Injuries of the subscapularis: prevalence of partial lesions and their diagnostic difficulty
Lesiones del subescapular: prevalencia de las lesiones parciales y su dificultad diagnóstica
Resumen:
Objetivo: realizar una revisión de roturas parciales del subescapular (SBE) y establecer su prevalencia y la dificultad de su diagnóstico preoperatorio, así como su frecuente asociación a lesiones del supraespinoso (SPE) y de la porción larga del bíceps (PLB).
Material y método: se han revisado de forma retrospectiva los datos de 75 roturas parciales del SBE de entre las 660 roturas de manguito rotador intervenidas por el mismo equipo de cirujanos desde junio de 2008 hasta junio de 2018. Para el estudio de fiabilidad diagnóstica se consideró como patrón de referencia el tipo de lesión diagnosticado por artroscopia, que se comparó con los resultados de las pruebas de exploración y el resultado del estudio de resonancia magnética (RM). Se han recogido también los datos quirúrgicos: tipo y tamaño de lesión; y se han definido los tipos de lesión en relación con la asociación a las del SPE y de la PLB.
Resultados: de los 660 casos, 280 (42,4%) presentaban una rotura del SBE y, de ellos, 75 (11,4% del total y 26,8% de las roturas del subescapular) presentaban roturas consideradas parciales; 33 fueron mujeres, una intervenida de ambos hombros (45,3%) y 41, hombres (54,7%). El dolor se localizaba en la cara anterior del hombro y en 66 casos (88,0%) irradiaba a la cara anterior del brazo. La combinación de test de exploración del SBE solo fue positiva en el 64,7% de las lesiones aisladas del SBE y en un 14,7% del conjunto de la muestra, mientras que el test de Neer fue positivo en el 93,1% de los casos con lesión asociada del SPE. La RM solo identificó el 21,3% de las lesiones del SBE frente a un 70,7% de las lesiones asociadas del SPE.
Conclusiones: las roturas parciales del SBE presentan una prevalencia del 11,4% del total de las lesiones del manguito. Dada la dificultad en su diagnóstico en función de la frecuente asociación con las lesiones del SPE y de la PLB, junto a la validez reducida de las pruebas de exploración y de imagen, se presenta una nueva subclasificación que recoge esta asociación, para un mejor enfoque de su tratamiento quirúrgico.
Nivel de evidencia: IV.
Abstract:
Objective: to conduct a review of partial ruptures of the subscapularis muscle (SSC) and establish their prevalence and preoperative diagnostic difficulty, as well as their frequent association to injuries of the supraspinatus (SSP) and long portion of the biceps (LPB).
Material and methods: a retrospective review was made of the data corresponding to 75 partial ruptures of the SSC out of 660 rotator cuff ruptures operated upon by the same team of surgeons between June 2008 and June 2018. With regard to the analysis of diagnostic reliability, the reference standard was taken to be the type of lesion diagnosed via arthroscopy, establishing comparisons against the results of the exploration tests and the magnetic resonance imaging (MRI) findings. The following surgical data were also recorded: type and size of the lesion, with definition of the types of lesion in relation to the association to those of SSP and LPB.
Results: of the 660 cases, 280 (42.4%) presented SSC rupture, and of these, 75 (11.4% of the total and 26.8% of the SSC ruptures) presented ruptures considered to be partial. There were 33 women —including one operated upon in both shoulders (45.3%)— and 41 men (54.7%). The pain was located on the anterior surface of the shoulder, and in 66 cases (88.0%) it radiated to the anterior surface of the arm. The combination of exploration testing of the SSC only proved positive in 64.7% of the isolated injuries of the SSC and in 14.7% of the global sample, while the Neer test proved positive in 93.1% of the cases with associated injury of the SSP. Magnetic resonance imaging only identified 21.3% of the injuries of the SSC versus 70.7% of the associated injuries of the SSP.
Conclusions: the prevalence of partial ruptures of the SSC corresponds to 11.4% of the total cuff injuries. Given their diagnostic difficulty due to the frequent association to injuries of the SSP and LPB, together with the limited validity of the exploration and imaging tests, a new subclassification is presented that contemplates this association with a view to improving surgical treatment.
Level of evidence: IV.
Introduction
An injury of the subscapularis muscle (SSC) produces an imbalance of the pairs of forces that act upon the shoulder, stabilising it in the transverse plane. This results in a tendency towards anterior migration of the humeral head during motion that proves more relevant the greater the lesion happens to be(1,2). Repair of the SSC is therefore crucial in order to restore this balance. A number of factors have contributed to improve the diagnosis and treatment of these lesions, such as the description of new exploration manoeuvres, magnetic resonance imaging (MRI), and the consolidation of arthroscopic surgical techniques of the shoulder.
With the adequate assessment of partial lesions —which are more difficult to diagnose— the incidence of involvement of the SSC could reach 35% of all reported lesions of the rotator cuff(3). Some studies report a prevalence of partial lesions of 13-19%, and even of 50%(4,5,6). They have also been frequently associated to injuries of the long portion of the biceps (LPB) or of the bicipital groove(3,7,8,9). The reported difficulty of diagnosing these injuries has caused them to be regarded as "occult lesions"(3,10,11). Magnetic resonance arthrography would allow a more reliable preoperative diagnosis(12), and arthroscopy is considered to be the gold standard for identifying them(13,14,15).
The main objective of the present study was to assess the prevalence of partial lesions of the SSC in relation to the cases subjected to arthroscopic surgery, and to establish a new subclassification according to the frequent association of disease conditions of the supraspinatus muscle (SSP) and of the LPB. As secondary objectives, an evaluation was made of the validity of clinical exploration and MRI studies compared with the arthroscopic findings in relation to the diagnosis of these small ruptures.
Methods
A retrospective review was made of the data corresponding to 660 rotator cuff ruptures operated upon by the same team of surgeons between June 2008 and June 2018. The database created for the study was used to compile the following parameters: type and size of the rupture, patient age and gender, the affected side, characterization of the pain, data on the exploration and results of the MRI study performed in all cases, as commented further below. The study was approved by the Research Ethics Committee of Grupo Hospitalario Quirónsalud, with registry code 2020/124-COT-PGQ.
In order to characterize the type and size of the rupture, we used the classification of the French school, which contemplates 5 types(9,16): type I or isolated partial tendon (or upper third) lesion; type II or isolated complete lesion of the upper third with retraction; type III or lesion of the entire tendon but without coracohumeral conflict; type IV or complete tendon lesion, with retraction, the presence of coracohumeral stenosis, anterior migration of the humeral head and muscle atrophy (less than grade 3); and type V, analogous to the previous type but with muscle atrophy in excess of grade 3.
The inclusion criteria were: only cases with partial rupture of the SSC corresponding to its upper third (types I and II), with preoperative exploration, MRI study, and a good description of the lesion in the arthroscopic evaluation. The exclusion criteria were: all cases with larger size ruptures (i.e., types III, IV and V), cases in which the lesion affected the SSC but in the context of large or massive rupture and/or cases that were the result of failed previous repair procedures.
With regard to diagnosis in the clinic, use was made of the lift-off test(1), Napoleon test or belly-press test(2), belly-off test(17) and the bear-hug test(18), due to the reportedly greater specificity afforded by their combined application(19). In addition, in all cases we also performed the classical Neer manoeuvre for assessment of the SSP and the tests of Yergason and Speed, for evaluating the LPB(19,20). In order to diagnose possible involvement of the coracohumeral space, the pain provocation test was performed on the anterior surface of the shoulder by means of combined antepulsion, internal rotation and adduction, as described by Lo and Burkhart(8). In addition to carrying out the radiographic study with the three most common projections (anteroposterior [AP], axillary oblique and Y-lateral scapular view), the diagnostic process was completed with an MRI study.
Surgical procedure
All surgeries were performed by the same surgical team. The patients were operated upon in lateral decubitus under combination general anaesthesia and interscalene block through the conventional portals —posterior, anterior and anterosuperior (AS)— using the technique previously described(21,22).
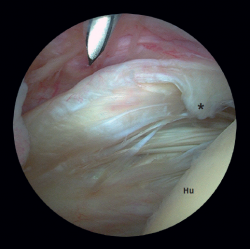
The posterior lever push manoeuvre described by Burkhart(23) was used to the arm to improve the anterior space and allow better diagnosis and access to the lesion (Figure 1). The latter was explored by initially debriding the rotator interval as described by Lafosse(16), thus allowing better evaluation of frequent damage to the walls of the groove of the LPB, the stability of the LPB, and the size of SSC and SSP rupture(23). This exploration is made from the subacromial anterolateral approach, which allows much wider vision encompassing the entire coracoid space and the trajectory of the tendon.
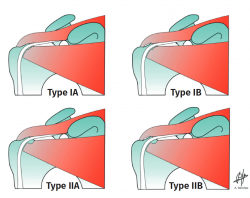
Arthroscopic exploration allowed combined assessment of the damage to the SSC and anterior margin of the SSP. According to the form of presentation of this association, isolated partial ruptures of the SSC were subclassified as types I-A and II-A, while partial SSC ruptures combined with incomplete ruptures of the most anterior portion of the SSP or AS pattern ruptures were subclassified as types I-B and II-B (Figure 2). This is a personalised subclassification that we feel to be necessary in order to adequately interpret the results of the joint repair of both tendons, which requires an approach differentiated from that used in isolated SSC repair.
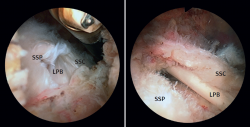
The type I-A and II-A ruptures were repaired from the glenohumeral space via a posterior viewing portal and an AS portal. In type I-B and II-B ruptures, suturing of the lesion was carried out in the same way, but that of the SSP was completed from the subacromial space using a third anterolateral portal (Figure 3). The type I-A ruptures were usually repaired with a single anchoring, while the type I-B, II-A and II-B ruptures typically required two or three.
Statistical analysis
The SPSS Statistics V22 software was used for data analysis. A descriptive study was made of the sample characteristics, while associations between qualitative variables were evaluated based on contingency tables and the Fisher exact test. Statistical significance was considered for p < 0.05.
With regard to the analysis of diagnostic reliability, the reference standard was taken to be the type of lesion diagnosed via arthroscopy(13,14,15), establishing comparisons against the results of the exploration tests and the MRI findings. The results of the Neer manoeuvre were analysed in relation to the cases of associated injury of the SSP. The results of the LPB provocation tests were assessed in relation to the cases of associated injury of said LPB. The results of the SSC tests (lift-off test, belly-press test, belly-off test and bear-hug test) were analysed in relation to the global sample both individually and according to the combinations of tests that proved positive in one same individual.
Results
Of the 660 cases operated upon during the study period, 280 (42.4%) presented SSC rupture, though in three cases the exploration or MRI findings were not correctly documented. Of the 277 well documented cases, 75 (11.4% of the total and 27.1% of the SSC ruptures) presented type I and II ruptures, and constituted the sample for the present analysis.
The series consisted of 74 patients: 33 women —one of which was operated upon in both shoulders— (45.3%) and 41 men (54.7%). The mean patient age at the time of surgery was 60.7 years (range: 47-81). The right shoulder was operated upon in 44 cases (58.7%) and the left shoulder in 31 cases (41.3%).
The firm diagnosis regarding the type of lesion involved was established by arthroscopic examination, with the following distribution: 17 cases corresponded to isolated SSC lesion —10 of type I-A (13.3%) and 7 of type II-A (9.3%)— while 23 cases presented small lesion with an AS pattern of type I-B (30.7%) and 35 of type II-B (46.7%). In 67 of the 75 cases (89.3%) we recorded an associated partial injury in the tendon of the LPB and/or its groove, which corresponded to 4 of the 10 cases (40%) of type I-A and 21 of the 23 cases (90%) of type I-B, as well as all the cases of type II-A and II-B lesions. Laterality showed no statistical significance with respect to the type of lesion —the distribution being very similar between the left and the right side for all types of injuries.
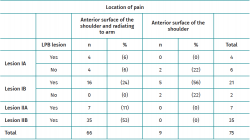
The pain was mainly located on the anterior surface of the shoulder, and radiated to the anterior surface of the arm (66 cases, 88.0%), following the trajectory of the biceps to the elbow flexure (Table 1). Given the strong association to partial injury of the tendon of the LPB, in all types of lesion it was more common for the pain to radiate over the anterior surface of the arm, while pain was circumscribed to the anterior region of the shoulder only in 9 cases: 5 with associated injury of the LPB and four without.
The LPB provocation tests proved positive in 66 of the 75 cases, while arthroscopy revealed 67 cases with injury in the tendon or in the groove of the LPB. There were 5 false-negative and 4 false-positive results. The sensitivity of these tests among the studied sample was therefore 92.5%, with a specificity of 50.0% and a positive and negative likelihood ratio of 1.9 and 0.1, respectively.
With regard to the SSC exploration tests, none of the 75 cases yielded a positive result either in the belly-off test or in the Napoleon test or belly-press test —these tests only being positive in the cases characterised by larger injuries not included in the present study. The lift-off test was positive in 11 individuals —all of them included among the 17 cases (64.7%) of isolated lesions (types IA and IIA). The bear-hug test was positive in 27 patients (36%) distributed among all the observed types of lesions. 17 individuals corresponded to the cases of isolated lesions (types IA and IIA) and 10 to type IB and IIB lesions. Of the 17 cases with isolated lesions, 11 (64.7%) presented a combined positive result of the lift-off and bear-hug tests. The Neer test was positive in 54 subjects (93.1%) out of the 58 cases which arthroscopically presented tendon lesion of the SSP (types IB and IIB), and proved negative in the 17 cases (types IA and IIA) with isolated injury of the SSC.
The results corresponding to the MRI study are reported in Table 2. In two cases, the MRI scan identified no type of lesion, while it was able to identify 16 of the 75 cases (21.3%) of SSC tendon injury, 16 of the 67 cases (23.9%) of LPB injury, and 41 of the 58 cases (70.7%) of SSP injury.
Discussion
The importance of this study is that it suggests a correlation between the injuries confirmed by arthroscopy and the symptoms. Arthroscopy, which is regarded as the gold standard for identifying injuries(13,14,15), allowed us to validate their type, size and location, establishing a new subclassification in relation to the frequent association to injuries of the SSP and LPB. The recorded total prevalence of SSC injuries among all the treated cuff lesions was 42.4%, versus 11.4% in the case of partial injury of the SSC. The clinical relevance of these data serves to alert us to the frequency of such injuries and prevent them from going unnoticed, particularly when hidden by damage to the SSP —which is better diagnosed from the clinical manifestations and the imaging findings.
While some studies have reported a prevalence of partial injuries of the SSC of between 13-19%(3,4), it has also been described that the total prevalence of these ruptures can reach up to 35%(3) and even 50%(5,6). The data obtained from our series are consistent with these figures and offer a combined view of the percentage of complete and partial injuries in relation to the total treated rotator cuff injuries.
The patients with SSC injuries reported pain on the anterior surface of the shoulder and on performing activities below horizontal level(7). This distinguishing feature is confirmed by our own study, where most of the patients presented pain of insidious onset and located on the anterior surface.
For correct evaluation, it is advisable to jointly perform the lift-off test(1), the Napoleon test or belly-off test(16), the belly-press test(2) and the bear-hug test(18). In their article, Barth et al.(18) indicated that these ruptures cannot be adequately predicted in up to 40% of the cases, even when these tests are jointly used. Our own data are consistent with this same diagnostic difficulty described by Barth et al. Considered isolatedly, the bear-hug test offers greater sensitivity, especially in detecting injuries of the upper third of the SSC(18), as occurred in all the isolated injuries of our series. However, the sensitivity found on jointly performing all the tests with respect to the total cases of the series decreased to 14.7% versus the 60% described in the literature(18). The coexistence of lesions of the SSP and LPB very probably influenced this result.
On the other hand, it must be taken into account that through the usual glenohumeral posterior approach we can only visualise between 26-37% of the tendon(24). Injuries of the SSC must be suspected in many cases, especially those of a partial nature (longitudinal and transversal)(25). We need to be careful in searching for them, in order to stop regarding them as "occult lesions"(3,11) or injuries that are difficult to diagnose(26). The view obtained from the anterolateral approach of the subacromial space —once the coracohumeral space has been debrided— is much wider, encompassing all of the coracoid process, and visualisation of the tendon of the SSC is much more complete.
With regard to imaging diagnosis, MRI shows high sensitivity(27), but likewise in the case of large ruptures with muscle atrophy and fat infiltration. In our series, MRI was able to identify 70.7% of the added SSP ruptures, but only 21.3% of the partial and incomplete SSC ruptures. This is consistent with the findings of other published studies(12,13,14,15).
A recent article has proposed a new classification of these partial lesions of the SSC(28). Although isolated lesions appear to be present, on examining the concurrent injuries, concomitant injuries of the SSP are seen in 80% of the cases and injuries of the biceps pulley are seen in 100%. In our opinion, this strong association defines a pattern which in view of its frequency is better understood with the classification as types IA, IB, IIA and IIB which we have used. Furthermore, it is complicated to perform such precise measurement of the size of the lesions, particularly with such narrow limits between the different types. This classification exclusively addresses the anatomical aspects related to isolated surgical repair of the SSC. However, the frequent association of type I and II lesions to likewise incomplete injuries of the most anterior portion of the SSP and the LPB requires a combined surgical intervention. Hence, this is a personalised subclassification that we feel to be necessary in order to adequately interpret the results of the joint repair of both tendons, and of intervention upon this disease of the LPB versus isolated repair of the SSC.
The anatomical aspects referred to insertion are addressed by the classification of partial ruptures of the SSC published by Yoo et al.(6), based on four zones. However, we do not find this classification to be useful, due to the same problems in identifying the limits between the described zones, and because the association of injuries of the SSP and LPB are not taken into account.
A possible limitation of the present study is referred to the variability index between observers, in both the clinical explorations and in the MRI studies. Nevertheless, the data obtained are in line with those published elsewhere(18,27). Likewise, since this is a retrospective review, the different consideration of some aspects in time could constitute a source of bias. Nevertheless, as this is a descriptive study of injuries based on arthroscopy, we are able to establish a correct correlation with only a small margin of error.
The clinical relevance of our study lies in the possibility of establishing the frequency of these partial injuries of the SSC in order to avoid them from being underdiagnosed, since they are often overshadowed by the clinical manifestations of the injuries of the SSP and LPB.
Conclusions
The prevalence of partial ruptures of the SSC corresponds to 11.4% of the total cuff injuries. Given their diagnostic difficulty due to the frequent association to injuries of the SSP and LPB, together with the limited validity of the exploration and imaging tests, a new subclassification is presented that contemplates this association with a view to improving surgical treatment.
Figuras
Figure 1. View from the posterior glenohumeral portal of a type IA (*) partial rupture of the subscapularis in a left shoulder not diagnosed by MRI. Hu: humerus.
Figure 2. Subclassification of combined and partial ruptures of the subscapularis and supraspinatus into types IA, IB and IIA, IIB.
Figure 3. View from the posterior subacromial portal of type IB and IIB ruptures in left shoulders. A: type IB; B: type IIB. LPB: long portion of the biceps; SSC: subscapularis; SSP: supraspinatus.
Tablas
Table 1. Location of pain according to the type of lesion and its association to damage to the tendon or groove of the long portion of the biceps (LPB).
Información del artículo
Cita bibliográfica
Autores
Asier Cuéllar Ayestarán
Instituto Vasco de Cirugía Ortopédica-Traumatología (IVCOT). Policlínica Gipuzkoa Quirón-Salud. Donostia-San Sebastián, Gipuzkoa
Adrián Cuéllar Ayestarán
Instituto Vasco de Cirugía Ortopédica-Traumatología (IVCOT). Policlínica Gipuzkoa Quirón-Salud. Donostia-San Sebastián, Gipuzkoa
Alberto Sanchez Sobrino
Servicio de Cirugía Ortopédica y Traumatología, Hospital Galdakao-Usansolo, Galdakao, Vizcaya, España
Martín Eusebio Barra
Departamento de Fisioterapia. Universidad Internacional de Cataluña. Sant Cugat del Vallés, Barcelona
Ricardo Cuéllar Gutiérrez
Instituto Vasco de Cirugía Ortopédica-Traumatología (IVCOT). Policlínica Gipuzkoa Quirón-Salud. Donostia-San Sebastián, Gipuzkoa
Ethical responsibilities
Conflicts of interest. The authors state that they have no conflicts of interest.
Financial support. This study has received no financial support.
Protection of people and animals. The authors declare that this research has not involved human or animal experimentation.
Data confidentiality. The authors declare that the protocols of their work centre referred to the publication of patient information have been followed.
Right to privacy and informed consent. The authors declare that no patient data appear in this article.
Referencias bibliográficas
-
1Gerber C, Krushell RJ. Isolated rupture of the tendon of the subscapularis muscle. J Bone Joint Surg Am. 1991;73:389-94.
-
2Gerber C, Hersche O, Farron A. Isolated rupture of the tendon of the subscapularis tendon. J Bone Joint Surg Am. 1996;78:1015-23.
-
3Bennett WF. Subscapularis medial and lateral coracohumeral ligament insertion anatomy: arthroscopic appearance and incidence of “hidden” rotator interval lesions. Arthroscopy. 2001;17:173-80.
-
4Nove-Josserand L, Gerber C, Walch G. Lesions of the anterosuperior rotator cuff. En: Iannotti JP, Warner JJP, Gerber C (eds.). Complex and revision problems in shoulder surgery. Philadelphia: Lippincott-Raven; 1997. pp. 165-76.
-
5Gebellí Jové JT, Iftime P, Bel LLop M, Andreu Jiménez Ll, Buñuel Viñau A. Sutura artroscópica del tendón del subescapular. Técnica y resultados. Rev Esp Artroscop Cir Artic. 2018;25:48-55.
-
6Yoo JC, Rhee YG, Shin SJ, et al. Subscapularis tendon tear classification based on 3-dimensional anatomic footprint: a cadaveric and prospective clinical observational study. Arthroscopy. 2015 Jan;31(1):19-28.
-
7Bennett WF. Arthroscopic repair of isolated subscapularis tears: s prospective cohort with 2- to 4- follow-up. Arthroscopy. 2003;19:131-43.
-
8Lo IKY, Burkhart SS. The comma sign: an arthroscopic guide to the torn subscapularis tendon. Arthroscopy. 2003;19:334-7.
-
9Lafosse L, Brzoska R, Bouchard A, Reiland Y, Audebert S, Jost B, Toussaint B. Traitement arthroscopique des lésions du sous-scapulaire. Maitrise Orthop. 2005;145.
-
10Collin P, Matsumura N, Lädermann A, Denard PJ, Walch G. Relationship between massive chronic rotator cuff tear pattern and loss of active shoulder range of motion. J Shoulder Elbow Surg. 2014;23(8):1195-202.
-
11Lyons RP, Green A. Subscapularis tendon tears. J Am Acad Orthop Surg. 2005;13(5):353-63.
-
12De Jesús JO, Parker L, Frangos AJ, Nazarian LN. Accuracy of MRI, MR arthrography, and ultrasound in the diagnosis of rotator cuff tears: a meta-analysis. AJR Am J Roentgenol. 2009 Jun;192(6):1701-7.
-
13Adams CR, Schoolfield JD, Burkhart SS. Accuracy of preoperative magnetic resonance imaging in predicting a subscapularis tendon tear based on arthroscopy. Arthroscopy. 2010;26(11):1427-33.
-
14Barth J, Audebert S, Toussaint B, et al. Diagnosis of subscapularis tendon tears: are available diagnostic tests pertinent for a positive diagnosis? Orthop Traumatol Surg Res. 2012;98(8 Suppl):S178-85.
-
15Foad A, Wijdicks CA. The accuracy of magnetic resonance imaging and magnetic resonance arthrogram versus arthroscopy in the diagnosis of subscapularis tendon injury. Arthroscopy. 2012;28(5):636-41.
-
16Lafosse L, Reiland Y, Audebert S, Toussaint B, Gobezie R, Jost B. Structural integrity and clinical outcomes after arthroscopic repair of isolated subscapularis tears. J Bone Joint Surg Am. 2007;89:1184-93.
-
17Scheibel M, Magosch P, Pristch M, Lichtenberg S, Habermeyer P. The belly-off sign: a new clinical diagnostic sign for subscapularis lesions. Arthroscopy. 2005;21:1229-35.
-
18Barth JRH, Burkhart SS, DeBeer JF. The bear hug test: the most sensitive test for diagnosing a subscapularis tears. Arthroscopy. 2006;22:1076-84.
-
19Beaudreuil J, Nizard R, Thomas T, et al. Contribution of clinical tests to the diagnosis of rotator cuff disease: a systematic literature review. Joint Bone Spine. 2009 Jan;76(1):15-9.
-
20Neer CS 2nd. Impingement lesions. Clin Orthop Relat Res. 1983 Mar;(173):70-7.
-
21Cuéllar-Gutiérrez R, Aguinaga-Badiola I, Busto-Avis G, Baguer-Antonio A, Cuéllar-Ayestarán A. Reconstrucción por artroscopia del subescapular: ¿por qué no en decúbito lateral? Cuad Artroscop. 2009;16(1):34-44.
-
22Cuéllar-Ayestarán As, Cuéllar-Ayestarán Ad, Seijas-Vázquez R, Barra-López ME, Cuéllar-Gutiérrez R. Reparación artroscópica de lesiones del subescapular: análisis de resultados y factores adversos en un grupo de origen degenerativo. Rev Esp Cir Ortop Traumatol. 2021. In Press, Corrected Proof.
-
23Burkhart SS, Tehrany AM. Arthroscopic subscapularis tendon repair: Technique and preliminary results. Arthroscopy. 2002;18(5):454-63.
-
24Richards DP, Burkhart SS, Lo IK. Subscapularis tears: arthroscopic repair techniques. Orthop Clin North Am. 2003;34(4):485-98.
-
25Arai R, Sugaya H, Mochizuki T, Nimura A, Moriishi J, Akita K. Subscapularis tendon tear: An anatomic and clinical investigation. Arthroscopy. 2008;24:997-1004.
-
26Mendoza M, Cardoner JC, Samso F, Coba J. Lesions of the subscapular tendon regarding two cases in arthroscopic surgery. Arthroscopy. 1993;9:671-4.
-
27McCrum E. MR Imaging of the Rotator Cuff. Magn Reson Imaging Clinic N Am. 2020;28(2):165-79.
-
28Martetschläger F, Zampeli F, Tauber M, Habermeyer P, Leibe M. A classification for partial subscapularis tendon tears. Knee Surg Sports Traumatol Arthrosc. 2021;29: 275-83.
Descargar artículo:
Licencia:
Este contenido es de acceso abierto (Open-Access) y se ha distribuido bajo los términos de la licencia Creative Commons CC BY-NC-ND (Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional) que permite usar, distribuir y reproducir en cualquier medio siempre que se citen a los autores y no se utilice para fines comerciales ni para hacer obras derivadas.
Comparte este contenido
En esta edición
- Why the AEA endorses the REACA
- The cortical double button fixation system with posterior guide for anterior arthroscopic bone block allows precise graft positioning
- Injuries of the subscapularis: prevalence of partial lesions and their diagnostic difficulty
- Arthroscopic soft tissue findings associated with tibial plateau fractures
- Radiological classifications and assessment scales for Achilles tendinopathy
- Recurrent anteroinferior dislocation of the shoulder. Essential articles
- Stabilization of <em>os acromiale</em> with cannulated screws and high-resistance sutures
- Anterior arthroscopic bone block with double cortical button fixation system and posterior guide for anterior shoulder instability with glenoid defect. Surgical technique
- Proximal avulsion of the extrinsic volar radiocarpal ligaments following radiocarpal dislocation
Más en PUBMED
Más en Google Scholar
Más en ORCID


Revista Española de Artroscopia y Cirugía Articular está distribuida bajo una licencia de Creative Commons Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional.