique was described using autologous fascia lata (28), though at present there are studies that have used different heterologous acellular dermal matrix grafts, as well as different autologous grafts such as tendon of the semitendinosus, the Achilles tendon, or the long portion of the biceps (Table 1). Independently of the graft used, it should be at least 6 mm thick(30,38) in order to guarantee good middle and long term outcomes.
The studies published up until 2020, including systematic reviews(39,40,41,42,43), concluded that the SCR technique, at least over the short term, affords significant improvement in terms of strength and mobility, with the reduction of pain. Series have been published that report rates in excess of 90% of pseudo-paralysis reversion (44,45) and patient reincorporation to previous physical and working activity(46). These preliminary results, the introduction of dermal allografts, improvements of the surgical technique, etc., have caused this procedure to increase exponentially in popularity among shoulder surgeons. Some authors have referred to this popularity as being the result of pressure on the part of the industry, and of collective surgical enthusiasm(47). The fact is that to date, there have been no randomized prospective studies comparing SCR with techniques such as debridement, biceps tenotomy or partial repair. Most of the published articles can be classified as technical papers, articles on biomechanical principles, observational studies or reviews of observational studies. This lack of high level evidence has been cited as a cause underlying the decrease in the number of superior capsular reconstructions made. Other mentioned reasons are the lack of healing of the graft and the absence of patient perceived benefit capable of justifying the cost of the technique(48).
Transpositioning of the biceps for biological capsule reconstruction (bio-SCR)
As commented above, integration and healing of the graft with the receptor bone is one of the most important aspects for obtaining good outcomes with SCR over the middle and long term(35,36). Recently, a number of authors have described the use of the long portion of the biceps (LPB) as autograft in SCR(49,50,51,52). Furthermore, the use of this autograft in comparison with the initial technique of Mihata et al.(28) offers a series of advantages such as the disappearance of morbidity in the donor zone, and an apparent decrease in surgery time and the risk of infection(53). When compared with the use of allografts, xenografts and synthetic grafts, SCR with biceps transposition is a less demanding technique, and reduces the costs of surgery and the risk of transmissible diseases(54,55).
The indications of bio-SCR are basically the same as those of the conventional SCR technique, though the following is moreover needed:
- An intact tendon of the long portion of the biceps and its insertion.
- Patients with low functional or strength demands.
During the arthroscopic subacromial step of the bio-SCR technique, it is essential to confirm the integrity of the long portion of the biceps. Once this has been confirmed, we prepare the footprint. Two anchorings are placed with sutures, one at the most medial aspect of the footprint and the other at the most lateral aspect (Figure 6A). A curved soft tissue penetrating device is used to perform a loop through the long head of the biceps, with fixation to the anchoring with 4-5 knots. This first knotting step fixes the biceps in its new location, and with the second thread emerging from the anchoring we perform another knot that envelops the tendon of the long head of the biceps to secure greater fixation and stability in the insertion bed (Figure 6B). The same process is carried out with the threads of the lateral anchoring of the footprint in the greater tuberosity. Then tenotomy of the long portion of the biceps distal to the knot of the second anchoring is carried out (Figure 6C)(56).
reacae.30279.fs2301005en-figure6.png

Figure 6. Right shoulder. A: preparation of the footprint parallel to the bicipital groove and decorticating part of the more lateral cartilage of the joint; B: appearance of the biceps after performing the two types of sutures with the threads of the more medial implant; C: final view of the technique after performing the biceps tenotomy. Reproduced from the original article by Llanos-Rodríguez et al.(56).
Fandridis et al.(57) described bio-SCR with bifascicular fixation of the biceps using the box technique (Figure 7); from the anchoring in the greater tuberosity, a circular twist of the tendon is applied, inserting it again with another anchoring over the upper margin of the glenoid cavity. In order to do this, we need to use a small subpectoral approach to secure greater length with the autograft.
To date, the studies in cadavers and biomechanical models have shown that the bio-SCR technique appears to be biomechanically equivalent and potentially stronger in centering the humeral head in the glenoid cavity compared with conventional SCR(58,59). These studies suggest that the bio-SCR technique with adequate lateral fixation in the footprint appears to restore shoulder stability in irreparable massive cuff ruptures, thanks to its capacity to center the humeral head in the glenoid cavity.
Lädermann et al.(60), in a retrospective study, compared the early clinical outcomes in patients subjected to arthroscopic SCR with different types of grafts (acellular dermis versus long head of the biceps). The clinical scores in both groups were seen to improve after SCR in patients with irreparable rotator cuff ruptures, though there were fewer complications and revision surgeries with autograft versus the allograft. The authors concluded that if the long portion of the biceps is still in its place during surgery, its use seems to be valid, given the reasonable cost and the few associated complications.
Conclusions
The surgical management of patients with massive rotator cuff rupture remains a challenge. Detailed knowledge of the different therapeutic options and their indications is crucial for improving the functional outcomes in these patients. New surgical techniques have appeared in recent years, such as the subacromial balloon and SCR for the treatment of some of the patients with ruptures of this kind, though the results published to date are inconsistent and with low scientific evidence. For this reason, the authors, before recommending their generalized use, point to the need for comparative randomized prospective studies and publications with long term follow-up, demonstrating consistent good results over time, in order to help select the best technique for each individual patient, and to determine whether they will continue to play a role in the surgical management of irreparable massive cuff ruptures.
Figuras
Figure 2. Graphic representation of the end result of the subacromial balloon technique following insufflation. Image reproduced from the original article by Savarese et al.(8).
Figure 3. Graphic representation of the subacromial view from the lateral port in the right shoulder after placing the first four anchorings to perform the superior capsule reconstruction technique.
Figure 4. Figure showing the size of the final graft according to the measures taken intraoperatively, and graphic representation of the location of the four orifices in the graft according to the pre-established distance. Image provided by Arthur Rousseau.
Figure 5. A: arthroscopic view of the left shoulder. Lateral view of superior capsular reconstruction (SCR) with a graft anchored medially to the glenoid cavity and subsequently convergence knotted to the tendon of the infraspinatus; B: arthroscopic view of the left shoulder. Posterior view of SCR anchored laterally to the greater tuberosity in a knotless double row; C: schematic view of the SCR anchored medially to the glenoid cavity and laterally to the greater tuberosity.
Figure 6. Right shoulder. A: preparation of the footprint parallel to the bicipital groove and decorticating part of the more lateral cartilage of the joint; B: appearance of the biceps after performing the two types of sutures with the threads of the more medial implant; C: final view of the technique after performing the biceps tenotomy. Reproduced from the original article by Llanos-Rodríguez et al.(56).
Figure 7. In performing the bio-SCR technique with bifascicular biceps plasty, the tendon is fixed at two points in the upper part of the glenoid neck and at two points in the footprint of the greater tuberosity, generating the box configuration shown in the figure.
Tablas
Información del artículo
Cita bibliográfica
Autores
Karla Rodríguez Bascones
Servicio de Cirugía Ortopédica y Traumatología. Unidad de Artroscopia. Hospital ASEPEYO Sant Cugat. Barcelona
Unidad de Hombro y Codo. Hospital Asepeyo. Sant Cugat, Barcelona
Montserrat Castillo
Servicio de Cirugía Ortopédica y Traumatología. Unidad de Artroscopia. Hospital ASEPEYO Sant Cugat. Barcelona
Tomás Eduardo Maio
Servicio de Cirugía Ortopédica y Traumatología. Unidad de Artroscopia. Hospital ASEPEYO Sant Cugat. Barcelona
Ethical responsibilities
Conflicts of interest. The authors state that they have no conflicts of interest.
Financial support. This study has received no financial support.
Protection of people and animals. The authors declare that this research has not involved human or animal experimentation.
Data confidentiality. The authors declare that the protocols of their work centre referred to the publication of patient information have been followed.
Right to privacy and informed consent. The authors declare that no patient data appear in this article.
Referencias bibliográficas
-
1Cofield RH. Rotator cuff disease of the shoulder. J Bone Joint Surg Am. 1985 Jul;67(6):974-9.
-
2Gerber C, Fuchs B, Hodler J. The results of repair of massive tears of the rotator cuff. J Bone Joint Surg Am. 2000 Apr;82(4):505-15.
-
3Lädermann A, Denard PJ, Collin P. Massive rotator cuff tears: definition and treatment. Int Orthop. 2015 Dec;39(12):2403-14.
-
4Patte D. Classification of rotator cuff lesions. Clin Orthop Relat Res. 1990 May;(254):81-6.
-
5Goutallier D, Postel JM, Bernageau J, Lavau L, Voisin MC. Fatty muscle degeneration in cuff ruptures. Pre- and postoperative evaluation by CT scan. Clin Orthop Relat Res. 1994 Jul;(304):78-83.
-
6Srinivasan RC, Elhassan BT, Wright TW. Rotator Cuff Repair and Reconstruction. J Hand Surg Am. 2021 Jun;46(6):493-500.
-
7Di Benedetto P, Mancuso F, Tosolini L, Buttironi MM, Beltrame A, Causero A. Treatment options for massive rotator cuff tears: a narrative review. Acta Biomed. 2021 Jul 26;92(S3):e2021026.
-
8Savarese E, Romeo R. New solution for massive, irreparable rotator cuff tears: the subacromial "biodegradable spacer". Arthrosc Tech. 2012 May 4;1(1):e69-74.
-
9Striker. InSpace. Separador subacromial biodegradable. Disponible en: https://www.stryker.com/es/es/sports-medicine/products/inspace/index-eu.html.
-
10Senekovic V, Poberaj B, Kovacic L, et al. The biodegradable spacer as a novel treatment modality for massive rotator cuff tears: a prospective study with 5-year follow-up. Arch Orthop Trauma Surg. 2017 Jan;137(1):95-103.
-
11Yallapragada RK, Apostolopoulos A, Katsougrakis I, Selvan TP. The use of a subacromial spacer-inspace balloon in managing patients with irreparable rotator cuff tears. J Orthop. 2018 Aug 16;15(3):862-8. Erratum in: J Orthop. 2020 Dec 14;23:275.
-
12Lobao MH, Canham RB, Melvani RT, Abboud JA, Parks BG, Murthi AM. Biomechanics of Biodegradable Subacromial Balloon Spacer for Irreparable Superior Rotator Cuff Tears: Study of a Cadaveric Model. J Bone Joint Surg Am. 2019 Jun 5;101(11):e49.
-
13Haim Zada M, Kumar A, Elmalak O, Markovitz E, Icekson R, Domb AJ. In vitro and in vivo degradation behavior and the long-term performance of biodegradable PLCL balloon implants. Int J Pharm. 2020;574:118870.
-
14Ricci M, Vecchini E, Bonfante E, et al. A clinical and radiological study of biodegradable subacromial spacer in the treatment of massive irreparable rotator cuff tears. Acta Biomed. 2017 Oct 18;88(4S):75-80.
-
15Senekovic V, Poberaj B, Kovacic L, Mikek M, Adar E, Dekel A. Prospective clinical study of a novel biodegradable sub-acromial spacer in treatment of massive irreparable rotator cuff tears. Eur J Orthop Surg Traumatol. 2013 Apr;23(3):311-6.
-
16Ramot Y, Nyska A, Markovitz E, et al. Long-term local and systemic safety of poly(l -lactide-co-epsilon-caprolactone) after subcutaneous and intra-articular implantation in rats. Toxicol Pathol. 2015;43(8):1127-40.
-
17Horneff III JG, Abboud JA. Balloon arthroplasty: indications, technique, and European outcomes. Ann Jt. 2018;3:85-85.
-
18Wright MA, Abboud JA, Murthi AM. Subacromial Balloon Spacer Implantation. Curr Rev Musculoskelet Med. 2020 Oct;13(5):584-91.
-
19Viswanath A, Drew S. Subacromial balloon spacer - Where are we now? J Clin Orthop Trauma. 2021 Mar 26;17:223-32.
-
20Burnier M, Elhassan BT, Sánchez-Sotelo J. Surgical Management of Irreparable Rotator Cuff Tears: What Works, What Does Not, and What Is Coming. J Bone Joint Surg Am. 2019 Sep 4;101(17):1603-12.
-
21Ruiz-Ibán MA, Lorente R, Ruiz R, et al. The absorbable subacromial spacer for irreparable posterosuperior cuff tears has inconsistent results. Knee Surg Sports Traumatol Arthrosc. 2018 Dec;26(12):3848-54.
-
22Moon AS, Patel HA, Ithurburn MP, Brabston EW, Ponce BA, Momaya AM. Subacromial Spacer Implantation for the Treatment of Massive Irreparable Rotator Cuff Tears: A Systematic Review. Arthroscopy. 2019 Feb;35(2):607-14.
-
23Johns WL, Ailaney N, Lacy K, Golladay GJ, Vanderbeck J, Kalore NV. Implantable Subacromial Balloon Spacers in Patients With Massive Irreparable Rotator Cuff Tears: A Systematic Review of Clinical, Biomechanical, and Financial Implications. Arthrosc Sports Med Rehabil. 2020 Oct 16;2(6):e855-e872.
-
24Metcalfe A, Parsons H, Parsons N, et al. Subacromial balloon spacer for irreparable rotator cuff tears of the shoulder (START:REACTS): a group-sequential, double-blind, multicentre randomised controlled trial. Lancet. 2022 May 21;399(10339):1954-63.
-
25Clark J, Sidles JA, Matsen FA. The relationship of the glenohumeral joint capsule to the rotator cuff. Clin Orthop Relat Res. 1990 May;(254):29-34.
-
26Burkhart SS, Esch JC, Jolson RS. The rotator crescent and rotator cable: an anatomic description of the shoulder's "suspension bridge". Arthroscopy. 1993;9(6):611-6. Erratum in: Arthroscopy 1994 Apr;10(2):239.
-
27Pouliart N, Somers K, Eid S, et al. Variations in the superior capsuloligamentous complex and description of a new ligament. J Shoulder Elbow Surg. 2007;16:821Y36.
-
28Mihata T, McGarry MH, Pirolo JM, Kinoshita M, Lee TQ. Superior capsule reconstruction to restore superior stability in irreparable rotator cuff tears: A biomechanical cadaveric study. Am J Sports Med. 2012 Oct;40(10):2248-55.
-
29Tokish JM, Beicker C. Superior Capsule Reconstruction Technique Using an Acellular Dermal Allograft. Arthrosc Tech. 2015 Dec 23;4(6):e833-9.
-
30Mihata T, McGarry MH, Kahn T, Goldberg I, Neo M, Lee TQ. Biomechanical Effect of Thickness and Tension of Fascia Lata Graft on Glenohumeral Stability for Superior Capsule Reconstruction in Irreparable Supraspinatus Tears. Arthroscopy. 2016 Mar;32(3):418-26.
-
31Adams CR, Comer B, Scheiderer B, et al. The Effect of Glenohumeral Fixation Angle on Deltoid Function During Superior Capsule Reconstruction: A Biomechanical Investigation. Arthroscopy. 2020 Feb;36(2):400-8.
-
32Dyrna F, Berthold DP, Muench LN, et al. Graft Tensioning in Superior Capsular Reconstruction Improves Glenohumeral Joint Kinematics in Massive Irreparable Rotator Cuff Tears: A Biomechanical Study of the Influence of Superior Capsular Reconstruction on Dynamic Shoulder Abduction. Orthop J Sports Med. 2020 Oct 6;8(10):2325967120957424.
-
33Mihata T, McGarry MH, Kahn T, Goldberg I, Neo M, Lee TQ. Biomechanical Role of Capsular Continuity in Superior Capsule Reconstruction for Irreparable Tears of the Supraspinatus Tendon. Am J Sports Med. 2016 Jun;44(6):1423-30.
-
34Plachel F, Klatte-Schulz F, Minkus M, Böhm E, Moroder P, Scheibel M. Biological allograft healing after superior capsule reconstruction. J Shoulder Elbow Surg. 2018 Dec;27(12):e387-e392.
-
35Makovicka JL, Chung AS, Patel KA, Deckey DG, Hassebrock JD, Tokish JM. Superior capsule reconstruction for irreparable rotator cuff tears: a systematic review of biomechanical and clinical outcomes by graft type. J Shoulder Elbow Surg. 2020 Feb;29(2):392-401.
-
36Zastrow RK, London DA, Parsons BO, Cagle PJ. Superior Capsule Reconstruction for Irreparable Rotator Cuff Tears: A Systematic Review. Arthroscopy. 2019 Aug;35(8):2525-34.e1.
-
37Hamada K, Fukuda H, Mikasa M, Kobayashi Y. Roentgenographic findings in massive rotator cuff tears. A long-term observation. Clin Orthop Relat Res. 1990 May;(254):92-6.
-
38Scheiderer B, Kia C, Obopilwe E, et al. Biomechanical Effect of Superior Capsule Reconstruction Using a 3-mm and 6-mm Thick Acellular Dermal Allograft in a Dynamic Shoulder Model. Arthroscopy. 2020 Feb;36(2):355-64.
-
39Sochacki KR, McCulloch PC, Lintner DM, Harris JD. Superior Capsular Reconstruction for Massive Rotator Cuff Tear Leads to Significant Improvement in Range of Motion and Clinical Outcomes: A Systematic Review. Arthroscopy. 2019 Apr;35(4):1269-77.
-
40Catapano M, de Sa D, Ekhtiari S, Lin A, Bedi A, Lesniak BP. Arthroscopic Superior Capsular Reconstruction for Massive, Irreparable Rotator Cuff Tears: A Systematic Review of Modern Literature. Arthroscopy. 2019 Apr;35(4):1243-53.
-
41Gao I, Sochacki KR, Freehill MT, Sherman SL, Abrams GD. Superior Capsular Reconstruction: A Systematic Review of Surgical Techniques and Clinical Outcomes. Arthroscopy. 2021 Feb;37(2):720-46.
-
42Frank RM, Cvetanovich G, Savin D, Romeo AA. Superior Capsular Reconstruction: Indications, Techniques, and Clinical Outcomes. JBJS Rev. 2018 Jul;6(7):e10.
-
43Galvin JW, Kenney R, Curry EJ, et al. Superior Capsular Reconstruction for Massive Rotator Cuff Tears: A Critical Analysis Review. JBJS Rev. 2019 Jun;7(6):e1.
-
44Mihata T, Lee TQ, Hasegawa A, et al. Arthroscopic superior capsule reconstruction can eliminate pseudoparalysis in patients with irreparable rotator cuff tears. Am J Sports Med 2018;46:2707-16.
-
45Burkhart SS, Hartzler RU. Superior capsular reconstruction reverses profound pseudoparalysis in patients with irreparable rotator cuff tears and minimal or no glenohumeral arthritis. Arthroscopy. 2019;35:22-8.
-
46Mihata T, Lee TQ, Fukunishi K, et al. Return to Sports and Physical Work After Arthroscopic Superior Capsule Reconstruction Among Patients With Irreparable RotatorCuff Tears. Am J Sports Med. 2018;46(5):1077-83.
-
47Lädermann A, Rashid M. Superior Capsular Reconstruction-Technical Marvel or Fading Fashion? Arthroscopy. 2022 Nov;38(11):2954-6.
-
48Hankins AC, Griffin JW, Taliaferro JP, Werner BC, Bonner KF. The Number of Surgeons Using Superior Capsular Reconstruction for Rotator Cuff Repair Is Declining. Arthrosc Sports Med Rehabil. 2022 Nov 17;4(6):e2089-e2098.
-
49Boutsiadis A, Chen S, Jiang C, Lenoir H, Delsol P, Barth J. Long Head of the Biceps as a Suitable Available Local Tissue Autograft for Superior Capsular Reconstruction: "The Chinese Way". Arthrosc Tech. 2017 Oct 12;6(5):e1559-e1566.
-
50Kim YS, Lee HJ, Park I, Sung GY, Kim DJ, Kim JH. Arthroscopic In Situ Superior Capsular Reconstruction Using the Long Head of the Biceps Tendon. Arthrosc Tech. 2018 Jan 8;7(2):e97-e103.
-
51Shin SJ, Kim IW, Park I, Lee S, Kim MS. Anterior Cable Reconstruction Using the Biceps Tendon in Retracted Anterior L-Shaped Rotator Cuff Tears. Arthrosc Tech. 2020 Dec 16;10(1):e55-e60.
-
52Adrian SC, Field LD. Biceps Transposition for Biological Superior Capsular Reconstruction. Arthrosc Tech. 2020 Jun 15;9(6):e841-e846.
-
53Kim DH, Jung YS, Kim KR, Yoon JP. The best options in superior capsular reconstruction. Clin Shoulder Elb. 2021 Jun;24(2):114-21.
-
54Chiang CH, Shaw L, Chih WH, Yeh ML, Su WR. Arthroscopic Rotator Cuff Repair Combined With Modified Superior Capsule Reconstruction as Reinforcement by the Long Head of the Biceps. Arthrosc Tech. 2019 Sep 21;8(10):e1223-e1231.
-
55Adrian SC, Field LD. Biceps Transposition for Biological Superior Capsular Reconstruction. Arthrosc Tech. 2020 Jun 15;9(6):e841-e846.
-
56Llanos-Rodríguez Á, Escandón-Almazán P, Espejo-Reina A, Nogales-Zafra J, Egozgue-Folgueras R, Espejo-Baena A. Anterior Capsular Reconstruction With Proximal Biceps Tendon for Large to Massive Rotator Cuff Tears. Arthrosc Tech. 2021 Jul 21;10(8):e1965-e1971.
-
57Fandridis E, Zampeli F. Superior Capsular Reconstruction With Double Bundle of Long Head Biceps Tendon Autograft: The "Box" Technique. Arthrosc Tech. 2020 Nov 20;9(11):e1747-e1757.
-
58Han F, Kong CH, Hasan MY, Ramruttun AK, Kumar VP. Superior capsular reconstruction for irreparable supraspinatus tendon tears using the long head of biceps: A biomechanical study on cadavers. Orthop Traumatol Surg Res. 2019 Apr;105(2):257-63.
-
59El-Shaar R, Soin S, Nicandri G, Maloney M, Voloshin I. Superior Capsular Reconstruction With a Long Head of the Biceps Tendon Autograft: A Cadaveric Study. Orthop J Sports Med. 2018 Jul 19;6(7):2325967118785365.
-
60Lädermann A, Denard PJ, Barth J, et al. Superior capsular reconstruction for irreparable rotator cuff tears: Autografts versus allografts. Orthop Traumatol Surg Res. 2021 Dec;107(8S):103059.
Descargar artículo:
Licencia:
Este contenido es de acceso abierto (Open-Access) y se ha distribuido bajo los términos de la licencia Creative Commons CC BY-NC-ND (Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional) que permite usar, distribuir y reproducir en cualquier medio siempre que se citen a los autores y no se utilice para fines comerciales ni para hacer obras derivadas.
Comparte este contenido
En esta edición
- Sometimes the rotator cuff injury of the shoulder is not repairable and we will have to do something with it…
- More manuscripts!
- Teach everything, tell everything
- Irreparable massive ruptures of the posterosuperior cuff: definition, diagnosis and classification
- Conservative management with medication and other non-surgical invasive therapies
- Physiotherapy and electrophysical therapies in the conservative management of irreparable posterosuperior rotator cuff rupture
- Alternatives in irreparable ruptures of the posterosuperior cuff. Debridement, tenotomy, partial repair
- Surgical alternatives in irreparable ruptures of the posterosuperior cuff
- Tendon transfers in irreparable ruptures of the posterosuperior rotator cuff. Latissimus dorsi and lower trapezius
- Reverse replacement in a patient without osteoarthritis
- Arthroscopic surgical technique for tendon transfer of the lower trapezius
- Arthroscopy assisted latissimus dorsi transfer for irreparable posterosuperior rotator cuff injuries really works
- Instructions for authors (Sept. 2023)
Más en PUBMED
Más en Google Scholar
Más en ORCID


Revista Española de Artroscopia y Cirugía Articular está distribuida bajo una licencia de Creative Commons Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional.