Irreparable massive ruptures of the posterosuperior cuff: definition, diagnosis and classification
Roturas masivas irreparables del manguito posterosuperior: definición, diagnóstico y clasificación
Resumen:
Las roturas masivas irreparables del manguito rotador son un reto incluso para el cirujano de hombro experto. El algoritmo de diagnóstico y decisión terapéutica de este tipo de roturas es complejo y atiende a diversos factores. El principal factor para definir una rotura masiva es el tamaño de esta, aunque a lo largo del tiempo se han propuesto diferentes acepciones. La irreparabilidad de una rotura viene determinada por el grado de infiltración grasa de Goutallier, sobre todo los grados 3 y 4, la distancia acromiohumeral < 6 mm, el tamaño mediolateral de la huella de 47,4 mm y la presencia de un hombro pseudoparalítico de evolución crónica, además de otros factores secundarios como el grado de retracción de Patte de tipo 3, la edad, las enfermedades concomitantes, la actividad física y la cronicidad de la lesión. Los pacientes con roturas masivas irreparables del manguito rotador pueden estar asintomáticos, pero si manifiestan síntomas, estos suelen estar íntimamente relacionados con los tendones afectos. Una de las presentaciones posibles es el hombro pseudoparalítico, asociado a los patrones de rotura de tipo B, E y C de Collin. Una vez definida una lesión como masiva e irreparable y en relación con el tipo de déficit motor, se puede clasificar en varios grupos denominados PLEA, ILEA, ILER, CLEER o ILIR.
El objetivo de este artículo es realizar una revisión sobre el concepto de rotura masiva irreparable del manguito rotador, los métodos diagnósticos, la exploración física y su clasificación.
Abstract:
Irreparable massive rotator cuff rupture is a challenge even for expert shoulder surgeons. The diagnostic and therapeutic decision algorithm of ruptures of this kind is complex and is conditioned by a number of factors. The main factor defining massive tear or rupture is its size, though different definitions have been proposed over time. The irreparability of rupture is determined by Goutallier fatty infiltration, particularly grades 3 and 4, an acromiohumeral distance < 6 mm, a mediolateral footprint size of 47.4 mm, and the presence of a chronic pseudo-paralytic shoulder - in addition to other secondary factors such as type 3 Patte retraction, patient age, concomitant diseases, physical activity and the chronicity of the injury. Patients with irreparable massive rotator cuff rupture may be asymptomatic, but when symptoms are present, they tend to be intimately related to the affected tendons. One of the possible presentations is pseudo-paralytic shoulder, associated to Collin type B, E and C ruptures. Once the injury has been diagnosed as massive and irreparable, and considering the type of motor deficit involved, it can be classified into various groups referred to as PLEA, ILEA, ILER, CLEER or ILIR.
The present study offers a review of the concept of irreparable massive rotator cuff rupture, the diagnostic methods, physical examination and classification.
Introduction
Rotator cuff tears or ruptures are among the most common musculoskeletal injuries, with a prevalence of 20% in the general population(1). Larger lesions are associated to poorer functional outcomes and greater postoperative structural failure rates(2,3). Of all rotator cuff ruptures, approximately 20% are massive ruptures(2) that pose a challenge due to their high re-rupture rate of between 18-94%, and their potential irreparability(4).
But what is massive rotator cuff rupture, and what are the criteria for considering it to be irreparable? The truth is that both terms have evolved over time, and although they are intimately related, they are not synonymous. While most irreparable ruptures are massive, some are not. In contrast, many massive ruptures are reparable despite the fact that the term "massive" has connotations of repair difficulty(5).
Many factors need to be taken into account for both the diagnosis and treatment of irreparable massive rupture (IMR) of the rotator cuff, such as the size of rupture, its retraction, the affected tendons and the exploratory findings in relation to them, the degree of adipose or fatty infiltration, the presence or not of degenerative joint findings, the age of the patient, and the physical demands.
The present study offers a review of the concept of IMR of the rotator cuff, with special attention to those lesions that affect the posterosuperior (supraspinatus-infraspinatus) cuff, their classification, and the typical physical exploratory findings.
Definition and diagnostic tests
Massive ruptures
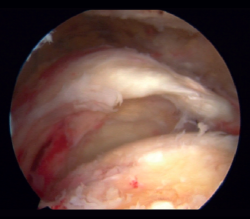
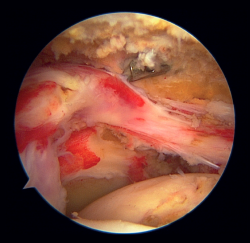
Different definitions of massive rupture of the rotator cuff (MRRC) have been proposed over time. Cofield defined them as lesions measuring 5 cm or more in diameter(6), while according to Gerber et al.(7) they involve the complete deinsertion of two or more tendons, exposing the tuberosities - a circumstance easily identifiable during surgery (Figure 1). On the other hand, Davidson and Burkhart(8) defined such lesions as retracted ruptures measuring at least 2 cm in length in the sagittal plane and with a width of 2 cm in the coronal plane - being identifiable preoperatively by means of magnetic resonance imaging (MRI). However, these definitions may result in bias due to differences in size between patients or the position of the arm at the time of measurement, and they moreover fail to distinguish between different patterns of rupture and do not predict function of the injured shoulder. Accordingly, Ladërmann et al.(9) considered that in addition to the number of damaged tendons, at least one of the two must be retracted more medial to the humeral head - this corresponding to supraspinatus grade 3 retraction in the coronal plane according to the classification of Patte(10), which adds more objective three-dimensional value to the measurement (Figure 2). Lastly, Schumaier et al., involving a group of experts, recently published a consensus document defining massive ruptures as those that are retracted to the margin of the glenoid cavity in the coronal or axial plane and/or present exposure of two-thirds of the greater tuberosity footprint in the sagittal plane(11).
Once MRRC has been identified, it can be subclassified according to the classification of Collin et al.(12), which divides the rotator cuff into 5 components: inferior subscapularis, superior subscapularis, supraspinatus, infraspinatus and teres minor, ordered from anterior to posterior. In relation to these components, rotator cuff ruptures are classified into 5 types:
- Type A: injuries of the supraspinatus and superior subscapularis.
- Type B: injuries of the supraspinatus and entire subscapularis.
- Type C: injuries of the supraspinatus, superior subscapularis and infraspinatus.
- Type D: injuries of the supraspinatus and infraspinatus.
- Type E: injuries of the supraspinatus.
This classification, which is a novelty due to its anatomical division into 5 parts, not only classifies massive ruptures in relation to the damaged parts but also in relation to shoulder function - specifically active elevation, which is a concept we will examine in the section on exploration.
Irreparable ruptures
The concept of MRRC irreparability remains controversial, and given the important technological advances in relation to implants, suture resistance, interval slide techniques(13) and techniques for fixation and load distribution in repair(14,15), the term "irreparable" is still evolving. In addition, the possibility of correct repair does not necessarily imply correct healing or functional improvement of the shoulder. Hence, the making of decisions in relation to MRRC is extremely arduous and complex, and requires many factors to be taken into account - making it difficult to predict the reparability of rupture.
The most determining prognostic factor in the therapeutic algorithm is the degree of fatty infiltration of the muscle bellies as postulated by Goutallier et al.(16). This classification assesses the degree of fatty infiltration from a computed axial tomography (CAT) axial scan of the shoulder. Grade 0 corresponds to the absence of fatty infiltration. Grade 1 is characterized by small adipose inclusions. Grade 2 still presents more muscle than adipose tissue, while in Grade 3 both components are present in equal proportions (50%). Lastly, Grade 4 is characterized by the presence of more fat than muscle. Grades 3 and 4 show the poorest prognosis, though the repair of MRRC with grade 2 and 3 fatty infiltration and a supraspinatus tendon length of less than 15 mm exhibit a failure rate of up to 92%. However, if the length of remaining tendon is over 15 mm, the failure rate drops to 33%. In this respect, Meyer et al.(17) concluded that the combination of the classification of Goutallier with the size of the tendon stump appears to be a powerful predictor of MRRC reparability.
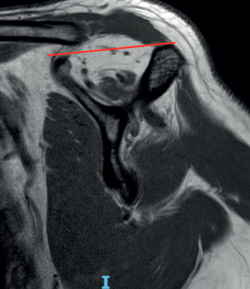
The fish backbone sign(18), in which the muscle belly presents a veined or streaky pattern reminiscent of a fish backbone, is another indicator of fatty infiltration of the muscle belly in the axial axis of the CAT scan, and is equivalent to Goutallier grade 3. The classification of Goutallier has been validated in MRI, and measurement is made in the sagittal section where the scapular spine comes into contact with the body of the scapula, producing a "Y" shaped image(19). Another predictor of irreparability and also an indicator of advanced fatty infiltration is the tangent sign of Zanetti et al.(20). According to the authors, advanced fatty infiltration is present when on tracing a line from the upper margin of the coracoid process to the upper margin of the scapular spine in the same sagittal section of an MRI scan in which a "Y" image is obtained, there is no cut in the muscle volume of the supraspinatus (Figure 3). When measuring in the sagittal view of an MRI scan, we must take into account that a healthy muscle presenting some retraction may simulate greater than real fatty infiltration, and conversely, the muscle may seem normal postoperatively, suggesting that the fatty infiltration has reverted, when in fact it is only healthy but retracted muscle. Fatty infiltration is irreversible and progressive, and although minor improvements have been observed after the repair of these tendons(21), the results are generally poorer than in situations of low grades of adipose atrophy, especially of the infraspinatus(22). Thus, one of the aims of early repair (within 2.5 years from symptoms onset) of rotator cuff injuries is to prevent the condition from progressing to higher grades of adipose atrophy associated with irreversible loss of function and the concept to irreparability(23).
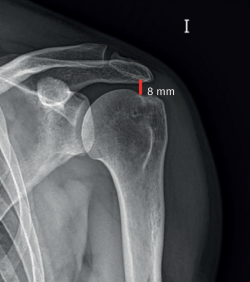
Another indicator of irreparability is the acromiohumeral distance (AHD). This is measured according to the classification proposed by Hamada et al. in 1990(24) (and modified in 2011)(25) for MRRC based on an anteroposterior plain radiograph of the shoulder, comprising 5 grades: in grade 1, AHD measures 6 mm or more (Figure 4); in grade 2 it narrows and measures 5 mm or less; in grade 3 acetabularization of the acromion is observed secondary to ascent of the humeral head; grade 4 is subdivided into grade 4A with narrowing of the glenohumeral joint space without acetabularization of the acromion and grade 4B with acetabularization; and lastly grade 5 consists of humeral head collapse. An AHD of less than 6 mm is considered to be an independent predictor or irreparability. Thus, those cases of MRRC corresponding to Hamada grade 2 or higher are considered to be irreparable.
The mediolateral magnitude of the rupture has also been postulated as an independent irreparability factor. Thus, ruptures with a mediolateral size of 47.4 mm were considered to be irreparable in a sample of 758 patients subjected to multivariate logistic regression analysis(26). In this same study, those lesions jointly affecting the supraspinatus, infraspinatus and subscapularis were also regarded as irreparable.
The degree of tendon retraction is not an irreparability indicator in itself. In this sense, it is important to take into account that L-shape or inverted L-shape ruptures may present a greater than real mediolateral size in some coronal MRI sections, simulating retraction grade 3 of the Patte classification, when in fact their true size is smaller and they may be reducible and reparable(27) - as can also occur with large retracted ruptures produced in the context of acute trauma(28).
Chronic pseudo-paralysis (with no recent acute event) is also an independent indicator of irreparability(26), with the pseudo-paralytic shoulder being understood as a shoulder with an elevation in active flexion < 90°, with complete passive joint balance, no neurological involvement and not caused by pain but characterized by genuine functional involvement (Figure 5)(12). The pseudo-paralytic shoulder is one of the possible manifestations of MRRC and will be addressed in the section on physical examination.
The age of the patient, physical activity, the time from onset of the lesion and concomitant conditions such as diabetes or smoking, are secondary factors which along with those described above must be taken into account in the decision making algorithm(5).
Physical examination and classification
Clinically, patients with MRRC may be asymptomatic(5). This is because the torque between the non-injured rotator cuff, the deltoid muscle and the rest of the periscapular muscles is balanced. In other words, despite the damage, the rotator cuff is able to exert compression force between the humeral head and the glenoid cavity, thus generating a stable fulcrum on which the deltoid muscle and the periscapular muscles are able to displace the humeral head with respect to the glenoid cavity(9).
This is possible thanks to the rotator cable, which is a thickening of the cuff acting as protection of the critical zone of this front to traction. It has been compared with a suspension bridge that distributes the forces among the supporting pillars and which, in the case of the rotator cuff, would be its anterior and posterior insertion(29). The more anterior insertion of the rotator cable divides around the bicipital groove, and its posterior pillar comprises the 50% lower portion of the insertion of the infraspinatus, which would explain why patients with ruptures of the rotator cuff between these pillars are able to maintain good active joint balance (30) and why even partial repairs of the rotator cuff achieve good functional outcomes(31).
When patients with MRRC present symptoms, they often experience typically nocturnal pain and pain with activities requiring them to raise the arm above head level, though the severity of pain is not related to lesion grade(32). The functional deficits that we can identify at physical examination are correlated to the location of the lesion. Consequently, those patients with complete subscapularis injuries will produce positive belly-press(33) and lift off(34) tests and a positive lift off lag sign(35). Supraspinatus insufficiency, present in all massive ruptures according to Collin et al.(12), is normally associated to positive Jobe(36) and drop arm(37) maneuvers, with a decrease in external rotation strength with the elbow in approximation(9). Damage to the posterosuperior cuff is usually associated with a positive external rotation lag sign, which has high sensitivity and specificity(38). The horn blower sign, which implies that the patient cannot maintain external rotation with the shoulder in 90° abduction, offers high sensitivity and specificity in diagnosing posterosuperior cuff lesions that affect the tendon of the teres minor muscle(39).
Asymptomatic patients in the context of MRRC, apart from all the already mentioned tests, and due to involvement of the rotator cable, with the consequent impossibility of compensating torque, may present a pseudo-paralytic shoulder which - as already described - is characterized by elevation in active flexion of < 90º in the absence of neurological damage and stiffness. If doubts arise during exploration as to whether the functional limitation is caused by pain, we can resort to a subacromial anesthetic test as a diagnostic strategy, where a genuine pseudo-paralytic shoulder would continue to present an elevation defect(40). It must be commented that the term pseudo-paralysis has still not been fully defined, for although the most widely accepted definition is that already mentioned above, some authors limit the term to shoulders with completely abolished active elevation, while others consider an elevation of less than 45º, always in the context of chronicity(41). In contrast, thanks to the study published by Collin et al.(12), we do know that the rupture patterns most associated with pseudo-paralysis are B (involvement of the supraspinatus + complete subscapularis with 80% pseudo-paralysis), C (superior subscapularis + supraspinatus + infraspinatus with 45% pseudo-paralysis) and E (supraspinatus + infraspinatus + teres minor with 30% pseudo-paralysis).
In 2018, Boileau et al.(42) established a classification of shoulders with MRRC according to their functional imbalance:
- Group I or PLEA (painful loss of elevation [active]): loss of active elevation due to pain. This is not a pseudo-paralytic shoulder, because the pain subsides with a subacromial anesthetic test, and muscle balance is preserved.
- Group II or ILEA (isolated loss of elevation [active]): pseudo-paralytic shoulder with loss of elevation due to imbalanced torque.
- Group III or ILER (isolated loss of external rotation): this is not pseudo-paralysis as such, since there is only loss of external rotation due to horizontal alteration of muscle balance.
- Group IV or CLEER (combined loss of active elevation and external rotation): pseudo-paralytic shoulder with deficit of both active elevation and external rotation. It is divided into two types:
- CLEER 1: deficit of both movements, fundamentally deficit of active elevation, with some preservation of external rotation.
- CLEER 2: abolished active elevation and external rotation.
In this classification, the authors assigned a treatment option of choice to each group; this will not be addressed here, however, as it falls outside the scope of this monographic article.
Another term, CLEIR, introduced by Kany et al.(43), involves the presence of a pseudo-paralytic shoulder with combined active elevation and external rotation deficit and Goutallier grade III atrophy.
Conclusions
Although the terms massive rupture and irreparable rupture are sometimes used indistinctly, they are not synonymous, and their definition has evolved over time. The most widely accepted definition refers to massive ruptures as those that are retracted to the margin of the glenoid cavity in the coronal or axial plane and/or present exposure of two-thirds of the greater tuberosity footprint in the sagittal plane. The most determining factor defining irreparability is the degree of fatty infiltration of the muscle belly according to the classification of Goutallier, with grades 3 and 4 presenting the poorest prognosis. Other factors that must be taken into account in defining rupture irreparability are an acromiohumeral distance < 6 mm, mediolateral rupture size 47.4 mm, Patte retraction grade 3, combined involvement of the supraspinatus, infraspinatus and subscapularis, and pseudo-paralytic shoulder in the absence of an acute event.
Patients with irreparable massive cuff rupture may remain asymptomatic provided the shoulder presents a balanced torque. If symptoms are present, the functional deficits are related to the damaged tendon structures. One possible manifestation is pseudo-paralytic shoulder, which is most often seen in Collin type B, C and E ruptures. Lastly, cases of irreparable massive rotator cuff rupture are classified into 5 groups according to the deficit involved: PLEA, ILEA, ILER, CLEER and CLEIR.
Figuras
Figure 3. Tangent sign of Zanetti with no cut in the volume of the supraspinatus in the parasagittal MRI view, where the coracoid process and scapular spine are identified.
Información del artículo
Cita bibliográfica
Autores
Santos Moros Marco
Servicio de Traumatología. Hospital MAZ. Zaragoza
Cirugía Ortopédica y Traumatología. Unidad de Miembro Superior. Hospital MAZ Zaragoza. Arthrosport Zaragoza
Editor asociado de REACA
Servicio de Traumatología y Cirugía Ortopédica. Hospital de la Mutua MAZ. Zaragoza
Jorge Díaz Heredia
Cirugía Ortopédica y Traumatología. Unidad de Hombro y Codo. Hospital Universitario Ramón y Cajal. Madrid
Clínica La Antigua. Guadalajara
Editor asociado de REACA
Gabriel del Monte Bello
Unidad de Hombro y Codo. Hospital Fraternidad-Muprespa. Madrid
Hospital Quirón Juan Bravo. Madrid
Hospital Monográfico Asepeyo. Coslada, Madrid
Ethical responsibilities
Conflicts of interest. The authors state that they have no conflicts of interest.
Financial support. This study has received no financial support.
Protection of people and animals. The authors declare that this research has not involved human or animal experimentation.
Data confidentiality. The authors declare that the protocols of their work centre referred to the publication of patient information have been followed.
Right to privacy and informed consent. The authors declare that no patient data appear in this article.
Referencias bibliográficas
-
1Yamamoto A, Takagishi K, Osawa T, et al. Prevalence and risk factors of a rotator cuff tear in the general population. J Shoulder Elb Surg. 2010;19:116-20.
-
2Kluger R, Bock P, Mittlböck M, Krampla W, Engel A. Long-term survivorship of rotator cuff repairs using ultrasound and magnetic resonance imaging analysis. Am J Sports Med 2011;39:2071-81.
-
3Rashid MS, Cooper C, Cook J, et al. Increasing age and tear size reduce rotator cuff repair healing rate at 1 year: data from a large randomized controlled trial. Acta Orthop. 2017;88:606-11.
-
4Schumaier A, Kovacevic D, Schmidt C, et al. Defining massive rotator cuff tears: a Delphi consensus study. J Shoulder Elbow Surg. 2020;29:674-80.
-
5Kucirek NK, Hung NJ, Wong SE. Treatment Options for Massive Irreparable Rotator Cuff Tears. Curr Rev Musculoskelet Med. 2021 Oct;14(5):304-15.
-
6Cofield RH. Subscapular muscle transposition for repair of chronic rotator cuff tears. Surg Gynecol Obstet. 1982 May;154(5):667-72.
-
7Gerber C, Fuchs B, Hodler J. The results of repair of massive tears of the rotator cuff. J Bone Joint Surg Am. 2000 Apr;82(4):505-15.
-
8Davidson J, Burkhart SS. The geometric classification of rotator cuff tears: a system linking tear pattern to treatment and prognosis. Arthroscopy. 2010;26:417-24.
-
9Lädermann A, Denard PJ, Collin P. Massive rotator cuff tears: definition and treatment. Int Orthop. 2015 Dec;39(12):2403-14.
-
10Patte D. Classification of rotator cuff lesions. Clin Orthop Relat Res. 1990 May;(254):81-6.
-
11Schumaier A, Kovacevic D, Schmidt C, et al. Defining massive rotator cuff tears: a Delphi consensus study. J Shoulder Elbow Surg. 2020 Apr;29(4):674-80.
-
12Collin P, Matsumura N, Lädermann A, Denard PJ, Walch G. Relationship between massive chronic rotator cuff tear pattern and loss of active shoulder range of motion. J Shoulder Elbow Surg. 2014;23(8):1195-202.
-
13Lo IK, Burkhart SS. Arthroscopic repair of massive, contracted, immobile rotator cuff tears using single and double interval slides: technique and preliminary results. Arthroscopy. 2004 Jan;20(1):22-33.
-
14Burkhart SS, Denard PJ, Konicek J, Hanypsiak BT. Biomechanical validation of load-sharing rip-stop fixation for the repair of tissue-deficient rotator cuff tears. Am J Sports Med. 2014 Feb;42(2):457-62.
-
15Neeley RA, Diaz MA, Gorman RA 2nd, Frankle MA, Mighell MA. A Weaving Rip-Stop Technique Leads to a Significantly Increased Load to Failure and Reduction in Suture-Tendon Cut-Through in a Biomechanical Model of Rotator Cuff Repair. Arthrosc Sports Med Rehabil. 2021 Aug 6;3(5):e1263-e1272.
-
16Goutallier D, Postel JM, Bernageau J, Lavau L, Voisin MC. Fatty muscle degeneration in cuff ruptures. Pre- and postoperative evaluation by CT scan. Clin Orthop Relat Res. 1994 Jul;(304):78-83.
-
17Meyer DC, Farshad M, Amacker NA, Gerber C, Wieser K. Quantitative analysis of muscle and tendon retraction in chronic rotator cuff tears. Am J Sports Med. 2012 Mar;40(3):606-10.
-
18Williams MD, Lädermann A, Melis B, Barthelemy R, Walch G. Fatty infiltration of the supraspinatus: a reliability study. J Shoulder Elbow Surg. 2009 Jul-Aug;18(4):581-7.
-
19Fuchs B, Weishaupt D, Zanetti M, Hodler J, Gerber C. Fatty degeneration of the muscles of the rotator cuff: assessment by computed tomography versus magnetic resonance imaging. J Shoulder Elbow Surg. 1999 Nov-Dec;8(6):599-605.
-
20Zanetti M, Gerber C, Hodler J. Quantitative assessment of the muscles of the rotator cuff with magnetic resonance imaging. Invest Radiol. 1998 Mar;33(3):163-70.
-
21Kuzel BR, Grindel S, Papandrea R, Ziegler D. Fatty infiltration and rotator cuff atrophy. J Am Acad Orthop Surg. 2013 Oct;21(10):613-23.
-
22Gladstone JN, Bishop JY, Lo IK, Flatow EL. Fatty infiltration and atrophy of the rotator cuff do not improve after rotator cuff repair and correlate with poor functional outcome. Am J Sports Med. 2007 May;35(5):719-28.
-
23Melis B, Wall B, Walch G. Natural history of infraspinatus fatty infiltration in rotator cuff tears. J Shoulder Elbow Surg. 2010 Jul;19(5):757-63.
-
24Hamada K, Fukuda H, Mikasa M, Kobayashi Y. Roentgenographic findings in massive rotator cuff tears. A long-term observation. Clin Orthop Relat Res. 1990 May;(254):92-6.
-
25Hamada K, Yamanaka K, Uchiyama Y, Mikasa T, Mikasa M. A radiographic classification of massive rotator cuff tear arthritis. Clin Orthop Relat Res. 2011 Sep;469(9):2452-60.
-
26Kim IB, Jung DW, Suh KT. Prediction of the irreparability of rotator cuff tears. Arthroscopy. 2018;34:2076-84.
-
27Eichinger JK. Editorial commentary: Look more closely at those coronal magnetic resonance imaging cuts before concluding a rotator cuff tendon tear is irreparable-don’t let an L-shaped tear fool you. Arthroscopy. 2020;36:2831.
-
28Guo S, Zhu Y, Song G, Jiang C. Assessment of tendon retraction in large to massive rotator cuff tears: a modified patte classification based on 2 coronal sections on preoperative magnetic resonance imaging with higher specificity on predicting reparability. Arthroscopy. 2020;36:2822-30.
-
29Burkhart SS, Esch JC, Jolson RS. The rotator crescent and rotator cable: an anatomic description of the shoulder’s “suspension bridge”. Arthroscopy. 1993;9(6):611-6.
-
30Huri G, Kaymakoglu M, Garbis N. Rotator cable and rotator interval: anatomy, biomechanics and clinical importance. EFORT Open Rev. 2019 Feb 20;4(2):56-62.
-
31Burkhart SS, Nottage WM, Ogilvie-Harris DJ, Kohn HS, Pachelli A. Partial repair of irreparable rotator cuff tears. Arthroscopy. 1994 Aug;10(4):363-70.
-
32Dunn WR, Kuhn JE, Sanders R, et al. Symptoms of pain do not correlate with rotator cuff tear severity. J Bone Joint Surg Am. 2014;96:793-800.
-
33Gerber C, Hersche O, Farron A. Isolated rupture of the subscapularis tendon. J Bone Joint Surg Am. 1996 Jul;78(7):1015-23.
-
34Gerber C, Krushell RJ. Isolated rupture of the tendon of the subscapularis muscle. Clinical features in 16 cases. J Bone Joint Surg Br. 1991 May;73(3):389-94.
-
35Hertel R, Ballmer FT, Lombert SM, Gerber C. Lag signs in the diagnosis of rotator cuff rupture. J Shoulder Elbow Surg. 1996 Jul-Aug;5(4):307-13.
-
36Jobe FW, Jobe CM. Painful athletic injuries of the shoulder. Clin Orthop Relat Res. 1983;173:117-24.
-
37Park HB, Yokota A, Gill HS, El Rassi G, McFarland EG. Diagnostic accuracy of clinical tests for the different degrees of subacromial impingement syndrome. J Bone Joint Surg Am. 2005;87:1446-55.
-
38Castoldi F, Blonna D, Hertel R. External rotation lag sign revisited: accuracy for diagnosis of full thickness supraspinatus tear. J Shoulder Elbow Surg. 2009;18:529-34.
-
39Walch G, Boulahia A, Calderone S, Robinson AH. The ‘dropping’ and ‘hornblower’s’ signs in evaluation of rotator-cuff tears. J Bone Joint Surg Br. 1998;80:624-8.
-
40Tokish JM, Alexander TC, Kissenberth MJ, Hawkins RJ. Pseudoparalysis: a systematic review of term definitions, treatment approaches, and outcomes of management techniques. J Shoulder Elbow Surg. 2017 Jun;26(6):e177-e187.
-
41Burks RT, Tashjian RZ. Should we have a better definition of pseudoparalysis in patients with rotator cuff tears? Arthroscopy. 2017;33:2281-3.
-
42Boileau P, Baba M, McClelland WB Jr, Thélu CÉ, Trojani C, Bronsard N. Isolated loss of active external rotation: a distinct entity and results of L'Episcopo tendon transfer. J Shoulder Elbow Surg. 2018 Mar;27(3):499-509.
-
43Kany J, Anis H, Werthel JD. Massive irreparable rotator cuff tears. Obere Extrem. 2018;13:246-54.
Descargar artículo:
Licencia:
Este contenido es de acceso abierto (Open-Access) y se ha distribuido bajo los términos de la licencia Creative Commons CC BY-NC-ND (Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional) que permite usar, distribuir y reproducir en cualquier medio siempre que se citen a los autores y no se utilice para fines comerciales ni para hacer obras derivadas.
Comparte este contenido
En esta edición
- Sometimes the rotator cuff injury of the shoulder is not repairable and we will have to do something with it…
- More manuscripts!
- Teach everything, tell everything
- Irreparable massive ruptures of the posterosuperior cuff: definition, diagnosis and classification
- Conservative management with medication and other non-surgical invasive therapies
- Physiotherapy and electrophysical therapies in the conservative management of irreparable posterosuperior rotator cuff rupture
- Alternatives in irreparable ruptures of the posterosuperior cuff. Debridement, tenotomy, partial repair
- Surgical alternatives in irreparable ruptures of the posterosuperior cuff
- Tendon transfers in irreparable ruptures of the posterosuperior rotator cuff. Latissimus dorsi and lower trapezius
- Reverse replacement in a patient without osteoarthritis
- Arthroscopic surgical technique for tendon transfer of the lower trapezius
- Arthroscopy assisted latissimus dorsi transfer for irreparable posterosuperior rotator cuff injuries really works
- Instructions for authors (Sept. 2023)
Más en PUBMED
Más en Google Scholar
Más en ORCID


Revista Española de Artroscopia y Cirugía Articular está distribuida bajo una licencia de Creative Commons Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional.