Radiological classifications and assessment scales for Achilles tendinopathy
Clasificaciones radiológicas y escalas de valoración de la tendinopatía del Aquiles
Resumen:
Las tendinopatías de Aquiles son enfermedades con una incidencia creciente debido al aumento de la práctica deportiva. Se realiza una revisión de las clasificaciones radiológicas de esta enfermedad, así como de las escalas de valoración clínicas. Hasta la fecha, no se ha desarrollado ningún sistema de clasificación radiológica aceptado universalmente. La mayoría de las clasificaciones descritas atienden a parámetros ecográficos, aunque también se han publicado clasificaciones por resonancia magnética. El grosor del tendón, la presencia de neovascularización y la ecogenicidad tendinosa son los únicos parámetros ecográficos que, medidos de forma conjunta, se han correlacionado con el desarrollo de síntomas, por lo que las clasificaciones radiológicas que pretendan aportar valor pronóstico deberían incorporar estas 3 variables. Las escalas de valoración clínica permiten cuantificar la gravedad de la tendinopatía aquílea y su impacto en la calidad de vida. De forma ideal, se debería utilizar un cuestionario general de salud y una escala de valoración específica. El VISA-A es la única escala de valoración específica de la tendinopatía del Aquiles. Tiene una adecuada correlación clínica, es reproducible y ha sido validado al castellano, por lo que su utilización está muy extendida en la valoración de esta enfermedad.
Abstract:
Achilles tendinopathies are becoming increasingly common as a result of the increase in sports activity. A review is made of the radiological classifications of this injury, and of the clinical assessment scales employed. To date, no universally accepted radiological classification has been established. Most of the described classifications focus on ultrasound parameters, though classifications based on magnetic resonance imaging (MRI) parameters have also been published. The thickness of the tendon, the presence of neovascularisation, and tendon echogenicity are the only ultrasound parameters which when measured jointly have been correlated to the development of symptoms. Radiological classifications that aim to be of prognostic value therefore should incorporate these three parameters. The clinical assessment scales allow us to quantify the severity of Achilles tendinopathy and its impact upon patient quality of life. Ideally, a general health questionnaire and a specific assessment scale should be used. In this regard, the VISA-A is the only specific Achilles tendinopathy assessment scale developed to date. It affords adequate clinical correlation, is reproducible, and has been validated in its Spanish version. As a result, this tool is widely used for evaluating this disease.
Introduction
The incidence of disorders of the foot and ankle has increased in recent years as a result of the growth in sports activities(1). Disease conditions of the Achilles tendon account for a very important percentage of these disorders, and can result in great disability and worsening of patient quality of life.
At present, radiological evaluation of Achilles tendinopathy is very important as a complement to the clinical information. Different radiological classifications have been proposed, which ideally should afford data on the disease in question, as well as contribute prognostic information to help decide which treatment to provide according to the stage of the tendinopathy.
The clinical assessment scales have been developed with the same purpose in mind. These are evaluating tools used to measure different characteristics of the disease with a view to assessing the effects of treatment upon patient health. At least 139 scales have been used to evaluate the clinical outcomes in patients with disorders of the ankle and foot(2). Of these scales, only some can be used to evaluate Achilles tendinopathy, and there is no clear consensus as to which clinical assessment scale should be used on a systematic basis(3,4).
The present study offers a review of the radiological classifications of Achilles tendinopathy, and of the clinical assessment scales applicable to such disease.
Radiological classifications of Achilles tendinopathy
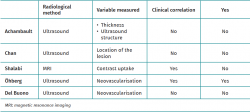
Although studies have been made of the prognostic usefulness of many radiological variables in Achilles tendinopathy, there is no agreement as to which of them are important enough to serve as the basis for a universal classification system(4). For this reason, different classification models have been proposed depending on the ra diological variable analysed — though none of them can be taken to constitute a clear reference standard. Table 1 provides a summarised comparison of the classifications which are described below.
Archambault ultrasound classification(5)
The authors of this classification conducted a retrospective review of the ultrasound findings in a series of consecutive cases diagnosed with non-insertional Achilles tendinopathy. The findings were classified into three types according to the thickness of the tendon and its ultrasound appearance over the long axis:
- Grade I. Tendon of normal appearance: parallel tendon margins and fibrillar ultrasound structure.
- Grade II. Thickened tendon: non-parallel margins, increased tendon thickness and fibrillar structure.
- Grade III. Tendon with hypoechoic zones and altered fibrillar ultrasound structure, with or without tendon thickening.
This classification was not found to be useful from the prognostic perspective, since no significant differences were observed between the ultrasound grades and the persistence of symptoms following conservative treatment at 24 months of follow-up(5).
Chan classification(6)
This is an anatomical classification that divides tendinopathies according to the affected region of the tendon. In this respect, three zones of the Achilles tendon are distinguished based on sagittal MRI images or ultrasound images over the long axis:
- Intramuscular tendon: muscle fibers are seen to be still inserted within the trajectory of the tendon.
- Free tendon: absence of muscle fibers; this zone in turn can be divided into three subzones of similar length:
– Proximal.
– Middle.
– Distal. - Calcaneal insertion: at the confluence between the tendon and the posterior calcaneal tuberosity.
The publication in which this classification was described was not accompanied by a case series to demonstrate its clinical correlation or prognostic value. The clinical usefulness of this tool is therefore limited.
Öhberg score of tendon neovascularisation(7)
It has often been postulated that the appearance of neovascularisation in a pathological tendon is related to the development of pain(8,9). Different studies have attempted to quantify the degree of neovascularisation with a view to assessing the effectiveness of different therapies(7,9). The Öhberg score is the most widely used classification and recognises 5 types of tendon according to the number of neovessels observed in the ultrasound study:
- Grade 0: no intratendon vascularisation.
- Grade 1+: 1 or 2 small vessels in the anterior portion of the tendon.
- Grade 2+: 2 vessels located at any point of the tendon.
- Grade 3+: 3 vessels located at any point of the tendon.
- Grade 4+: > 3 vessels located at any point of the tendon.
Del Buono classification of tendon neovascularisation(6)
This is an ultrasound classification of the grade of neovascularisation of the pathological tendon:
- Grade I: 1 altered vessel in the tendon.
- Grade II: 2 altered vessels in the tendon.
- Grade III: neovascularisation enveloping < 50% of the thickness of the tendon.
- Grade IV: neovascularisation enveloping 50-90% of the thickness of the tendon.
- Grade V: neovascularisation enveloping > 90% of the thickness of the tendon.
This again is a morphological classification in which the authors conducted no clinical or prognostic validation.
Shalabi magnetic resonance imaging classification(10)
This classification groups Achilles tendinopathy according to the uptake of the pathological tendon following a gadolinium contrast administration. Four degrees of tendon involvement are considered based on the MRI data:
- Grade 0: no enhanced uptake.
- Grade I: mildly enhanced intrasubstance uptake.
- Grade II: moderately enhanced intrasubstance uptake.
- Grade III: greatly enhanced intrasubstance and peritendinous uptake.
Although this classification was not found to be of prognostic value, it did show an acceptable clinical correlation, since close to 85% of all patients with some degree of tendon involvement before surgery presented lesser involvement at two years of follow-up, with associated clinical improvement(10).
Achilles tendinopathy assessment scales
The measurement of outcomes in orthopaedic surgery and traumatology has become a crucial aspect for knowing the effectiveness of the applied treatments and for publishing objective data in clinical research. In most of the existing assessment scales, the subjective data from the patients themselves are very important, since they have been shown to be better indicators of the final outcome than questionnaires based only on objective clinical data(11).
At present, the most widespread recommendation in assessing the outcomes of any disease process is to use a generic health questionnaire and another questionnaire specific of the disease in question(11). A number of questionnaires have been developed that specifically evaluate the function of the ankle and hindfoot, and there is even a specific questionnaire for evaluating Achilles tendinopathy(12), which has become the reference tool for measuring the outcomes of this disease.
Evaluation of health condition
The SF-12(13) (Table 2), as the short version of the SF-36(14,15), is a good example of a generic questionnaire, since it offers a general view of the patient health condition. Furthermore, it can be completed easily and rapidly. The scores of each of the dimensions of the SF-12 range between 0-100, where 100 indicates optimum health and 0 is the poorest score possible(14,15).
Specific evaluation of foot and ankle disorders
Foot and Ankle Ability Measure (FAAM)(16)
The FAAM is a generic scale used for the evaluation of foot and ankle disorders, and exclusively measures subjective aspects of the disease. It is especially focused on individuals with great physical demands, and so has been mainly used in athletes with chronic ankle instability. This tool consists of 29 items divided into two parts: gestures related to activities of daily living (21 items) and aspects gestures of sports activity (8 items). The FAAM has not been validated in Spanish or for specifically evaluating disorders of the Achilles tendon.
American Orthopaedic Foot and Ankle Society (AOFAS)(17) (Table 3)
Originally published in 1994, this is the most widely used foot and ankle scale in clinical research(18). It consists of 4 classification systems, each adapted to a different anatomical area, namely the ankle-hindfoot, midfoot, hallux-metatarsophalangeal zone-interphalangeal joints and metatarsophalangeal-lesser interphalangeal joints. The scale integrates subjective and objective data and comprises three sections: function, pain and alignment. The AOFAS has been used to evaluate different procedures such as trauma surgery, arthroplasties, arthrodesis, etc. It therefore has not been specifically designed to evaluate the function of the Achilles tendon, though it offers excellent reproducibility and clinical correlation(19,20). Nevertheless, it has a number of limitations that must be taken into account. Firstly, the AOFAS has not been formally validated(18,21). Furthermore, over half of the evaluated items are not considered to be especially important by either patients or physicians(22). Lastly, this tool must be evaluated by an examiner, which can generate inter-observer variability and reduce the validity of the results obtained. For all these reasons, it is currently not advised to use this scale on an isolated basis for evaluating patients with foot and ankle problems(18).
European Foot and Ankle Score (EFAS)(23) (Table 4)
The EFAS is the assessment system of the European Foot and Ankle Society. In the same way as the previous scale, it is useful for evaluating the function of the ankle and subtalar, talonavicular and calcaneocuboid regions, and has been used to evaluate the treatment of fractures, arthroplasties, arthrodesis and instability procedures. This instrument is divided into 2 parts: a general questionnaire referred to pain and activities of daily living, and a section specifically dedicated to sports.
Foot and Ankle Outcome Score (FAOS)(24)
The FAOS is a questionnaire entirely self-completed by the patient. It comprises 42 items that evaluate the outcomes based on 5 subscales (pain, other symptoms, activities of daily living, sports and leisure activities, and quality of life related to the foot and ankle). It appears to be useful for evaluating outcomes that are relevant for the patient and addresses ankle stability following ligament reconstruction.
Visual Analogue Scale-Foot and Ankle (VAS-FA)(2)
The VAS-FA is a visual scale that evaluates disorders of the foot and ankle. It has been validated for both healthy individuals and patients with disease conditions. The instrument is reliable and has been validated in a number of languages. The VAS-FA consists of 20 items divided into 3 groups: pain, function and others.
Foot Function Index (FFI)(25)
The FFI is a subjective scale that consists of 23 items in its original description, divided into 3 subscales: pain, function and limitation of activity. All the variables are measured using a visual scale, where higher scores indicate greater disease. A number of subsequent versions have been developed, since the original scale could not be completed by different population groups, leaving too many unanswered questions(26). At present, all these subsequent versions have not shown sufficient validity compared with the SF-36. Its isolated use therefore cannot be recommended(21,26).
Manchester-Oxford Foot Questionnaire (MOXFQ)(27)
The MOXFQ is a scale entirely self-completed by the patient. It was originally designed to evaluate the outcomes of foot and ankle surgeries in clinical trials, and therefore proved useful only in the academic setting(27). It consists of 3 sections: pain, gait / difficulty standing, and social interaction, and higher scores are indicative of increased severity of disease. A short version, the MOXFQ-Index, has recently been introduced, with results comparable to those of the original MOXFQ, and possessing adequate validity compared with the SF-36(28).
Specific assessment of Achilles tendinopathy
The Victorian Institute of Sports Assessment–Achilles questionnaire (VISA-A)(29) (Table 5) is the only scale specifically developed to evaluate Achilles tendinopathy. It measures the severity of tendinopathy based on the assessment of pain, function and the impact upon activity. This instrument consists of 10 items: stiffness, pain on walking, pain on stretching, walking down stairs, standing on tiptoe, jumping on one leg, sports activity, pain on loading the tendon, and training time. The VISA-A uses a numerical rating scale from 0-100 points, where higher scores correspond to people with improved functional condition.
It is easily understood by patients and has been shown to offer good clinical correlation(30). In addition, the VISA-A has been validated in Spanish(31). In sum, it is considered to be the reference scale for assessing the severity of Achilles tendinopathies.
Discussion
The present review describes different radiological classifications of Achilles tendinopathy, and the most commonly used clinical assessment scales. Both tools are employed to better characterise disease and allow a more detailed description of the disease process, with a view to facilitating the therapeutic approach.
It is clear that most of the described classifications are based on the ultrasound findings. This is because the accessibility of ultrasound has caused it to become the first choice of use of imaging diagnostic technique in most cases. However, the ultrasound findings with demonstrated clinical correlation or of prognostic value are scarce(32). In 2018, Matthews et al. published a systematic review of the ultrasound classifications of Achilles tendinopathies, with the aim of determining the most widely used parameters(33). Likewise, they conducted a meta-analysis to determine whether any ultrasound finding was of prognostic value in relation to the development of symptoms. The study included 19 publications, and the parameters most commonly used for establishing a classification were found to be the thickness of the tendon, echogenicity, and the presence of vascularisation. These findings were of prognostic utility in reference to the development of clinical symptoms, especially when 3 parameters were measured simultaneously instead of only 2. The authors therefore concluded that although there is great variability in the published ultrasound classifications, the most reliable tools in terms of prognostic value should at least include the aforementioned 3 parameters. However, no classifications including these parameters and applied to clinical practice on a generalised basis have been developed to date. In addition, as has been commented above, very few classifications are of prognostic value. As a result, it is currently not possible to recommend basing therapeutic decisions exclusively on the radiological stage of the disease.
The assessment scales allow numerical quantification of the severity of the disorder. An ideal assessment tool should be able to record clinically relevant changes, and should be reliable, validated and reproducible. Objective measurements, such as radiological parameters, might not adequately correlate to the patient symptoms or quality of life(2). No clear consensus has been reached regarding which clinical assessment scale to use in patients with Achilles tendinopathy(3,4).
Curiously, the scale most widely used to assess disease of the foot and ankle - the AOFAS - has not demonstrated sufficient validity in comparison with other less recognised scales such as the FFI, the FAOS or the FAAM. As a result, its isolated use for assessing the outcomes cannot be recommended(18). These other scales, including the MOXFQ, do not specifically address Achilles tendinopathy, and have been validated for more general disorders of the foot and ankle. The exception could be the FAAM, which has been validated for assessing chronic ankle instability. Thus, the VISA-A is seen to be the most specific and reliable option for assessing Achilles tendinopathy, and its use should thus be recommended, associated to a generic health questionnaire.
The main limitation of the present study is that it is not a systematic review, and no analysis is made of the results described in the literature. It is a narrative review made to describe the radiological classifications and the clinical assessment scales used in patients with Achilles tendinopathy.
Conclusions
The ultrasound findings that appear to be of prognostic value in evaluating Achilles tendinopathy are the thickness of the tendon, the presence of neovascularisation, and echogenicity measured simultaneously. To date, no radiological classification has included these items or is able to offer adequate prognostic correlations; as a result, no concrete classification may be considered preferable to the rest. At least both a general and a specific health questionnaire should be used. In this regard, the VISA-A is the only specific Achilles tendinopathy assessment scale developed to date, and has been shown to be reproducible and offer good clinical correlation.
Información del artículo
Cita bibliográfica
Autores
Pablo Carnero Martín de Soto
Arthrosport Zaragoza
Instituto Malagueño de Traumatología del Deporte (IMATDE). Málaga
Hospital Regional de Málaga
Deborah González-García
Complejo Hospitalario Quirón Juan Bravo. Madrid
Unidad de Pie y Tobillo. Hospital Universitario de Guadalajara
Hospital ASEPEYO. Coslada. Madrid
Néstor Antonio Zurita Uroz
Hospital IMED Elche. Alicante
Arthrosport. Zaragoza
Servicios Médicos. Real Federación Española de Natación
Servicio de Cirugía Ortopédica y Traumatología. Hospital IMED Elche. Alicante
Ethical responsibilities
Conflicts of interest. The authors state that they have no conflicts of interest.
Financial support. This study has received no financial support.
Protection of people and animals. The authors declare that this research has not involved human or animal experimentation.
Data confidentiality. The authors declare that the protocols of their centre referred to the publication of patient information have been followed.
Right to privacy and informed consent. The authors declare that no patient data appear in this article.
Referencias bibliográficas
-
1Meshal A, Najla A, Maryam A, Mark G. Cross-cultural adaptation and validation of an Arabic version of the American Orthopedics Foot and Ankle Score (AOFAS). Foot Ankle Surg. 2020 Dec;26(8):876-82.
-
2Saarinen AJ, Uimonen MM, Sandelin H, Toom A, Richter M, Repo JP. Minimal important change for the visual analogue scale foot and ankle (VAS-FA). Foot Ankle Surg. 2021 Feb;27(2):196-200.
-
3Jia Y, Huang H, Gagnier JJ. A systematic review of measurement properties of patient-reported outcome measures for use in patients with foot or ankle diseases. Qual Life Res. 2017;26:1969-2010.
-
4Rolfson O, Eresian KC, Bohm E, et al. Patient-reported outcome measures in arthroplasty registries. Acta Orthop. 2016;87:3-8.
-
5Archambault JM, Wiley JP, Bray RC, Verhoef M, Wiseman DA, Elliott PD. Can sonography predict the outcome in patients with achillodynia? J Clin Ultrasound. 1998 Sep;26(7):335-9.
-
6Del Buono A, Chan O, Maffulli N. Achilles tendon: functional anatomy and novel emerging models of imaging classification. Int Orthop. 2013 Apr;37(4):715-21.
-
7Ohberg L, Alfredson H. Ultrasound guided sclerosis of neovessels in painful chronic Achilles tendinosis: pilot study of a new treatment. Br J Sports Med. 2002 Jun;36(3):173-5.
-
8De Jonge S, de Vos RJ, Van Schie HT, Verhaar JA, Weir A, Tol JL. One-year follow-up of a randomised controlled trial on added splinting to eccentric exercises in chronic midportion Achilles tendinopathy. Br J Sports Med. 2010 Jul;44(9):673-7.
-
9De Vos RJ, Weir A, Cobben LP, Tol JL. The value of power Doppler ultrasonography in Achilles tendinopathy: a prospective study. Am J Sports Med. 2007 Oct;35(10):1696-701.
-
10Shalabi A, Kristoffersen-Wiberg M, Aspelin P, Movin T. MR evaluation of chronic Achilles tendinosis. A longitudinal study of 15 patients preoperatively and two years postoperatively. Acta Radiol. 2001 May;42(3):269-76.
-
11Feliu EC, Vidal N, Conesa X. Escalas de valoración en cirugía ortopédica y traumatología. Trauma. 2010;21(1):34-43.
-
12Robinson JM, Cook JL, Purdam C, et al.; Victorian Institute Of Sport Tendon Study Group. The VISA-A questionnaire: a valid and reliable index of the clinical severity of Achilles tendinopathy. Br J Sports Med. 2001 Oct;35(5):335-41.
-
13Huo T, Guo Y, Shenkman E, Muller K. Assessing the reliability of the short form 12 (SF-12) health survey in adults with mental health conditions: a report from the wellness incentive and navigation (WIN) study. Health Qual Life Outcomes. 2018 Feb 13;16(1):34.
-
14Alonso J, Regidor E, Barrio G, Prieto L, Rodríguez C, de la Fuente L. Valores poblacionales de referencia de la versión española del Cuestionario de salud SF-36. Med Clin (Barc). 1998;111:410-6.
-
15Bhandari M, Sprague S, Hanson B, et al. Health-Related Quality of Life Following Operative Treatment of Unstable Ankle Fractures: A Prospective Observational Study. J Orthop Trauma. 2004 Jul;18(6):338-45.
-
16Martin RL, Irrgang JJ. Burdett RG, Conti SF, van Swearingen JM. Evidence of validity for the Foot and Ankle Ability Measure (FAAM). Foot Ankle Int. 2005;26:968-83.
-
17Kitaoka HB, Alexander IJ, Adelaar RS, Nunley JA, Myerson MS, Sanders M. Clinical rating systems for the ankle-hindfoot, midfoot, hallux, and lesser toes. Foot Ankle Int. 1994 Jul;15(7):349-53.
-
18Shazadeh Safavi P, Janney C, Jupiter D, Kunzler D, Bui R, Panchbhavi VK. A Systematic Review of the Outcome Evaluation Tools for the Foot and Ankle. Foot Ankle Spec. 2019 Oct;12(5):461-70.
-
19Ibrahim T, Beiri A, Azzabi M, Best AJ, Taylor GJ, Menon DK. Reliability and validity of the subjective component of the American Orthopaedic Foot and Ankle Society clinical rating scales. J Foot Ankle Surg. 2007 Mar-Apr;46(2):65-74.
-
20SooHoo NF, Vyas R, Samimi D. Responsiveness of the foot function index, AOFAS clinical rating systems, and SF-36 after foot and ankle surgery. Foot Ankle Int. 2006 Nov;27(11):930-4.
-
21Hunt KJ, Lakey E. Patient-Reported Outcomes in Foot and Ankle Surgery. Orthop Clin North Am. 2018 Apr;49(2):277-89.
-
22Baumhauer JF, McIntosh S, Rechtine G. Age and sex differences between patient and physician-derived outcome measures in the foot and ankle. J Bone Joint Surg Am. 2013 Feb 6;95(3):209-14.
-
23Richter M, Agren PH, Besse JL, et al. EFAS Score - Multilingual development and validation of a patient-reported outcome measure (PROM) by the score committee of the European Foot and Ankle Society (EFAS). Foot Ankle Surg. 2018 Jun;24(3):185-204.
-
24Roos EM, Brandsson S, Karlsson J. Validation of the foot and ankle outcome score for ankle ligament reconstruction. Foot Ankle Int. 2001 Oct;22(10):788-94.
-
25Budiman-Mak E, Conrad KJ, Roach KE. The Foot Function Index: a measure of foot pain and disability. J Clin Epidemiol. 1991;44(6):561-70.
-
26Sierevelt IN, Zwiers R, Schats W, et al. Measurement properties of the most commonly used Foot- and Ankle-Specific Questionnaires: the FFI, FAOS and FAAM. A systematic review. Knee Surg Sports Traumatol Arthrosc. 2018 Jul;26(7):2059-73.
-
27Dawson J, Coffey J, Doll H, et al. A patient-based questionnaire to assess outcomes of foot surgery: validation in the context of surgery for hallux valgus. Qual Life Res. 2006 Sep;15(7):1211-22.
-
28Morley D, Jenkinson C, Doll H, et al. The Manchester-Oxford Foot Questionnaire (MOXFQ): Development and validation of a summary index score. Bone Joint Res. 2013 Apr 3;2(4):66-9.
-
29Robinson JM, Cook JL, Purdam C, et al.; Victorian Institute Of Sport Tendon Study Group. The VISA-A questionnaire: a valid and reliable index of the clinical severity of Achilles tendinopathy. Br J Sports Med. 2001 Oct;35(5):335-41.
-
30Iversen JV, Bartels EM, Langberg H. The victorian institute of sports assessment - Achilles questionnaire (VISA-A) - A reliable tool for measuring Achilles tendinopathy. Int J Sports Phys Ther. 2012 Feb;7(1):76-84.
-
31Hernández-Sánchez S, Poveda-Pagán EJ, Alakhdar-Mohmara Y, Hidalgo MD, Fernández-de-Las-Peñas C, Arias-Buría JL. Cross-cultural Adaptation of the Victorian Institute of Sport Assessment-Achilles (VISA-A) Questionnaire for Spanish Athletes With Achilles Tendinopathy. J Orthop Sports Phys Ther. 2018 Feb;48(2):111-20.
-
32Comin J, Cook JL, Malliaras P, et al. The prevalence and clinical significance of sonographic tendon abnormalities in asymptomatic ballet dancers: a 24-month longitudinal study. Br J Sports Med. 2013 Jan;47(2):89-92.
-
33Matthews W, Ellis R, Furness J, Hing W. Classification of Tendon Matrix Change Using Ultrasound Imaging: A Systematic Review and Meta-analysis. Ultrasound Med Biol. 2018 Oct;44(10):2059-80.
Descargar artículo:
Licencia:
Este contenido es de acceso abierto (Open-Access) y se ha distribuido bajo los términos de la licencia Creative Commons CC BY-NC-ND (Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional) que permite usar, distribuir y reproducir en cualquier medio siempre que se citen a los autores y no se utilice para fines comerciales ni para hacer obras derivadas.
Comparte este contenido
En esta edición
- Why the AEA endorses the REACA
- The cortical double button fixation system with posterior guide for anterior arthroscopic bone block allows precise graft positioning
- Injuries of the subscapularis: prevalence of partial lesions and their diagnostic difficulty
- Arthroscopic soft tissue findings associated with tibial plateau fractures
- Radiological classifications and assessment scales for Achilles tendinopathy
- Recurrent anteroinferior dislocation of the shoulder. Essential articles
- Stabilization of <em>os acromiale</em> with cannulated screws and high-resistance sutures
- Anterior arthroscopic bone block with double cortical button fixation system and posterior guide for anterior shoulder instability with glenoid defect. Surgical technique
- Proximal avulsion of the extrinsic volar radiocarpal ligaments following radiocarpal dislocation
Más en PUBMED
Más en Google Scholar
Más en ORCID


Revista Española de Artroscopia y Cirugía Articular está distribuida bajo una licencia de Creative Commons Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional.