The cortical double button fixation system with posterior guide for anterior arthroscopic bone block allows precise graft positioning
El sistema de fijación de doble botón cortical con guía posterior para bloque óseo artroscópico anterior logra posiciones precisas del injerto
Resumen:
Objetivo: evaluar la posición del injerto óseo en pacientes con inestabilidad glenohumeral anteroinferior intervenidos con un sistema de fijación de doble botón cortical con guía posterior para bloque óseo artroscópico anterior.
Método: estudio longitudinal prospectivo, multicéntrico, de pacientes con inestabilidad glenohumeral anteroinferior y defecto óseo glenoideo, operados mediante la técnica de bloque óseo artroscópico con injerto de cresta ilíaca, autólogo o alogénico, estabilizado mediante sistema de doble botón. Se analizó mediante tomografía computarizada (TC) 2D la posición del injerto en el plano axial, estimando la cantidad de injerto medial o lateral a la superficie articular glenoidea. La posición craneocaudal se evaluó en el plano sagital estimando la cantidad de defecto óseo glenoideo cubierto por el injerto.
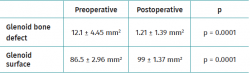
Resultados: se estudió una serie de casos consecutiva de 25 pacientes (25 hombres; edad media: 29,6 ± 8,74 años). La TC postoperatoria se realizó a los 2,77 ± 3,33 meses de la cirugía. En el plano sagital, el 80% (20/25) de los injertos se encontraban bien posicionados. En el plano axial, el 92% de los injertos se encontraban en línea, un injerto (4%) lateral y uno (4%) medial. El total de pacientes con una ubicación perfecta tanto en el plano sagital como en el axial fue del 72% (18/25). El defecto óseo glenoideo pasó de 12,1 ± 4,45 mm2 preoperatorio a 1,21 ± 1,39 mm2 postoperatorio (p = 0,0001). Esto implicó la restauración de la totalidad de la superficie de la glena en el 68% (17/25) de los pacientes.
Conclusiones: mediante un sistema de fijación de doble botón cortical con guía posterior para bloque óseo artroscópico anterior se logran posiciones precisas del injerto tanto a nivel axial como craneocaudal.
Nivel de evidencia: IV (serie de casos clínicos).
Relevancia clínica: el éxito de los procedimientos de bloque óseo depende de la correcta ubicación del injerto. Mediante el procedimiento de bloque óseo artroscópico se logran posiciones precisas del injerto tanto en el eje craneocaudal como en el eje mediolateral, con lo que se podrían recudir algunas de las complicaciones atribuidas a estos procedimientos como son la degeneración artrósica o la recidiva de la luxación.
Abstract:
Objective: to evaluate bone graft positioning in patients with anteroinferior glenohumeral instability operated upon using a cortical double button fixation system with posterior guide for anterior arthroscopic bone block.
Method: a prospective, longitudinal multicentre study was made in patients with anteroinferior glenohumeral instability and glenoid bone defects operated upon using the arthroscopic bone block technique with autologous or allogenic iliac crest grafts subjected to double button stabilisation. Two-dimensional computed tomography (CT) was used to analyse the position of the graft in the axial plane, estimating the amount of graft medial or lateral to the glenoid joint surface. The craniocaudal position was evaluated in the sagittal plane, estimating the amount of glenoid bone defect covered by the graft.
Results: a consecutive series of 25 patients was studied (25 men; mean age: 29.6 ± 8.74 years). The postoperative CT study was made 2.77 ± 3.33 months after surgery. In the sagittal plane, 80% of the grafts (20/25) were well positioned. In the axial plane, 92% of the grafts were in line, one graft (4%) was positioned lateral, and another (4%) medial. Overall, the proportion of patients with perfect positioning in both the sagittal and the axial plane was 72% (18/25). The glenoid bone defect decreased from 12.1 ± 4.45 mm2 before surgery to 1.21 ± 1.39 mm2 postoperatively (p = 0.0001). This represented complete glenoid surface restoration in 68% of the patients (17/25).
Conclusions: the cortical double button fixation system with posterior guide for anterior arthroscopic bone block allows precise graft positioning at both axial and craniocaudal level.
Level of evidence: IV (clinical case series).
Clinical relevance: the success of bone block procedures depends on correct positioning of the graft. The arthroscopic bone block procedure allows precise graft positioning in both the craniocaudal and the mediolateral axis. This could reduce some of the complications attributed to these procedures, such as degenerative arthritis or dislocation relapse.
Introduction
In up to 90% of all cases, glenohumeral instability is associated to anteroinferior glenoid bone defects(1). As a result, the arc of the glenoid joint is reduced, increasing the risk of dislocation recurrence. These bone defects are therefore considered to be one of the main risk factors for dislocation recurrence and in many cases constitute the cause of failure of the soft tissue repair techniques(2,3). Although there is no agreement on the bone defect size required to indicate repair, anteroinferior glenoid cavity reconstruction techniques using bone grafts are usually indicated from bone defects of 10%(4).
Many techniques have been described for restoring the glenoid joint surface and arc, based on the placement of a bone graft anterior to the glenoid defect. Different types of grafts have been used for this purpose, from autologous coracoid bone in the Latarjet procedure to free bone grafts. The success of these procedures largely depends on correct positioning of the bone graft in relation to the glenoid joint surface(5). Positioning too medial may result in recurrence of the instability(6), while a lateral position increases the risk of degenerative changes of the glenohumeral joint(7). The craniocaudal position of the graft is also important; higher graft positioning is associated with an increased incidence of instability relapse and a greater risk of neurological damage on inserting the screws(8). In contrast, it has been postulated that lower graft positioning may lead to mechanical failure and a lack of bone joining(9).
The present study employed computed tomography (CT) to evaluate the precision of iliac crest bone graft positioning at the anterior border of the glenoid cavity using an arthroscopic bone block placing system with a posterior guide and cortical double button. The null hypothesis was that this technique is not effective in restoring the glenoid joint surface with precise graft positioning.
Material and methods
A prospective, longitudinal multicentre study was made in a series of patients with anteroinferior glenohumeral instability and glenoid bone defects operated upon between 2016-2020 using the arthroscopic bone block technique with autologous or allogenic iliac crest grafts subjected to double button stabilisation (Smith & Nephew Inc., Andover, MA, USA).
The study was approved by the Ethics Committee of Hospital Universitario Ramón y Cajal (Madrid, Spain) (26/10/20, Minutes 400). Informed consent was obtained from all the patients.
Patients
We included all patients with recurrent anteroinferior shoulder instability requiring surgical treatment via the arthroscopic bone block positioning system with a posterior guide and cortical double button using autologous or allogenic iliac crest grafts. The patients were operated upon in four hospital centres by three different surgeons, and all of them met the inclusion criteria and none of the exclusion criteria.
The inclusion criteria were: 1) age over 18 years old; 2) recurrent anteroinferior shoulder instability; 3) glenoid defect > 5% assessed according to the Pico area measurement system in two-dimensional (2D) CT(10); and 4) good soft tissue condition as evaluated intraoperatively.
The exclusion criteria were: 1) a first dislocation episode or absence of clear dislocation episodes; 2) previous surgery involving glenoid grafting of the mentioned joint; and 3) a glenoid bone defect > 20% as assessed according to the Pico area measurement system in 2D-CT(10).
Surgical technique
The surgical technique reproduces that presented by Taverna et al. in 2014(11). The technique has been described in detail elsewhere, but is summarised here.
Preparation of the graft (fresh frozen allogenic or autologous) is carried out in a first step; the type of graft used depends on the preferences of each surgeon. Sizing to 20 × 10 × 10 mm is carried out, and two orifices spaced 10 mm apart are made on the graft at 5 mm from each end, with placement of the cortical buttons anterior to it. The patient is placed in lateral decubitus for the arthroscopic procedure. A complete arthroscopic exploration is made through three standard portals, and the lesions are identified. The anteroinferior capsulolabral complex is deinserted from the neck of the glenoid cavity from the 2 to the 6 o'clock position in the case of the right shoulder, taking special care to maintain the circumferential continuity of the labrum. The glenoid defect is drilled and freshened to leave it smooth and perpendicular to the joint plane. Using a posterior glenoid guide, two transglenoid cannulas are inserted from posterior to anterior, and the threads attached to the graft and the anterior buttons are passed through them. By exerting traction upon these threads, the graft is introduced in the joint through the rotator interval and is positioned in line with the defect. The posterior buttons are passed over the threads and are affixed tightening both sutures to 100 N. Posteriorly, we repair the capsulolabral complex over the graft (leaving the graft at extraarticular level) with glenoid implants and, in the presence of an engaging Hill-Sachs lesion, a remplissage procedure is carried out(12).
Following surgery, the patients carry an abduction sling during four weeks, allowing active exercises of the elbow and hand, and passive shoulder flexion exercises from the first day. From four weeks, progressive withdrawal of the sling is allowed, and assisted active mobility exercises are started. Free mobility is permitted after 9 weeks. After 12 weeks, strengthening exercises are started, focused on the recovery of normal scapulothoracic kinetics. Contact sports are not allowed until 6 months after surgery.
Clinical and radiological evaluation
The patient epidemiological and clinical data were collected before surgery. The intraoperative complications were recorded.
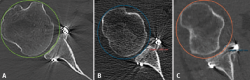
reacae.28474.fs2103006en-figure1.png

Figure 1. Estimation of glenoid axis and height according to the method of Barth(13). Two circumferences are traced: one lower, taking the posteroinferior glenoid border as reference, and one higher than the other and tangential to the glenoid borders. The line joining the centre of both circumferences is taken to represent the axis of the glenoid cavity. Over this, the height corresponding to half of the glenoid cavity and to 25% is established.
The radiological evaluation involved pre- and postoperative CT scans analysed with the Horos application (version 3.3.6, Pixmeo, Ginebra, Switzerland) in duplicate by one same person, taking the mean of the two measurements as the final measure. In both CT scans we evaluated the glenoid bone defect according to the Pico area measurement system in 2D-CT(10). The postoperative control CT study assessed positioning of the bone graft in relation to the glenoid joint surface in the sagittal and axial planes. For this purpose, and using the multiplanar reconstruction (3D MPR) function, we first obtained a "face to face" view of the glenoid cavity, simultaneously displaying the three planes (axial, sagittal and coronal) in the same window. Then, the axis and height of the glenoid cavity were determined in the sagittal plane based on the method described by Barth et al.(13).
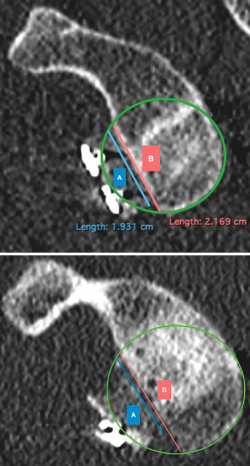
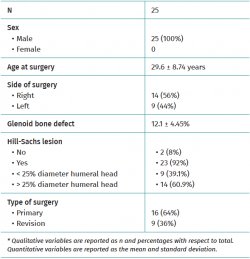
reacae.28474.fs2103006en-figure2.png
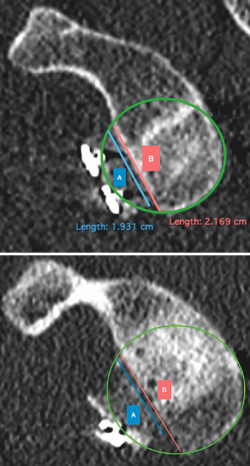
Figure 2. Evaluation of graft positioning in the sagittal section. Two lines are traced of a length equivalent to the size of the glenoid bone defect (B) and to the length of the graft covering the defect (A). Image A shows how most of the bone defect is covered by the graft - the latter therefore being considered to be well positioned. Image B shows that less than 90% of the bone defect is covered by the graft - the latter therefore being considered to be inadequately positioned.
Taking the posteroinferior glenoid border as reference, we traced a first circumference over its contour, and a second circumference above the previous one and tangential to the glenoid borders. The line joining the centre of both circumferences was taken to represent the axis of the glenoid cavity. Over this we estimated the point corresponding to the half and 25% of the glenoid height (Figure 1). The sagittal section was used to determine the position of the graft in the craniocaudal direction (Figure 2). The length (in mm) of the bone defect was measured (B), along with the amount of bone graft covering the defect (A). Percentage covering of the bone defect was estimated from the ratio between A and B. The graft was considered to be well positioned when the percentage coverage of the defect was at least 90%.
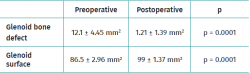
reacae.28474.fs2103006en-figure3.png

Figure 3. Evaluation of the graft position in the axial view, according to the description of Kany et al.(14). A circumference is traced over the glenoid border, and following the curvature of the latter, the amount of graft (in mm) extending beyond or failing to reach this line is measured. Image A shows the graft perfectly positioned, following the curvature of the glenoid concavity. Image B shows the graft medial with respect to the line. Image C shows the graft positioned too lateral.
The position of the graft in the mediolateral direction was evaluated in the axial sections corresponding to 50% and 25% of the glenoid height. For this purpose we used the curvature method described by Kany et al.(14); on the glenoid border and following its curvature, a circumference was traced and we quantified (in mm) the amount of defect that did not reach or surpassed that line at the point where the graft was closest to the native glenoid cavity (Figure 3). Optimum positioning of the graft was considered when the latter was located in line with the glenoid cavity, up to 3 mm lateral or up to 5 mm medial with respect to the glenoid joint border(14). Grafts protruding more than 3 mm were considered to be located lateral, while those located more than 5 mm medial to the glenoid joint surface were classified as being medial.
Statistical analysis
The characteristics of the patients were reported as frequencies and percentages in the case of qualitative variables. Normal distribution of the quantitative variables was assessed using the Kolmogorov-Smirnov test. These variables were reported as the mean and standard deviation (SD), and the Student t-test for paired samples was used for comparison purposes. Statistical significance was considered for p < 0.05.
Results
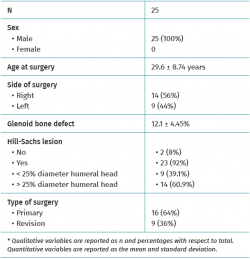
A total of 25 patients that met the inclusion criteria and none of the exclusion criteria were included. A preoperative and a postoperative CT scan was available for evaluation in all the patients included in the final analysis. The epidemiological and clinical data are reported in Table 1.
Iliac crest allografts were used in 13 patients (52%), and iliac crest autografts in the remaining 12 patients (48%). Capsulolabral repair was added to positioning of the bone graft in all cases, with infraspinatus plication using the remplissage technique in 16 of the 25 patients (64%). There were no intraoperative or immediate postoperative complications.
The postoperative radiological study was made an average of 2.77 ± 3.33 months after the operation. In the sagittal plane, the graft covered the bone defect, and was therefore optimally positioned, in 20 of the 25 patients (80%). In the axial plane, at 50% of the height of the glenoid cavity, the graft was seen to be positioned at a mean distance of − 1.05 ± 1.97 mm with respect to the glenoid joint surface. In 92% of the cases (23/25) positioning was within the range considered to be optimum. In one case (4%) the graft was located lateral, and in another case (4%) we observed excessive graft medialisation with respect to the position considered to be optimum. In the position corresponding to 25% of the height of the glenoid cavity, the graft was seen to be positioned at a mean distance of − 1.19 ± 1.55 mm with respect to the glenoid joint surface. All of the grafts were positioned within the accepted range. The final proportion of patients with perfect positioning in both the sagittal and the axial plane was 72% (18/25).
With graft implantation, we recorded a mean increase in glenoid cavity surface of 12.5 ± 3.8 mm2, and 17 patients (68%) showed complete restoration of the glenoid surface (Table 2).
Discussion
The results obtained in this study show that the arthroscopic bone block procedure is able to position the graft precisely at both craniocaudal and mediolateral level, with complete restoration of the glenoid cavity surface in most patients.
Although the outcomes of arthroscopic techniques for the treatment of anterior glenohumeral instability are mostly good(15,16), they may be adversely affected in the presence of a glenoid or humeral bone defect(3). The exact magnitude in order for the bone defect to be considered significant has not been clearly established. Traditionally, it was taken to be 25% of the width of the glenoid cavity (3,17), though recently Shaha et al.(18) have introduced the concept of the subcritical bone defect, in which defects of 13.5% or more of the glenoid width may adversely affect the functional outcomes of Bankart repair. A recent systematic review has established 10% as the magnitude of the glenoid bone defect beyond which glenoid cavity reconstructions should be regarded as indicated(4). However, the presence of a glenoid bone defect not only implies a decrease of glenoid joint surface but also an alteration of its concavity and thus loss of the compression-concavity effect partially responsible for the stability of the glenohumeral joint(19). In a biomechanical study, Moroder et al.(20) observed no linear relationship between the size of the glenoid bone defect and alteration of the concavity of the glenoid cavity. Hence, small bone defects could imply a biomechanical alteration equal to or greater than that of a large glenoid defect; small defects therefore must be evaluated with caution.
The Latarjet procedure has been shown to be effective in repairing anterior glenohumeral instability, and some authors consider it to be the technique of choice when a significant glenoid bone defect is observed(21). However, it is a non-anatomical technique with associated risks, where rescue in the event of failure is complex(22). Although they have been known for years, techniques that use free grafts have gained popularity following their adaptation to the arthroscopic approach, with good results in restoring stability(15).
The arthroscopic approach involves less soft tissue aggression, allows simultaneous Bankart lesion repair and achieves precise and reproducible positioning of the graft thanks to the direct vision given to the surgeon(23). The arthroscopic bone block procedure moreover keeps the tendon of the subscapular muscle intact(24), poses a lesser risk of scapulothoracic dyskinesia(25), and avoids possible complications associated to coracoid transference(22). Biomechanical studies(8) have confirmed the capacity of the free bone graft to restore stability. In addition, the triple blocking effect attributed to the Latarjet technique might not be necessary in patients with a less significant bone defect and in individuals in which soft tissue repair can be made, as advocated by Taverna et al.(16). Our study population consisted of patients with bone defects of over 5% but under 20%, and with good soft tissue conditions in which soft tissue repair alone might not be enough to guarantee stability, but with bone defects of insufficient relevance to indicate a Latarjet technique. In this way, the patients are subjected to an operation that restores stability with a lesser incidence of associated risks and complications, with the Latarjet technique remaining available as rescue option in the event of failure.
The surgical procedure was carried out using a graft sized to 20 × 10 × 10 mm. The main concern of fixed graft sectioning is incomplete coverage of the bone defect when the latter is large. In such cases, this technique, if performed isolatedly, may prove insufficient to guarantee shoulder stability(26). However, in patients with small bone defects, as in our series, the graft dimensions in most cases are sufficient to cover the defect and even to exceed coverage of the defect. In these situations the "excess bone" provided by the graft is not subjected to stress or to remodelling stimulus(27), and may be expected to be reabsorbed according to Wolff's law of bone remodelling(28). On the other hand, positioning of the graft was combined with infraspinatus plication using the remplissage technique in 64% of the patients in the study. Although some authors consider that mere positioning of the bone graft restores glenoid track and therefore stability(16), Hill-Sachs lesions of large size or located medially may benefit from adding remplissage to graft placement, thereby resulting in greater stability(29).
The success of bone block procedures fundamentally depends on the capacity of the graft to restore the arc of the glenoid joint. In order for this to occur, the graft must be positioned in continuity with the glenoid surface(5). According to the literature, the most frequent form of malpositioning, with an incidence of 11-53%(6,30), is excessive lateralisation of the graft, which as evidenced by biomechanical studies(31) and confirmed by subsequent clinical studies, can lead to degenerative arthritis(16,32). While less frequent, an excessively medial position has been associated to an increased risk of recurrence of instability, since the graft fails to act as a bone extension of the glenoid joint surface(6,30). In our series, only one of the grafts (4%) was positioned lateral, one medial (4%), and the remaining 23 were perfectly aligned (92%).
The craniocaudal position is usually assessed on the basis of the percentage graft located above the equator of the glenoid cavity. In this respect, a position above the equator is considered to possibly imply a greater risk of relapse, while a lower position appears to be more susceptible to mechanical failure. The position of the graft with respect to the equator is particularly important in the Latarjet procedure, where an excessively elevated position could reduce the sling effect, thereby increasing the risk of relapse. However, according to the biomechanical studies of Willemot et al.(8), the best position of the graft does not always seem to lie below the equator of the glenoid cavity. In effect, while patients with anteroinferior glenohumeral instability benefit more from positioning all or at least 75% of the graft below the equator, in those cases where instability is exclusively anterior, the force needed to cause dislocation is smaller if only 50% or 75% of the graft is positioned below the equator. Accordingly, in arthroscopic bone block techniques, the aim is to position the bone graft centred with respect to the glenoid bone defect, thereby restoring the glenoid joint surface. Hence, it is considered that the method used in this study for assessing bone graft positioning - estimating the graft position with respect to the bone defect and not with respect to the equator of the glenoid cavity - is more useful for evaluating the craniocaudal position in the arthroscopic bone block technique. Based on this measurement method, 80% of the grafts in our case series were in an optimum position.
Taverna et al.(16), in their study of 26 patients subjected to the arthroscopic bone block procedure, recorded precise graft positioning on the craniocaudal axis in 92.3% of the cases, and a mediolateral location in line with the glenoid joint surface in all of the cases. Boileau et al.(29), in a study of 7 patients subjected to the arthroscopic bone block technique following failed Latarjet repair, recorded precise positioning of the graft in the postoperative CT study of all the patients. The precision in craniocaudal positioning of the graft was slightly lower in our sample than reported in the literature, though we consider that the results may have differed as a consequence of the differences in the positioning assessment systems used.
Both Taverna et al.(16) and Boileau et al.(29) , in their above mentioned studies, employed the double button with posterior guide system for graft fixation, which was also used in our series. With this device and the guide system for drilling, precise graft positioning is achieved, with a decrease in the risk of nerve damage and graft fracture associated to fixation with screws(16,22). None of the patients in the studies of Taverna et al.(16) and Boileau et al.(29) experienced intraoperative complications related to the graft or its fixation, and there were no neurological lesions in the immediate postoperative period. We likewise recorded no such complications in our own series.
The present study has some limitations. Firstly, the sample is relatively small, and no predetermination of the sample size was made. However, since these procedures are relatively infrequent, the present series is no less conditioned in this regard than the studies found in the international literature. On the other hand, the study lacked a control group involving the use of a different technique, though the data have been compared with those available in the literature. However, there is no standard method for assessing the position of the graft in arthroscopic bone block techniques - a fact that complicates the comparison of results among the different series. Lastly, the radiological measurements were made manually, and thus may be affected by human error.
Conclusions
Arthroscopic repair of anterior glenohumeral instability using a cortical double button fixation system with posterior guide for anterior arthroscopic bone block allows precise graft positioning in most patients, restoring the glenoid surface.
Figuras
Figure 1. Estimation of glenoid axis and height according to the method of Barth(13). Two circumferences are traced: one lower, taking the posteroinferior glenoid border as reference, and one higher than the other and tangential to the glenoid borders. The line joining the centre of both circumferences is taken to represent the axis of the glenoid cavity. Over this, the height corresponding to half of the glenoid cavity and to 25% is established.
Figure 2. Evaluation of graft positioning in the sagittal section. Two lines are traced of a length equivalent to the size of the glenoid bone defect (B) and to the length of the graft covering the defect (A). Image A shows how most of the bone defect is covered by the graft - the latter therefore being considered to be well positioned. Image B shows that less than 90% of the bone defect is covered by the graft - the latter therefore being considered to be inadequately positioned.
Figure 3. Evaluation of the graft position in the axial view, according to the description of Kany et al.(14). A circumference is traced over the glenoid border, and following the curvature of the latter, the amount of graft (in mm) extending beyond or failing to reach this line is measured. Image A shows the graft perfectly positioned, following the curvature of the glenoid concavity. Image B shows the graft medial with respect to the line. Image C shows the graft positioned too lateral.
Tablas
Información del artículo
Cita bibliográfica
Autores
Cristina Delgado del Caño
Unidad de Traumatología. Hospital Monográfico Asepeyo Coslada. Madrid
Hospital Universitario Fundación Jiménez Díaz. Madrid
Pablo Cañete San Pastor
Unidad de Hombro y Codo, Hospital de Manises, Valencia, España
Clínica Gastaldi de Traumatología deportiva, Valencia, España
Jorge Díaz Heredia
Cirugía Ortopédica y Traumatología. Unidad de Hombro y Codo. Hospital Universitario Ramón y Cajal. Madrid
Clínica La Antigua. Guadalajara
Editor asociado de REACA
Raquel Ruiz Díaz
Servicio de Cirugía Ortopédica y Traumatología, Hospital Universitario Ramón y Cajal, Madrid, España
Miguel García Navlet
Grupo +QTrauma. Hospital Beata María Ana. Madrid
Sección de Traumatología, Unidad de patología de hombro y codo, Hospital ASEPEYO, Coslada, Madrid, España
Unidad de Hombro y Codo. +QTrauma. Hospital Beata María Ana. Madrid
Cristina Victoria Asenjo Gismero
Equipo +Qtrauma. Hombro y Codo. Hospital Beata María Ana. Madrid
Unidad de Miembro Superior. Hospital FREMAP Majadahonda. Madrid
Cirugía Ortopédica y Traumatología, Hospital ASEPEYO, Coslada, Madrid, España
Ignacio de Rus Aznar
Servicio de Cirugía Ortopédica y Traumatología. Clinica CEMTRO. Madrid
Unidad de Hombro y Codo. Hospital Universitario Ramón y Cajal. Madrid
Servicio de Cirugía Ortopédica y Traumatología. Hospital Monográfico Asepeyo Coslada. Madrid
Hospital Universitario de Torrejón. Madrid
Miguel Ángel Ruiz Ibán
Director de REACA
Cirugía Ortopédica y Traumatología. Unidad de Hombro y Codo. Hospital Universitario Ramón y Cajal. Madrid
Ethical responsibilities
Conflicts of interest. The authors state that they have no conflicts of interest.
Financial support. This study has received no financial support.
Protection of people and animals. The authors declare that this research has not involved studies in humans or in animals.
Data confidentiality. The authors declare that the protocols of their centre referred to the publication of patient information have been followed.
Right to privacy and informed consent. The authors declare that no patient data appear in this article.
Acknowledgements
This study was funded in part by a Research Grant from the Fundación Española de Artroscopia in 2020.
Referencias bibliográficas
-
1Yamamoto N, Itoi E, Abe H, et al. Contact between the glenoid and the humeral head in abduction, external rotation, and horizontal extension: a new concept of glenoid track. J Shoulder Elbow Surg. 2007;16(5):649-56.
-
2Balg F, Boileau P. The instability severity index score. A simple pre-operative score to select patients for arthroscopic or open shoulder stabilisation. J Bone Joint Surg Br. 2007;89(11):1470-7.
-
3Burkhart SS, De Beer JF. Traumatic glenohumeral bone defects and their relationship to failure of arthroscopic Bankart repairs: significance of the inverted-pear glenoid and the humeral engaging Hill-Sachs lesion. Arthroscopy. 2000;16(7):677-94.
-
4Gottschalk LJ, Bois AJ, Shelby MA, Miniaci A, Jones MH. Mean Glenoid Defect Size and Location Associated With Anterior Shoulder Instability. Orthop J Sports Med. 2017;5(1):232596711667626.
-
5Longo UG, Loppini M, Rizzello G, Ciuffreda M, Maffulli N, Denaro V. Latarjet, Bristow, and Eden-Hybinette procedures for anterior shoulder dislocation: systematic review and quantitative synthesis of the literature. Arthroscopy. 2014;30(9):1184-211.
-
6Allain J, Goutallier D, Glorion C. Long-term results of the Latarjet procedure for the treatment of anterior instability of the shoulder. J Bone Joint Surg Am. 1998 Jun;80(6):841-52.
-
7Kraus TM, Graveleau N, Bohu Y, Pansard E, Klouche S, Hardy P. Coracoid graft positioning in the Latarjet procedure. Knee Surg Sports Traumatol Arthrosc. 2016;24(2):496-501.
-
8Willemot LB, Eby SF, Thoreson AR, et al. Iliac bone grafting of the intact glenoid improves shoulder stability with optimal graft positioning. J Shoulder Elbow Surg. 2015 Apr;24(4):533-40.
-
9Weppe F, Magnussen RA, Lustig S, Demey G, Neyret P, Servien E. A Biomechanical Evaluation of Bicortical Metal Screw Fixation Versus Absorbable Interference Screw Fixation After Coracoid Transfer for Anterior Shoulder Instability. Arthroscopy. 2011;27(10):1358-63.
-
10Baudi P, Righi P, Bolognesi D, et al. How to identify and calculate glenoid bone deficit. Chir Organi Mov. 2005;90(2):145-52.
-
11Taverna E, D'Ambrosi R, Perfetti C, Garavaglia G. Arthroscopic bone graft procedure for anterior inferior glenohumeral instability. Arthrosc Tech. 2014;3(6):e653-60.
-
12Purchase RJ, Wolf EM, Hobgood ER, Pollock ME, Smalley CC. Hill-Sachs “Remplissage”: An Arthroscopic Solution for the Engaging Hill-Sachs Lesion. Arthroscopy. 2008;24(6):723-6.
-
13Barth J, Neyton L, Metais P, et al. Is the two-dimensional computed tomography scan analysis reliable for coracoid graft positioning in Latarjet procedures? J Shoulder Elbow Surg. 2017;26(8):e237-e242.
-
14Kany J, Flamand O, Grimberg J, et al. Arthroscopic Latarjet procedure: is optimal positioning of the bone block and screws possible? A prospective computed tomography scan analysis. J Shoulder Elbow Surg. 2016;25(1):69-77.
-
15Kraus N, Amphansap T, Gerhardt C, Scheibel M. Arthroscopic anatomic glenoid reconstruction using an autologous iliac crest bone grafting technique. J Shoulder Elbow Surg. 2014;23(11):1700-8.
-
16Taverna E, Garavaglia G, Perfetti C, Ufenast H, Sconfienza LM, Guarrella V. An arthroscopic bone block procedure is effective in restoring stability, allowing return to sports in cases of glenohumeral instability with glenoid bone deficiency. Knee Surg Sports Traumatol Arthrosc. 2018;26(12):3780-7.
-
17Yamamoto N, Itoi E, Abe H, et al. Effect of an anterior glenoid defect on anterior shoulder stability: a cadaveric study. Am J Sports Med. 2009;37(5):949-54.
-
18Shaha JS, Cook JB, Song DJ, et al. Redefining "Critical" Bone Loss in Shoulder Instability: Functional Outcomes Worsen With "Subcritical" Bone Loss. Am J Sports Med. 2015;43(7):1719-25.
-
19Labriola JE, Lee TQ, Debski RE, McMahon PJ. Stability and instability of the glenohumeral joint: the role of shoulder muscles. J Shoulder Elbow Surg. 2005;14(1 Suppl S):32s-38s.
-
20Moroder P, Damm P, Wierer G, et al. Challenging the Current Concept of Critical Glenoid Bone Loss in Shoulder Instability: Does the Size Measurement Really Tell It All? Am J Sports Med. 2019;47(3):688-94.
-
21Bhatia S, Frank RM, Ghodadra NS, et al. The outcomes and surgical techniques of the latarjet procedure. Arthroscopy. 2014;30(2):227-35.
-
22Griesser MJ, Harris JD, McCoy BW, et al. Complications and re-operations after Bristow-Latarjet shoulder stabilization: a systematic review. J Shoulder Elbow Surg. 2013;22(2):286-92.
-
23Taverna E, D'Ambrosi R, Perfetti C, Garavaglia G. Arthroscopic Bone Graft Procedure for Anterior Inferior Glenohumeral Instability. Arthrosc Tech. 2014;3(6):e653-e660.
-
24Scheibel M, Kraus N, Diederichs G, Haas NP. Arthroscopic reconstruction of chronic anteroinferior glenoid defect using an autologous tricortical iliac crest bone grafting technique. Arch Orthop Trauma Surg. 2008;128(11):1295-300.
-
25Moroder P, Schulz E, Wierer G, et al. Neer Award 2019: Latarjet procedure vs. iliac crest bone graft transfer for treatment of anterior shoulder instability with glenoid bone loss: a prospective randomized trial. J Shoulder Elbow Surg. 2019;28(7):1298-307.
-
26Ljungquist KL, Butler RB, Griesser MJ, Bishop JY. Prediction of coracoid thickness using a glenoid width-based model: implications for bone reconstruction procedures in chronic anterior shoulder instability. J Shoulder Elbow Surg. 2012;21(6):815-21.
-
27Di Giacomo G, de Gasperis N, Costantini A, De Vita A, Beccaglia MA, Pouliart N. Does the presence of glenoid bone loss influence coracoid bone graft osteolysis after the Latarjet procedure? A computed tomography scan study in 2 groups of patients with and without glenoid bone loss. J Shoulder Elbow Surg. 2014;23(4):514-8.
-
28Wolf JH. [Julis Wolff and his "law of bone remodeling"]. Orthopade. 1995;24(5):378-86.
-
29Boileau P, Duysens C, Saliken D, Lemmex DB, Bonnevialle N. All-arthroscopic, guided Eden-Hybbinette procedure using suture-button fixation for revision of failed Latarjet. J Shoulder Elbow Surg. 2019;28(11):e377-e388.
-
30Hovelius L, Albrektsson B, Berg E, et al. Bristow-Latarjet Procedure for Recurrent Anterior Dislocation of the Shoulder: A 2-5 Year Follow-up Study on the Results of 112 Cases. Acta Orthop Scand. 1983;54(2):284-90.
-
31Ghodadra N, Gupta A, Romeo AA, et al. Normalization of glenohumeral articular contact pressures after Latarjet or iliac crest bone-grafting. J Bone Joint Surg Am. 2010;92(6):1478-89.
-
32Cassagnaud X, Maynou C, Mestdagh H. Clinical and computed tomography results of 106 Latarjet-Patte procedures at mean 7.5 year follow-up. Rev Chir Orthop Reparatrice Appar Mot. 2003;89(8):683-92.
Descargar artículo:
Licencia:
Este contenido es de acceso abierto (Open-Access) y se ha distribuido bajo los términos de la licencia Creative Commons CC BY-NC-ND (Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional) que permite usar, distribuir y reproducir en cualquier medio siempre que se citen a los autores y no se utilice para fines comerciales ni para hacer obras derivadas.
Comparte este contenido
En esta edición
- Why the AEA endorses the REACA
- The cortical double button fixation system with posterior guide for anterior arthroscopic bone block allows precise graft positioning
- Injuries of the subscapularis: prevalence of partial lesions and their diagnostic difficulty
- Arthroscopic soft tissue findings associated with tibial plateau fractures
- Radiological classifications and assessment scales for Achilles tendinopathy
- Recurrent anteroinferior dislocation of the shoulder. Essential articles
- Stabilization of <em>os acromiale</em> with cannulated screws and high-resistance sutures
- Anterior arthroscopic bone block with double cortical button fixation system and posterior guide for anterior shoulder instability with glenoid defect. Surgical technique
- Proximal avulsion of the extrinsic volar radiocarpal ligaments following radiocarpal dislocation
Más en PUBMED
Más en Google Scholar


Revista Española de Artroscopia y Cirugía Articular está distribuida bajo una licencia de Creative Commons Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional.