Anatomical ligament reconstruction with allograft in chronic acromioclavicular dislocations restores joint stability and function. Short-term outcomes in 14 cases
La reconstrucción ligamentosa anatómica con aloinjerto en luxaciones acromioclaviculares crónicas restaura la estabilidad articular y permite recuperar la función. Resultados a corto plazo en 14 casos
Resumen:
Objetivo: analizar los resultados a corto plazo de una técnica anatómica que reconstruye los complejos ligamentosos acromioclavicular y coracoclavicular con ayuda de un aloinjerto tendinoso para el tratamiento de las luxaciones acromioclaviculares de más de 3 semanas de evolución.
Métodos: estudio longitudinal prospectivo de una serie de casos con luxaciones acromioclaviculares de más de 3 semanas de evolución que fueron tratados con una técnica de reconstrucción anatómica de los complejos ligamentosos acromioclavicular y coracoclavicular con aloinjerto de tendón tibial. Se analizaron los resultados radiológicos y funcionales con las escalas de Constant-Murley, American Shoulder and Elbow Surgeons (ASES)-hombro y Quick-DASH (Disabilities of the Arm, Shoulder and Hand); además, se evaluó la estabilidad de la articulación acromioclavicular y la cinética escapulotorácica.
Resultados: se evaluaron 14 sujetos al menos un año tras la cirugía –media: 2,7 (1,1) años–. Hubo mejorías significativas en las 3 escalas clínicas evaluadas: Constant-Murley pasó de 64,4 (13,0) en el preoperatorio a 93,6 (12,6) al finalizar el seguimiento (p < 0,001); Quick-DASH evolucionó de 71,8 (15,9) a 95,4 (12,0) (p < 0,001); y ASES-hombro mejoró de 58,3 (15,8) a 95,5 (11,5) (p < 0,001). Trece sujetos (93%) presentaban una articulación estable, tanto en el plano vertical como horizontal, indolora y sin disfunción escapulotorácica residual al finalizar el seguimiento. En solo un caso se apreció un mal resultado funcional, con pérdida de la reducción, inestabilidad y sintomatología persistente. Hubo otro caso de pérdida de la reducción sin repercusión funcional. Apareció ensanchamiento de los túneles moderado y asintomático en la mayor parte de los pacientes: el tamaño de los túneles en el postoperatorio fue de 5,1 (0,3) mm frente a 5,9 (1,0) mm al finalizar el seguimiento (p = 0,001).
Conclusiones: los resultados a corto plazo de una técnica anatómica que reconstruye los complejos ligamentosos acromioclavicular y coracoclavicular con ayuda de un aloinjerto tendinoso para el tratamiento de las luxaciones acromioclaviculares de más de 3 semanas de evolución son satisfactorios. La técnica es, en esta serie corta de casos, segura y no presenta complicaciones.
Nivel de evidencia: IV (serie de casos).
Relevancia clínica: en sujetos con inestabilidad acromioclavicular de más de 3 semanas de evolución, la reconstrucción de los complejos ligamentosos acromioclaviculares y coracoclaviculares con aloinjerto tendinoso es eficaz y segura.
Abstract:
Objective: to analyse the short-term outcomes of an anatomical technique that reconstructs the acromioclavicular and coracoclavicular ligament complexes with the help of a tendon allograft for the management of acromioclavicular dislocations with an evolution of over three weeks.
Methods: a prospective longitudinal study was made of a series of cases with acromioclavicular dislocations with an evolution of over three weeks treated through anatomical reconstruction of the acromioclavicular and coracoclavicular ligament complexes using tibial tendon allografts. The radiological and functional outcomes were analysed based on the Constant-Murley, American Shoulder and Elbow Surgeons (ASES)-shoulder and Quick-DASH (Disabilities of the Arm, Shoulder and Hand) scales. The stability of the acromioclavicular joint and the scapulothoracic kinetics were also assessed.
Results: a total of 14 subjects were evaluated at least one year after surgery –mean 2.7 (1.1) years–. There were significant improvements in all three of the scales: The Constant-Murley score increased from 64.4 (13.0) preoperatively to 93.6 (12.6) at the end of follow-up (p < 0.001); the Quick-DASH score increased from 71.8 (15.9) to 95.4 (12.0) (p < 0.001); and the ASES-shoulder score increased from 58.3 (15.8) to 95.5 (11.5) (p < 0.001). Thirteen patients (93%) presented a stable joint in both the vertical and the horizontal plane, with no pain and without residual scapulothoracic dysfunction at the end of follow-up. Only one patient presented a poor functional outcome, with loss of reduction, instability and persistent symptoms. Another subject suffered loss of reduction, though without functional repercussions. Moderate and asymptomatic widening of the tunnels was observed in most patients: tunnel size after surgery was 5.1 (0.3) mm versus 5.9 (1.0) mm at the end of follow-up (p = 0.001).
Conclusions: satisfactory short-term outcomes were obtained with this anatomical technique that reconstructs the acromioclavicular and coracoclavicular ligament complexes with the help of a tendon allograft for the management of acromioclavicular dislocations with an evolution of over three weeks. In this small case series, the technique was seen to be safe, with no complications.
Level of evidence: IV (case series).
Clinical relevance: in individuals presenting acromioclavicular instability with an evolution of over three weeks, reconstruction of the acromioclavicular and coracoclavicular ligament complexes using tendon allografts is both effective and safe.
Introduction
Traumatic injury to the acromioclavicular joint is frequent and affects young and active individuals(1). Mild acute lesions (types I and II of the Rockwood classification) are subjected to conservative management, with good results(2). In the case of more serious injuries (Rockwood types III, IV and V), surgery is considered much more often(2,3,4,5). Nevertheless, conservative management is effective in many cases, and there is a clear tendency to adopt this approach and to offer surgery only in those cases characterized by persistent clinical manifestations following a variable period of conservative treatment(6). This strategy is justified by the acceptable outcomes of surgery in the management of such lesions in the subacute or chronic phase(7,8).
Many techniques are used for the treatment of chronic dislocations of the acromioclavicular joint(9), and there are no clear indications as to which technique is best. Since the primary healing capacity of the coracoclavicular ligaments (CCLs) beyond three weeks is limited(10), dislocations with an evolution longer than this can be regarded as non-acute, and some type of biological augmentation becomes necessary. In general terms, the alternatives are divided into non-anatomical techniques, that modify the normal anatomy using the coracoacromial ligament or the coracobrachialis to substitute the affected ligaments, and anatomical techniques based on the use of autologous, allogenic or artificial tendon grafts to reconstruct the ligaments. Although historically the techniques used were focused on management of the CCLs, it now seems to have become clear that the acromioclavicular ligaments (ACLs) are also crucial. As a result, anatomical techniques that restore both ligament complexes and repair the trapezoid-deltoid fascia are becoming the option of choice for the management of these lesions(11,12,13).
The present study was carried out to analyse the short-term radiological and functional outcomes of an anatomical technique that reconstructs the acromioclavicular and coracoclavicular ligament complexes with the help of a tendon allograft for the management of acromioclavicular dislocations with an evolution of over three weeks.
Methods
A prospective longitudinal study was made of a series of cases with subacute or chronic acromioclavicular dislocations treated by one same surgical team using a technique involving reconstruction of the CCLs and ACLs with the help of a posterior tibial allograft. The study was approved by the Ethics Committee of the Hospital Universitario Ramón y Cajal (Spain). All patients gave their consent to participation in the study.
Patients
The study included all patients with subacute or chronic acromioclavicular dislocations (over three weeks of evolution) requiring surgical management due to persistent symptoms after acute injury. The patients were operated upon by three senior shoulder surgeons from one same team in three both public and private hospitals.
The inclusion criteria were: 1) age over 18 years; 2) type III, IV or V acromioclavicular injury according to the Rockwood classification, with an evolution of over three weeks; and 3) persistent symptoms (pain or functional limitation) despite conservative management.
The exclusion criteria were: 1) acute lesions; 2) type I or II injury according to the Rockwood classification; 3) presence of associated lesions of the pectoral girdle (fractures or dislocations); and 4) previous surgery of the mentioned joint.
Surgical technique
The surgical technique reproduces that presented by Kibler et al. in 2017(12) and referred to by these authors as the MADOK technique. The technique has been described in detail in an additional article(14), but is summarized here. A longitudinal incision is made over the distal third of the clavicle, in line with its major axis, to expose the acromioclavicular joint. The ruptured ACLs are identified and separated (they almost always remain inserted in the acromion). An anterior or posterior tibial tendon allograft is prepared, measuring 15 cm in length and 5 mm in thickness. The coracoid process is identified and a passage beneath it is prepared with a dissector. Two orifices measuring 5 mm in diameter are made craniocaudally in the clavicle over the insertional footprint of the conoid and trapezoid ligaments. The acromioclavicular joint is reduced and temporarily fixed with a Kirschner wire. The graft is passed through each of the orifices and beneath the coracoid process; reinforcement is provided by four passes of high-resistance polyethylene tape (UltraTape®, Smith & Nephew, Boston, USA) displaced adjunct to the graft beneath the coracoid process, with knotting over the distal surface of the clavicle. Both ends of the allograft are sutured together over the clavicle and are placed over the acromioclavicular joint. Two sutures are passed through two 2-mm tunnels on the dorsal side of the acromion, and the ends of the tendon are sutured to these sutures over the lateral bone bridge. The ACLs are reinserted over the distal clavicle with the help of two all-suture implants measuring 1.7 mm (SutureFix® 1.7 mm, Smith & Nephew, Boston, USA). We repair the trapezoid-deltoid fascia over the reparation and the temporary fixation pin is removed. Resection of the distal clavicle is not carried out; in the case of evident deformity due to osteophytes, shape smoothing is performed.
Following surgery, all patients were immobilized with a 20° abduction sling during four weeks (to facilitate recovery of glenohumeral abduction), allowing its removal for active exercises of the elbow and hand, and for passive shoulder flexion exercises. Pendular exercises were explicitly to be avoided. During weeks 5 to 8, the orthosis was suspended and assisted active mobility exercises were started. Free active mobility was allowed in week 9, though strengthening exercises were postponed until 90% of the normal range of motion was achieved. An exercise program was then started, focused on the recovery of normal scapulothoracic kinetics.
Clinical and radiological evaluation
Prior to surgery, the epidemiological data were collected and all patients were evaluated using the Constant-Murley, American Shoulder and Elbow Surgeons (ASES)-shoulder and Quick-DASH (Disabilities of the Arm, Shoulder and Hand) scales. We measured the coracoclavicular distance in the healthy shoulder and the affected shoulder from plain anteroposterior radiographs, tracing a vertical line from the upper part of the coracoid process to the lower surface of the clavicle(15).
After surgery, the intraoperative complications were recorded. Likewise, the coracoclavicular distance and size of the clavicular tunnels were measured from the postoperative radiographs. Reduction was considered to be adequate when there was no increase in the coracoclavicular distance of over 25% with respect to the contralateral side.
The patients were evaluated one year after surgery and on a yearly basis thereafter. Use was made of the Constant-Murley, ASES-shoulder and Quick-DASH scales (the scores were standardized to a scale of 0-100, where 100 = perfect functional outcome). The presence of complications over follow-up was also documented. Based on the plain radiographs, we recorded the coracoclavicular distance in the affected shoulder, widening of the tunnels, and the presence of fractures or osteolysis of the distal clavicle. Likewise, careful exploration of the reconstructed joint and of the scapulothoracic kinetics was carried out(12), with palpation of the joint in search of pain in response to pressure or crepitation. We palpated the distal clavicle and acromion in search of signs of subtle instability in the superoinferior and anteroposterior planes, establishing comparisons with the healthy side. The joint was inspected during flexion and abduction movements of the arm in order to assess its dynamic stability. Any appearance of increased translation in either of the two planes was recorded. We visually analysed the presence of static and dynamic scapular asymmetries during active flexion of the shoulder(16).
Statistical analysis
Normal distribution of the quantitative variables was assessed using the Kolmogorov-Smirnov test. These variables were reported as the mean-standard deviation (SD), and the Student t-test for paired samples was used for comparison purposes. Statistical significance was considered for p < 0.05.
Results
The MADOK technique was applied to a total of 19 patients between January 2015 and January 2020. Two subjects were excluded: one presented malunion of an associated fracture of the middle third of the clavicle, and corrective osteotomy was performed at the same time, while the other patient had undergone surgery for acromioclavicular instability on three previous occasions. Thus, the inclusion criteria were finally met by 17 subjects, of which 14 (82%) were available for evaluation an average of 2.7 (1.1) years after surgery (range 14 months - 5 years).
reacae.28373.fs2102004-figure1.png
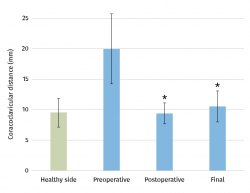
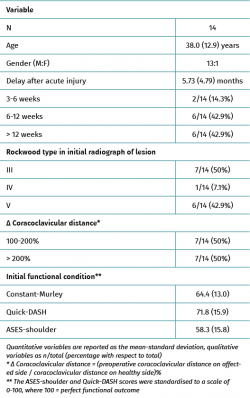
Figure 1. Coracoclavicular distance measured from the anteroposterior radiograph of the shoulder. The data correspond to the affected side (preoperative) and the healthy side as reference. The described technique allowed recovery of normal coracoclavicular distance after surgery (postoperative) and at the end of follow-up (final). * Significant differences (p < 0.0001) with respect to the preoperative values. There were no significant differences among the postoperative, final and healthy side values.
The epidemiological, clinical and radiological data of the 14 finally included patients are reported in Table 1. The degree of craniocaudal displacement of the affected clavicle with respect to the contralateral clavicle is shown in Figure 1. Fresh frozen tibial tendon allografts measuring 5 mm in diameter were used in all the procedures, and 5-mm tunnels were made in the distal clavicle. There were no perioperative or immediate postoperative complications.
The postoperative radiographic control evidenced correct reduction of the joint, with a restored coracoclavicular distance in 12 patients (85.7%); two subjects presented insufficient reduction but which was considered acceptable (43% and 54% increase in coracoclavicular distance).
At the end of follow-up, significant improvement was observed in all three functional assessment scales and their sub-sections (Table 2 and Figure 2). Thirteen patients (93%) presented distal clavicular stability in both planes at exploration, with no noticeable scapulothoracic dyskinesia. The good reduction achieved in the immediate postoperative period in 12 of the 14 patients persisted at the end of follow-up, though the degree of displacement in the two subjects with insufficient correction in the postoperative period was seen to progress (with increments of 74% and 132%, respectively). In addition, we documented osteolysis of the distal clavicle and mild degenerative changes in the acromioclavicular joint in 5 cases. With regard to the size of the clavicular tunnels, an increase in diameter was noted, though the increase was only > 2 mm in three tunnels corresponding to three different individuals.
reacae.28373.fs2102004-figure2.png

Figure 2. An 18-year-old male presenting type V acromioclavicular dislocation initially subjected to conservative management. One year after the injury he presented persistent symptoms and absolute limitation for sports activities (A). Surgery was performed with good reduction of the deformity (B), and four years after the operation the functional outcome was excellent (C), with minimum degenerative changes in the acromioclavicular joint and some widening of the clavicular tunnels.
The two patients in which initial correct reduction of the joint was not achieved were seen to group most of the complications. The first patient, a 52-year-old woman with type IV acromioclavicular dislocation operated upon after four weeks of pain and dysfunction refractory to conservative management, presented insufficient reduction (54% displacement), progressive loss of reduction (finally 132%) and a poor functional outcome 14 months after surgery (Constant-Murley = 54; Quick-DASH = 69; ASES-shoulder = 57) - with evident scapular dyskinesia and clear anteroposterior and craniocaudal instability of the distal clavicle (Figure 3). The patient declined any other additional procedures. The second patient, a 50-year-old man with type V acromioclavicular dislocation subjected to conservative management during four months without success, presented initially insufficient reduction (43%) with progressive loss of reduction (74% at the end of follow-up), osteolysis of the distal clavicle and widening of the proximal orifice of the clavicle to 7.7 mm. These findings nevertheless had no functional repercussions, since after 18 months of follow-up the functional outcome was very good (Constant-Murley = 94; Quick-DASH = 88; ASES-shoulder = 99).
reacae.28373.fs2102004-figure3.png
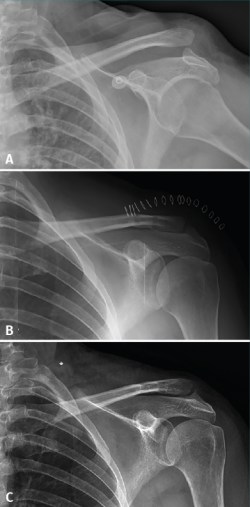
Figure 3. A 52-year-old woman with type IV acromioclavicular dislocation (A) subjected to surgery four weeks after injury due to refractory pain and dysfunction. The surgical outcome was considered acceptable, though with insufficient reduction (B). Fourteen months after surgery, the patient suffered persistent symptoms and loss of reduction was seen to have progressed (C).
Discussion
The main finding of this study is that the MADOK technique for reconstruction of the CCLs and ACLs with allografts is effective in restoring stability and function in patients with chronic acromioclavicular dislocations. Good correction of the instability is achieved during the surgical procedure, and consistent outcomes are obtained 2.7 years after the operation, without relevant complications.
There is much controversy as to which technique is best for the management of chronic acromioclavicular instabilities. In the same way as in other disorders, there are innumerable technical variants. In general terms, the surgeon should take three decisions into account: whether to perform an anatomical reconstruction of the joint and its ligaments, or use a non-anatomical technique; whether to use a graft as an adjunct to the soft tissues; and, if so, whether to use an autologous, allogenic or artificial graft. All these options have their advocates, who very recently have published excellent results(17,18,19,20).
Two systematic reviews have been published in 2020 that allow some light to be shed on this issue. Borbas et al.(21) conducted a meta-analysis of 27 studies involving 590 patients, comparing the outcomes of anatomical techniques with artificial grafts, anatomical techniques with tendon grafts, and non-anatomical techniques. The authors concluded that while the outcomes were similar, the studies of greater methodological quality were favourable to the anatomical techniques with grafts. On the other hand, Sircana et al.(13) carried out a meta-analysis of 44 studies involving over 1000 patients, and came to the conclusion that anatomical reconstructions (with either biological or artificial grafts) afforded the best results. It must be taken into account that the real differences in outcomes were small among the different techniques, and that all the evaluated procedures had similar complication rates and offered good results.
The outcomes obtained in the present series are similar to those reported by other authors using anatomical techniques to reconstruct both ligament complexes with grafts. Kibler et al.(12), in the initial description of the MADOK technique, recorded good results in 15 patients followed-up on during three years, with restoration of stability in both planes, no residual dyskinesia, and only one case of loss of reduction with a poor functional outcome. Saccomanno et al.(11), using a very similar technique including a tunnel in the acromion through which the autograft was passed, obtained good results in 30 patients followed-up on over an average of two years. Loss of reduction of the acromioclavicular joint was observed in four cases, but this did not appear to have an important functional impact. The only poor outcome in this series was related to a lack of reduction of the joint in the immediate postoperative period; precise intraoperative assessment of reduction should always be carried out.
In the present series widening of the clavicular tunnels was regularly observed over follow-up, though no relevant functional effect was noted. Berhold et al.(22) also observed such widening without functional repercussions in a review of 24 patients with three years of follow-up, though Sircana et al.(13) in their meta-analysis recorded clavicular fractures associated to the tunnels in 0.7% of the subjects subjected to biological reconstructions with grafts. It cannot be ruled out that this may represent a problem that was not evidenced in our series due to the limited number of patients involved.
Lastly, the outcomes in the present series can be regarded as excellent. This has certain implications in the acute management of severe acromioclavicular dislocations: conservative strategies become more relevant, since deferred surgery affords results similar to those of surgery in the acute phase, as suggested by the systematic review published by Song et al.(7). Such reasoning is fundamented not only upon this study - which has its limitations - but also on the data obtained with this technique by Muench et al.(8), who found the expected outcomes of the surgical treatment of such chronic lesions to be similar to those obtained in patients in whom initial conservative management proved effective.
Limitations
The present study has two important limitations: firstly, the number of included patients is limited, and this may cause infrequent complications (such as the aforementioned clavicular fractures) to go unnoticed. Nevertheless, the sample size does allows us to identify the improvements obtained on the functional scales as being significant and clinically relevant. Secondly, the duration of follow-up was insufficient. Although all patients were evaluated at least one year after surgery, the clinical outcomes could possibly worsen over longer periods of time. In particular, the presence of degenerative changes in the acromioclavicular joint observed in the radiographic studies at the end of follow-up appeared to have no functional repercussions, though in view of the young age of the patients, such changes might have consequences over the long term. In turn, it should be noted that among the individuals with correct initial reduction, no worsening at all was observed in the quality of reduction after 2.7 years of follow-up. Lastly, the clinical case series design of our study poses limitations compared with other studies that include a control group.
Conclusions
Satisfactory short-term outcomes were obtained with this anatomical technique that reconstructs the acromioclavicular and coracoclavicular ligament complexes with the help of a tendon allograft for the management of acromioclavicular dislocations with an evolution of over three weeks. In this small case series, the technique was seen to be safe, with no complications.
Figuras
Figure 1. Coracoclavicular distance measured from the anteroposterior radiograph of the shoulder. The data correspond to the affected side (preoperative) and the healthy side as reference. The described technique allowed recovery of normal coracoclavicular distance after surgery (postoperative) and at the end of follow-up (final). * Significant differences (p < 0.0001) with respect to the preoperative values. There were no significant differences among the postoperative, final and healthy side values.
Figure 2. An 18-year-old male presenting type V acromioclavicular dislocation initially subjected to conservative management. One year after the injury he presented persistent symptoms and absolute limitation for sports activities (A). Surgery was performed with good reduction of the deformity (B), and four years after the operation the functional outcome was excellent (C), with minimum degenerative changes in the acromioclavicular joint and some widening of the clavicular tunnels.
Figure 3. A 52-year-old woman with type IV acromioclavicular dislocation (A) subjected to surgery four weeks after injury due to refractory pain and dysfunction. The surgical outcome was considered acceptable, though with insufficient reduction (B). Fourteen months after surgery, the patient suffered persistent symptoms and loss of reduction was seen to have progressed (C).
Tablas
Información del artículo
Cita bibliográfica
Autores
Miguel Ángel Ruiz Ibán
Director de REACA
Cirugía Ortopédica y Traumatología. Unidad de Hombro y Codo. Hospital Universitario Ramón y Cajal. Madrid
Raquel Ruiz Díaz
Servicio de Cirugía Ortopédica y Traumatología, Hospital Universitario Ramón y Cajal, Madrid, España
Ignacio de Rus Aznar
Servicio de Cirugía Ortopédica y Traumatología. Clinica CEMTRO. Madrid
Unidad de Hombro y Codo. Hospital Universitario Ramón y Cajal. Madrid
Servicio de Cirugía Ortopédica y Traumatología. Hospital Monográfico Asepeyo Coslada. Madrid
Hospital Universitario de Torrejón. Madrid
Andrea Paniagua González
Unidad de Hombro y Codo. Hospital Fraternidad-Muprespa Habana. Madrid
Unidad de Hombro y Codo. Hospital Universitario Ramón y Cajal. Madrid
Cristina Victoria Asenjo Gismero
Equipo +Qtrauma. Hombro y Codo. Hospital Beata María Ana. Madrid
Unidad de Miembro Superior. Hospital FREMAP Majadahonda. Madrid
Cirugía Ortopédica y Traumatología, Hospital ASEPEYO, Coslada, Madrid, España
Rosa Ezquerro Cortés
Hospital Universitario Ramón y Cajal. Madrid
Hospital General Nuestra Señora del Prado. Talavera de la Reina, Toledo
Jorge Díaz Heredia
Cirugía Ortopédica y Traumatología. Unidad de Hombro y Codo. Hospital Universitario Ramón y Cajal. Madrid
Clínica La Antigua. Guadalajara
Editor asociado de REACA
Ethical responsibilities
Conflicts of interest. The authors state that they have no conflicts of interest.
Financial support. This study has received no financial support.
Protection of people and animals. The authors declare that the procedures carried out abided with the ethical standards of the responsible human experimentation committee and in accordance with the World Medical Association and the Declaration of Helsinki.
Data confidentiality. The authors declare that the protocols of their centre referred to the publication of patient information have been followed.
Right to privacy and informed consent. The authors have obtained informed consent from the patients and/or subjects cited in the article. The mentioned document is filed by the corresponding author.
Referencias bibliográficas
-
1Lemos MJ. The evaluation and treatment of the injured acromioclavicular joint in athletes. Am J Sports Med. 1998;26(1):137-44.
-
2Stucken C, Cohen SB. Management of acromioclavicular joint injuries. Orthop Clin North Am. 2015;46(1):57-66.
-
3Balke M, Schneider MM, Shafizadeh S, Bathis H, Bouillon B, Banerjee M. Current state of treatment of acute acromioclavicular joint injuries in Germany: is there a difference between specialists and non-specialists? A survey of German trauma and orthopaedic departments. Knee Surg Sports Traumatol Arthrosc. 2015;23(5):1447-52.
-
4Korsten K, Gunning AC, Leenen LP. Operative or conservative treatment in patients with Rockwood type III acromioclavicular dislocation: a systematic review and update of current literature. Int Orthop. 2014;38(4):831-8.
-
5Ruiz Ibán MA. The acromioclavicular joint: Lots of questions; Too many answers? Rev Esp Artrosc Cir Articul. 2015;22(1):1-2.
-
6Díaz Heredia J, Ruiz Díaz R, Valencia Mora M, Ruiz Ibán MA. ¿Por qué tratamiento conservador de las luxaciones acromioclaviculares tipo III? Rev Esp Artrosc Cir Articul. 2015;22:5.
-
7Song T, Yan X, Ye T. Comparison of the outcome of early and delayed surgical treatment of complete acromioclavicular joint dislocation. Knee Surg Sports Traumatol Arthrosc. 2016 Jun;24(6):1943-50.
-
8Muench LN, Berthold DP, Uyeki C, et al. Conversion to anatomic coracoclavicular ligament reconstruction (ACCR) shows similar clinical outcomes compared to successful non-operative treatment in chronic primary type III to V acromioclavicular joint injuries. Knee Surg Sports Traumatol Arthrosc. 2020 Jul 24. doi: 10.1007/s00167-020-06159-2. Epub ahead of print.
-
9Nolte PC, Lacheta L, Dekker TJ, Elrick BP, Millett PJ. Optimal Management of Acromioclavicular Dislocation: Current Perspectives. Orthop Res Rev. 2020;12:27-44.
-
10Weinstein DM, McCann PD, McIlveen SJ, Flatow EL, Bigliani LU. Surgical treatment of complete acromioclavicular dislocations. Am J Sports Med. 1995;23(3):324-31.
-
11Saccomanno MF, Marchi G, Mocini F, et al. Anatomic reconstruction of the coracoclavicular and acromioclavicular ligaments with semitendinosus tendon graft for the treatment of chronic acromioclavicular joint dislocation provides good clinical and radiological results. Knee Surg Sports Traumatol Arthrosc. 2020 Oct 27. doi: 10.1007/s00167-020-06285-x. Epub ahead of print.
-
12Kibler WB, Sciascia AD, Morris BJ, Dome DC. Treatment of Symptomatic Acromioclavicular Joint Instability by a Docking Technique: Clinical Indications, Surgical Technique, and Outcomes. Arthroscopy. 2017;33(4):696-708.
-
13Sircana G, Saccomanno MF, Mocini F, et al. Anatomic reconstruction of the acromioclavicular joint provides the best functional outcomes in the treatment of chronic instability. Knee Surg Sports Traumatol Arthrosc. 2020 May 27. doi: 10.1007/s00167-020-06059-5. Epub ahead of print.
-
14Ruiz Díaz R, Ruiz Ibán MA, de Rus Aznar I, et al. Técnica quirúrgica de reconstrucción anatómica abierta con aloinjerto para el tratamiento de las luxaciones acromioclaviculares crónicas. Rev Esp Artrosc Cir Articul. 2021;28(3):XXX-XXX.
-
15Carofino BC, Mazzocca AD. The anatomic coracoclavicular ligament reconstruction: surgical technique and indications. J Shoulder Elbow Surg. 2010;19(2 Suppl):37-46.
-
16Kibler WB, Sciascia A, Wilkes T. Scapular dyskinesis and its relation to shoulder injury. J Am Acad Orthop Surg. 2012;20(6):364-72.
-
17Ranne JO, Kainonen TU, Lehtinen JT, et al. Arthroscopic Coracoclavicular Ligament Reconstruction of Chronic Acromioclavicular Dislocations Using Autogenous Semitendinosus Graft: A Two-Year Follow-up Study of 58 Patients. Arthrosc Sports Med Rehabil. 2020;2(1):e7-e15.
-
18Cano-Martínez JA, Nicolás-Serrano G, Bento-Gerard J, Marín FP, Grau JA, Antón ML. Chronic acromioclavicular dislocations: multidirectional stabilization without grafting. JSES Int. 2020;4(3):519-31.
-
19Cerciello S, Berthold DP, Uyeki C, et al. Anatomic coracoclavicular ligament reconstruction (ACCR) using free tendon allograft is effective for chronic acromioclavicular joint injuries at mid-term follow-up. Knee Surg Sports Traumatol Arthrosc. 2020 Jun 30. doi: 10.1007/s00167-020-06123-0. Epub ahead of print.
-
20Hunter TJ, Abdus-Samee M, Balasubramanian S, Grocott N, McClelland D. Medium- to long-term results of acromioclavicular joint stabilisation using the Ligament Augmentation Reconstruction System (LARS) ligament. Shoulder Elbow. 2020;12(3):163-9.
-
21Borbas P, Churchill J, Ek ET. Surgical management of chronic high-grade acromioclavicular joint dislocations: a systematic review. J Shoulder Elbow Surg. 2019;28(10):2031-8.
-
22Berthold DP, Muench LN, Dyrna F, et al. Radiographic alterations in clavicular bone tunnel width following anatomic coracoclavicular ligament reconstruction (ACCR) for chronic acromioclavicular joint injuries. Knee Surg Sports Traumatol Arthrosc. 2020 Apr 25. doi: 10.1007/s00167-020-05980-z. Epub ahead of print.
Descargar artículo:
Licencia:
Este contenido es de acceso abierto (Open-Access) y se ha distribuido bajo los términos de la licencia Creative Commons CC BY-NC-ND (Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional) que permite usar, distribuir y reproducir en cualquier medio siempre que se citen a los autores y no se utilice para fines comerciales ni para hacer obras derivadas.
Comparte este contenido
En esta edición
- Don’t forget to remember
- Anatomical study on subtalar arthrodesis: anterolateral versus posterior portals
- Customized 3D printed guides for the repair of rupture of the posterior root of the internal meniscus. Preliminary outcomes
- Anatomical ligament reconstruction with allograft in chronic acromioclavicular dislocations restores joint stability and function. Short-term outcomes in 14 cases
- Patellar tendinopathy: diagnostic approach and functional assessment scales
- Current management of posterior cruciate ligament rupture. A narrative review
- Management of anterior instability of the shoulder with bone defects
- Open anatomical reconstruction surgical technique with allograft for the treatment of chronic acromioclavicular dislocations
- Simultaneous but different damage to both posterior meniscus roots with multiple ligament injury of the knee following high-energy trauma. Presentation of a case
- Pigmented villonodular synovitis of the ankle
Más en PUBMED
Más en Google Scholar
Más en ORCID


Revista Española de Artroscopia y Cirugía Articular está distribuida bajo una licencia de Creative Commons Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional.