Residual instability after reconstruction surgery of the anterior cruciate ligament. What are we missing?
Inestabilidad residual tras cirugía de reconstrucción del ligamento cruzado anterior. ¿Qué estamos pasando por alto?
Resumen:
Pese a la mejora en las técnicas de reconstrucción del ligamento cruzado anterior (LCA), continúa habiendo un número de pacientes que presentan inestabilidad rotacional residual y pivot shift postoperatorio. Esto ha llevado a buscar las causas que puedan justificar la presencia de esta inestabilidad en otras estructuras de la rodilla y en la propia morfología ósea. Así, se ha retomado el interés por las estructuras anterolaterales de la rodilla, pero también por el papel estabilizador de los meniscos, el tratamiento adecuado de las lesiones asociadas de los ligamentos colaterales y la importancia del eje de la extremidad en casos de revisión y también en primarios.
No se puede hablar ya solo de cirugía de reconstrucción del LCA, sino de cirugía de la inestabilidad de rodilla, debiendo considerar el resto de las estructuras que pueden estar afectadas y que necesitarán un correcto tratamiento. Diagnosticar y tratar adecuadamente las lesiones ligamentosas, meniscales y óseas asociadas a la rotura del LCA es una obligación para el cirujano de rodilla.
Se presenta un resumen del webinar realizado sobre la cuestión por la Asociación Española de Artroscopia (AEA) y LATAM.
Abstract:
Despite improvement of the reconstruction techniques of the anterior cruciate ligament (ACL), a number of patients continue to present residual rotational instability and pivot shift following surgery. This has led to a search for the causes of such instability in other structures of the knee and in the bone morphology itself. In this respect, there has been renewed interest in the anterolateral structures of the knee, but also in the stabilizing role of the menisci, adequate treatment of the associated lesions of the collateral ligaments, and the importance of the axis of the extremity in cases of revision surgery and also in primary surgery.
It is no longer possible to speak only of reconstruction surgery of the ACL; we now must refer to surgery of instability of the knee, with consideration of the rest of the structures that may be affected and which will need correct treatment. Diagnosing and adequately treating the ligamentous, meniscal and bony lesions associated to ACL rupture is mandatory for the knee surgeon.
A summary is presented of the webinar on this topic by the Spanish Association of Arthroscopy (Asociación Española de Artroscopia [AEA]) and LATAM.
Introduction
Surgery of the anterior cruciate ligament (ACL) remains one of the most frequent surgeries in diseases of the knee. In recent years there has been a transition from transtibial non-anatomic techniques, which placed the plasty in a vertical position, near the rotation axis of the knee, towards independent or anatomic femoral tunnel techniques.
Although the general impression among surgeons is that better outcomes are obtained with these techniques, the data found in the literature are unable to confirm their superiority(1). In addition, a number of patients continue to present residual rotational instability and pivot shift following surgery, despite well performed anatomic reconstruction(2).
This has led to a search for the causes of such residual instability in other structures of the knee and in the bone morphology itself. In this respect, there has been renewed interest in the anterolateral structures and anterolateral ligament (ALL)(3), but also in the stabilizing role of the menisci, and specifically those rupture patterns resulting in important loss of this function, such as rupture of the posterior ramp of the medial meniscus and ruptures of the posterior root - concretely that of the external meniscus in the context of ACL rupture(4). The most adequate treatment for the associated lesions of the collateral ligaments - a well known cause of failure after ACL surgery - is currently being updated. On the other hand, the bone morphology of the joint, especially tibial deformity in the coronal (varus-valgus) and sagittal plane (posterior tibial ramp), and its role in recurrent ruptures and multi-ligament injuries, have gained special importance in recent years(5).
The aim of this webinar was therefore to gain a more in-depth view of those associated lesions that may condition the prognosis of our patients with ACL injuries, and of which surgical procedures we should add to our intraarticular reconstructions - assuming that these have been well performed - in order to improve our outcomes and limit the risk of residual instability and recurrent rupture.
Importance of the collateral ligaments in residual instability
Antonio Cruz Cámara
Combined ACL / medial side injury is the most frequent combination of all ligament injuries of the knee (6.7%), while the association ACL / lateral side only accounts for 0.4%(6). Getelman et al. reported that 15% of their 26 cases of ACL revision surgery were due to associated instabilities of the collateral ligaments(7).
Anterior cruciate ligament / medial complex
Anatomically, the most relevant structures on the medial side of the knee are the medial collateral ligament (MCL), with its superficial (MCLs) and deep (MCLd) components, and the posterior oblique ligament (POL). The MCL is the most important primary static stabilizer for valgus and external rotation, while the POL is the primary stabilizer of internal rotation. Dynamically, the semimembranosus muscle is the most important structure.
Diagnosis
In the context of the physical examination, manoeuvres that cause us to suspect associated instabilities of this kind are an abnormally increased Lachman test and pivot shift, an anterior drawer test increased to 15º of external rotation, and a valgus stress test at 0º. In 1968, Slocum and Larson described(8) the modification of the anterior drawer test with 15º of external rotation that causes an increase in anterior translation at the expense of the medial tibial plateau for the diagnosis of anteromedial rotatory instability (AMRI). It also must be taken into account that a dial test may be positive at 30º not only in lesions of the posterolateral angle of the knee, but also in lesions of the medial side, at the expense of an increase in external rotation in the medial plateau.
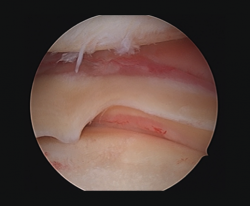
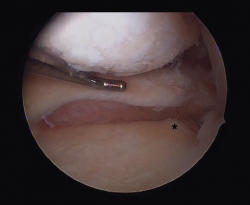
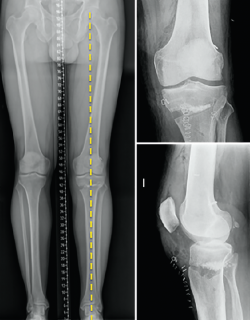
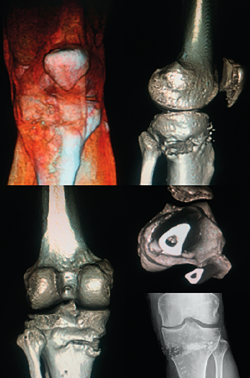
Other tests that contribute to the diagnosis are stress valgus radiographs (local anesthesia infiltration is advised in order not to underestimate the test), magnetic resonance imaging (MRI) and arthroscopic exploration (Figure 1).
Treatment
Although biomechanical studies warrant the reconstruction of combined ACL / medial lesions(9), satisfactory clinical outcomes have been reported with conservative management of the medial complex, supporting the idea that surgery of the MCL is not needed(10). Locations in the middle and proximal third afford better results. There is also controversy regarding the possibly greater incidence of mobility alterations and arthrofibrosis in the surgically treated cases(11).
It is generally accepted that low grade (I-II) lesions of the MCL can be managed on a conservative basis with an initial orthosis followed by deferred reconstruction of the ACL after 4-6 weeks, thus allowing healing of the MCL and complete recovery of the range of motion of the joint(12). Exploration under anesthesia, before and after reconstruction of the ACL, will serve as a guide to decide whether the MCL requires treatment or not. Severe valgus laxity after 6 weeks should cause us to consider the need for additional surgical treatment of the MCL.
No prospective studies comparing repair versus reconstruction of the MCL are found in the literature(13). Satisfactory outcomes have been reported with both approaches. Likewise, there is no strong evidence supporting reconstruction over repair. The general impression is that many surgeons prefer repair in acute avulsions and reconstruction in subacute or chronic scenarios. The recommendation is to attempt repair, if allowed by the quality of the tissues.
In reconstruction of the medial complex of the knee, the structures we seek to reproduce are the MCLs and the POL. We can consider reconstructions in one or two bands depending on whether we want to better stabilize the valgus / external rotation component or the anterior tibial translation(9). According to Stannard, the key to controlling rotational instability (atraumatic, multidirectional, bilateral, rehabilitation, inferior capsular shift [AMBRI]) is the POL(14); the triangular configuration formed by the MCL, the POL and the semimembranosus must be restored. We can choose between anatomic reconstructions such as that of LaPrade(15) and non-anatomic reconstructions. Authors such as Fanelli combine posteromedial capsular re-tensing(16).
Anterior cruciate ligament / lateral complex
Anatomically, the three most important structures are the lateral collateral ligament (LCL), the popliteus tendon (PT) and the popliteofibular ligament (PFL). The LCL is the first varus restrictor, particularly at 30º, and the external rotation restrictor at the same degrees of flexion. The role of the popliteal complex (PT / PFL) is to restrict external rotation at 60º of flexion, and also posterior translation motion of the tibia.
Diagnosis
The diagnostic indicators in the physical examination of a combined ACL / lateral lesion are an association of the tests specific of each type of injury (Lachman test, pivot shift, dial test at 30º, posterolateral drawer test at 30º, stress varus test at 0º, external rotation recurvatum test). An anterior drawer manoeuvre with 30º of internal rotation causing an increase in anterior translation at the expense of the lateral tibial plateau was described by Slocum and Larson as a test specific of this association(8).
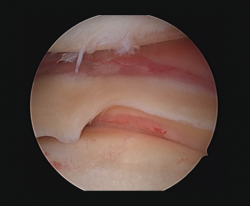
Other diagnostic tests are radiographs under stress varus conditions. We can find indirect radiological signs such as Segond fracture and the arcuate sign. MRI is of great help. Gelber et al. recently reported that over 80% of a group of world experts in the treatment of posterolateral angle injuries agree on the usefulness of MRI in the diagnosis of these lesions(17). Lastly, arthroscopy can offer additional information in the surgical cases (Figure 2).
Treatment
In contrast to combined ACL / medial injuries, in the case of combined ACL / lateral injuries conservative management would only be indicated for low grade lesions. The literature warrants surgery for grade 2-3 lesions of the posterolateral complex associated to the ACL(17).
The aim of surgery is to restore varus stability, external rotation and posterior translation according to the individualized assessment of each case. It is not always necessary to reconstruct the entire complex; the decision depends on the affected structures. The classification of Fanelli is very useful for assessing lesion grade and as a surgical indicator (18).
There is great variability in the world surgical community regarding the management of lesions of the posterolateral angle(17). The current tendency is to perform anatomic reconstructions that can be differentiated into techniques based on the fibula or the tibia. There is no evidence of superior outcomes with one technique or other. Minimally invasive approaches have now been introduced based on percutaneous and arthroscopic techniques, though they are not advisable in inexperienced hands. In acute cases, and even if reconstruction is performed, we always must try to repair the associated meniscal-capsular lesions and reinsert proximal avulsion of the popliteus and distal biceps muscle when present.
Meniscal disease and residual instability
Daniel Cansino Muñoz-Repiso
There are two meniscal injuries associated in biomechanical studies to the presence of residual instability following reconstruction of the ACL: meniscal ramp lesions and meniscal root lesions - fundamentally of the posterior root of both menisci.
Meniscal ramp lesions
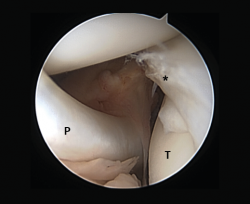
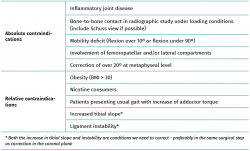
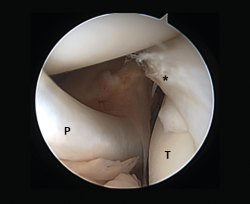
Although recently greater importance is being placed on the presence of so-called meniscal ramp lesions (Figure 3), with an estimated incidence of up to 23.9%(19) associated to ACL rupture, these lesions were already described by Strobel(20) in 1988 as a particular type of meniscal injury associated to ACL rupture and affecting the peripheral insertion of the posterior horn of the medial meniscus. These injuries are also referred to as hidden lesions of the posterior horn of the medial meniscus, since they may go undetected in the MRI studies(21). From the biomechanical perspective, ramp lesions of the knee with ACL rupture increase anterior translation of the tibia, internal and external rotation, and pivot shift. If not repaired, rotational stability following reconstruction of the ligament likewise is not fully restored(22).
Diagnosis
No clinical test is currently available allowing us to suspect the presence of these lesions. Magnetic resonance imaging is the diagnostic technique of choice, with the description of two signs associated to this disorder: the presence of an irregularity at the posterior margin of the medial meniscus, and the presence of joint fluid in the space between the posterior horn and the capsule(21). It has also been shown that the presence of edema in the posterior zone of the medial tibial plateau increases the probability of a meniscal ramp lesion(23). The definitive diagnosis is based on the arthroscopy findings. Authors such as Sonnery-Cottet(24) have described a systematic surgical exploration protocol to prevent such lesions from going undetected. In this exploration they recommend the use of a posteromedial port in order to allow improved visualization and even use a palpator probe to test the presence of these lesions, which are sometimes covered by a kind of membrane.
Treatment
Although the repair of ramp lesions improves joint laxity as evidenced by studies in cadavers(25), there is currently no clear consensus regarding which of these lesions should be repaired. In a prospective study published by X. Liu et al.(26), involving 73 patients, a total of 40 lesions were sutured with an all-inside technique, while another 33 simply underwent trephination - no significant differences in outcome being observed by MRI. The same authors published the functional outcomes in these patients with stable lesions - no significant differences being observed after two years in terms of the Lysholm scale, the International Knee Documentation Committee Knee (IKDC) form, the pivot shift and the Lachman test (KT-1000) between the two groups(27).
In relation to the surgical techniques, basically two have been described: all-inside suturing with preloaded suture systems(28) and the indirect suture technique using suture passer systems(29). Trans-notch vision or trans-septal vision can be used in either technique.
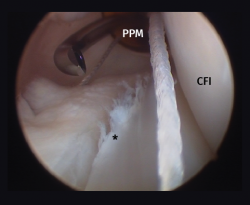
Meniscal root lesions
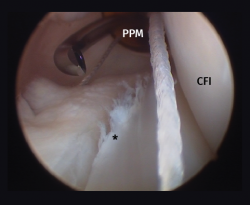
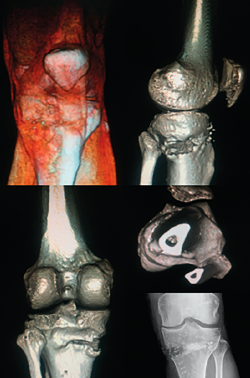
Meniscal root lesions are lesions located at less than 1 cm from the bone insertion of the meniscus, or lesions that involve bone avulsion of the anchoring zone (Figure 4). While lesions of the posterior root of the medial meniscus are related to degenerative processes, lesions of the posterior root of the external meniscus are associated to lesions of the ACL (7-12%)(30). Rupture of the posterior root of the medial meniscus biomechanically behaves like a total meniscectomy(31), while rupture of the posterior root of the external meniscus associated to ACL rupture results in an increase in anterior translation of the tibia and adds increased rotational instability, incrementing pivot shift(32).
Diagnosis
From the clinical perspective, these lesions should be suspected in the presence of Lachman scores of 3+ and pivot shift. High field MRI has been shown to be the diagnostic imaging test with the greatest sensitivity and specificity(33). Three radiological signs are associated to damage to the posterior root: 1) a hyperintense signal perpendicular to the meniscal root in the axial plane; 2) a vertical lineal defect over the meniscal root (truncation sign), which is associated to a meniscal extrusion of over 3 mm; and 3) the "ghost sign", representing the absence of meniscus in the sagittal plane in the zone of the posterior root(34,35).
Treatment
Repair of the posterior root of the external meniscus, in the setting of ACL repair, is essential in order to avoid residual instabilities and reduce plasty tension(36). Conservative management is indicated in elderly patients suffering from important osteoarthrosis, with the prescription of analgesics and changes in daily life activities.
Meniscectomy is an option in patients that have not responded to conservative management, though the benefits are only short term, since osteoarthrosis will advance more rapidly(35). Whenever possible, repair of the posterior root is the treatment of choice in order to avoid residual instability and early development of osteoarthrosis. The two most commonly described techniques are all-inside repair with side-to-side direct suturing(4), and the transtibial pull-out technique, where a transtibial tunnel is used to pass several sutures to the free margin of the meniscal root, affixing them in the anterior cortical layer of the tibia by means of a cortical anchoring system(37).
Axis and osteotomies in the treatment of residual instability
Fernando Martínez Delgado
One of the aspects often not adequately taken into account when considering the surgical management of knee instability is the influence of the loading axes upon the instability itself. A varus morphotype or axis associated to anterior instability due to ACL deficit tends to be the most frequent combination.
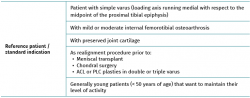
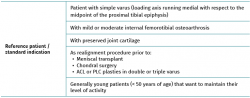
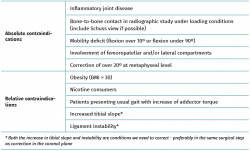
Correction of the loading axis by means of a valgus-producing tibial osteotomy (VTO) was a very common procedure in the 1990s in Departments of Orthopedic Surgery and Traumatology, but has now become a practically residual option for most specialists. Valgus-producing tibial osteotomy is no longer considered an option in the management of advanced gonarthrosis. At present, VTO is a tool for treating instability and a preventive measure against joint degeneration (Tables 1 and 2).
Effect of the tibial slope upon the anterior cruciate ligament
The effect of the tibial slope upon instability is well known and used in veterinary surgery: an increased slope favours anterior instability, while a reduced or inverted slope favours posterior instability. Recent studies have confirmed the negative effect of an increased tibial slope upon ACL reconstruction plasties(38). This would be a factor to be taken into account, fundamentally in ACL revision surgery. In this regard, there are authors such as Dejour(39) who recommend a supra-tuberosity deflecting tibial osteotomy in second revision surgeries, provided the slope exceeds 12º. Monllau et al.(5) have published their technical variant with the osteotomy in "inverted L" shape, in which varus and slope are corrected. In any case, the correction of both aspects simultaneously poses a challenge, and requires careful preoperative planning.
Effect of varus deformity upon the anterior cruciate ligament
Different studies have shown that deformity of the coronal axis in varus considerably increases loading upon the ACL(40). Mechanical varus of 10º implies an overload of over 400% upon the ACL at 30º of knee flexion or 100% in extension. Minor deviations of the neutral mechanical axis, even slightly above "physiological" varus, such as 5º, already imply an increase in stress upon the ACL (250% at 30º and 68% in extension).
In addition, mention must be made of the high prevalence of meniscal damage associated to ACL lesions(41,42), due to simultaneous damage to both structures, or as a consequence of stress secondary to the instability. Therefore, the combination of varus and anterior instability defines a harmful pattern requiring the consideration of single-step resolution of both situations when marked varus is associated to anterior instability(43).
Technical aspects
A number of aspects should be taken into account when considering the correction angle of our osteotomy (patient age, constitutional morphotype, bilaterality of the condition, level of joint degeneration in the medial compartment, condition of the lateral compartment). The multifactorial analysis of these elements will lead us to consider whether slight hyper-correction should be performed (with the Fujisawa point(44) as reference, for example), or whether a normo-corrective osteotomy is indicated(45).
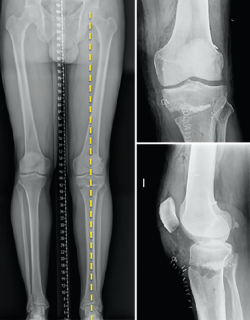
We should bear in mind that although the indication of osteotomy resides in varus correction (coronal plane), the osteotomy will also affect the sagittal and axial planes (Figure 5).
Type of osteotomy
In recent decades, medial opening wedge osteotomy has become the reference technique, due to its lesser morbidity, rapid consolidation and quick patient recovery(46). An important aspect is that it requires no intervention upon the fibula or the proximal tibiofibular joint. Other possibilities such as lateral subtraction wedge osteotomy or dome osteotomy have been displaced as a result of the good outcomes afforded by the medial addition wedge.
The osteotomy plane in the sagittal aspect is a crucial point for avoiding undesired modifications of the posterior tibial slope or for correcting it where indicated (the more posterior we position the base of the wedge, the greater the correction of the posterior slope). Because of the triangular shape of the section of the proximal tibial metaphysis, it is complicated to geometrically plan the wedge allowing the exact desired correction in the two planes. Some authors report good outcomes with customized cutting guides(47,48), but the results focus on correction in the coronal plane, not the sagittal plane.
Fixation system
Implant selection is a crucial factor for facilitating rapid patient recovery and an early start of weight-bearing. The choice should seek to ensure that the osteosynthesis system allows loading and can support the high compression and shear forces to which it will be exposed. In recent years titanium or PEEK (polyethyl ether ketone) plates with locking screws and even PEEK wedges have become popular, due to their great resistance to compression and biocompatibility(49) (Figure 6).
Anterolateral plasties associated to reconstruction of the anterior cruciate ligament
Juan Blanco Novoa
The need for anterolateral plasties in the setting of ACL insufficiency is based on the fact that after reconstruction, the presence of a positive pivot shift is observed in up to 20-25% of all cases(50) . On the other hand, all the anatomic reconstructions we perform are unable to fully restore the native biomechanics, with poor control of the generated residual rotational instability. In some situations we could assume that there is a greater risk of such instability, with the consequent presence of repeat rupture of our plasties: in primary cases in young individuals (under 18 years of age) with great pivoting activity demands, hyperlaxity-genu recurvatum, in cases of very marked preoperative pivot shift, and in rescue surgeries(51).
The performance of extra-articular plasties originated long ago, even before the generalization of arthroscopic treatments, with the descriptions of Lemaire (1970) or Macintosh (1971). They were subsequently abandoned on the grounds that they generated a pressure increase in the external compartment, with the consequent risk of producing secondary osteoarthrosis of the latter. However, it was not until publication of the anatomic study by the Belgian group of Steven Claes(3), in 2013, on the ALL, when importance was again attributed to the structures that contribute to rotational control of the native and reconstructed ACL. In 97% of 41 cadaver specimens, these authors identified a structure which they referred to as ALL, attributing it with biomechanical importance in the control of internal rotation between 30º and 90º of flexion. They initially described a series of anatomic insertion points and a definition which later studies and research groups modified, leading to what we currently take as being valid.
In this sense, a consensus group was established in 2019, studying the anterolateral complex (ALC) and clearly defining its anatomy, biomechanical function and the indications for its reconstruction(52). The following conclusions are drawn from that study:
- Anatomic. The ALL is a structure that forms part of the ALC, with a consistency that varies between subjects and which extends from a point located proximal and posterior to the lateral epicondyle, runs superficial to the LCL, relates to the lateral meniscus, and inserts at a point intermediate between the anterior margin of the fibular head and the posterior margin of Gerdy's tubercle. From superficial to in-depth, the mentioned complex is composed of a superficial iliotibial band with its patellar portion and a deep band with the proximal, distal and retrocondylar Kaplan fibres - the ALL being located in the deepest layer of the ALC.
- Biomechanical. The first stabilizer of anterior translation and internal rotation close to extension is the ACL, while the secondary stabilizers would be the iliotibial band with the Kaplan fibres, the external meniscus and the ALL - the latter being anisometric.
- Indications. Basically, at the present time it would be advisable in rescue surgery, high grade pivot shift, ligament hyperlaxity-genu recurvatum and in young individuals with great pivoting activity demands.
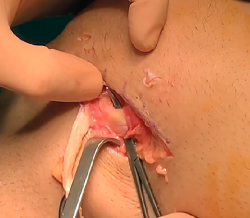
There are currently two options for performing anterolateral plasties in these cases(53): modified Lemaire or reconstruction with ALL augmentation plasty. Without entering the debate as to which option is best, since the initially proposed ALL reconstructions are not anatomic, it appears to be important to perform plasty fixation in full extension(54,55). The modified Lemaire technique in turn involves taking, on a minimally invasive basis (Figure 7) and with good dissection, 10 cm of band measuring 1 cm in width, pivoting in depth to the LCL and performing fixation in a zone proximal and posterior to the epicondyle. The technique is simple, adds no more than 10 minutes to reconstruction of the ACL, and affords satisfactory control of rotational instability(56). With regard to reconstruction of the ALL, we follow the previously described anatomic principles and the descriptions of the French group of Sonnery-Cottet(57) (Figure 8). In this case we would use the gracilis muscle as graft, demonstrating a decrease in the incidence of recurrent rupture in young patients in which this technique is added(58). This technique may be an option in cases of all-inside reconstruction using only the tendon of the semimembranosus muscle quadrupled for reconstruction of the ACL, and leaving the tendon of the gracilis muscle for anatomic reconstruction of the ALL.
Long-term studies have evidenced no increase in osteoarthrosis as a result of such plasties. Degeneration of the external compartment could be related to fixation of the graft with excessive tension or in external rotation(59,60) and with management of the associated external meniscus lesions with resection.
Conclusions
At present, we cannot speak of reconstruction surgery of the ACL; we now must refer to surgery of instability of the knee, for as has been mentioned, there are multiple associated lesions that must be taken into account and adequately treated during surgery. The implications in relation to the outcomes, the risk of recurrent rupture and the need for revision surgery in some of these surgical manoeuvres might not (yet) be evident, but this should not deviate us from our wish to offer the best possible treatment for our patients. Performing these treatments of the injuries associated to ACL rupture also has an impact in terms of the total cost of surgery, since more implants and surgery time are needed. Here again, however, we should not overly simplify things. Diagnosing and adequately treating the ligamentous, meniscal and bony lesions associated to ACL rupture is mandatory for the knee surgeon.
Figuras
Figure 1. Arthroscopic view through the anterolateral port of a positive drive-through sign with abnormal aperture of the internal compartment secondary to insufficiency of the medial collateral ligament. Right knee.
Figure 2. Arthroscopic view through the anterolateral port of damage to the meniscus-popliteal ligaments (*) at the level of the popliteal hiatus, leaving the tibia exposed (T). P: tendon of the popliteus muscle. Right knee.
Figure 3. Repair of a lesion of the posterior ramp of the medial meniscus (*) adopting a posteromedial arthroscopic approach. Trans-notch view from the anterolateral port. Working cannula in the posteromedial port (PMP). IFC: internal femoral condyle. Right knee.
Figure 4. Rupture of the posterior root of the medial meniscus. Note the lack of continuity in the posterior horn of the medial meniscus, exhibiting a space between the root and its insertion imprint in the tibia (*). Left knee; view from the anterolateral port.
Figure 7. Modified Lemaire extraarticular anterolateral plasty. Dissection under the lateral collateral ligament. Note the graft already sectioned from the iliotibial band.
Figure 8. Anatomic reconstruction of the anterolateral ligament. Selection of the insertion points, posterior and proximal to the lateral epicondyle in the femur and between Gerdy's tubercle and the fibular head in the tibia.
Tablas
Información del artículo
Cita bibliográfica
Autores
Diego García-Germán Vázquez
Servicio de Cirugía Ortopédica y Traumatología. Hospital Universitario HM Torrelodones. Universidad San Pablo CEU. Torrelodones. Madrid
Clínica DKF. Madrid
Servicio de Cirugía Ortopédica y Traumatología. Hospital Central de la Cruz Roja San José y Santa Adela. Madrid
Servicio de Cirugía Ortopédica y Traumatología. Hospital Universitario Puerta de Hierro-Majadahonda. Majadahonda. Madrid
Silvio Villaescusa Marín
Hospital Clínico Universitario Virgen de la Arrixaca
Policlínica Volta
Federación Murciana de Fútbol. Murcia
Juan Blanco Novoa
Clínica Trauma Sport. Ourense
Complexo Hospitalario Universitario de Ourense
Daniel Cansino Múñoz-Repiso
Centro Médico La Corredera. Sevilla
Antonio Cruz Cámara
Hospital Santa Clotilde-Federación Cántabra de Fútbol. Santander
Clínica La Cañía. Santander
Fernando Martínez Delgado
Hospital Universitario Miguel Servet. Zaragoza
Ethical responsibilities
Conflicts of interest. The authors state that they have no conflicts of interest.
Financial support. This study has received no financial support.
Protection of people and animals. The authors declare that this research has not involved studies in humans or in animals.
Data confidentiality. The authors declare that the protocols of their centre referred to the publication of patient information have been followed.
Right to privacy and informed consent. The authors declare that no patient data appear in this article.
Referencias bibliográficas
-
1MacDonald P, Kim C, McRae S, Leiter J, Khan R, Whelan D. No clinical differences between anteromedial portal and transtibial technique for femoral tunnel positioning in anterior cruciate ligament reconstruction: a prospective randomized, controlled trial. Knee Surg Sports Traumatol Arthrosc. 2018;26:1335-42.
-
2Ayeni OR, Chahal M, Tran MN, Sprague S. Pivot shift as an outcome measure for ACL reconstruction: a systematic review. Knee Surg Sports Traumatol Arthrosc. 2012;20:767-7.
-
3Claes S, Vereecke E, Maes M, Victor J, Verdonk P, Bellemans J. Anatomy of the anterolateral ligament of the knee. J Anat. 2013;223:321-8.
-
4Ahn JH, Lee YS, Chang JY, Chang MJ, Eun SS, Kim SM. Arthroscopic all inside repair of the lateral meniscus root tear. Knee. 2009;16:77-80.
-
5Monllau JC, Erquicia JI, Ibáñez F, Ibáñez M, Gelber P, Masferrer-Pino A, Pelfort X. Open-wedge valgus high tibial osteotomy technique with inverted L-shaped configuration. Arthroscopy Tech. 2017;13:e2161-7.
-
6Jari S, Shelbourne KD. Nonoperative or delayed surgical treatment of combined cruciate ligaments and medial side knee injuries. Sports Med Arthrosc Rev. 2001;9:185-92.
-
7Getelman MH, Schepsis AA, Zimmer J. Revision ACL reconstruction: autograft versus allograft. Arthroscopy. 1995;11:378.
-
8Slocum DB, Larson RL. Rotatory instability of the knee. Its pathogenesis and a clinical test to demonstrate its presence. J Bone Joint Surg Am. 1968;50:211-25.
-
9Zhu J, Dong J, Marshall B, Linde MA, Smolinski P, Fu F. Medial colateral ligament reconstruction is necessary to restore anterior stability with anterior cruciate and collateral ligament injury. Knee Surg Sports Traumatol Arthrosc. 2018;26:550-7.
-
10Zaffagnini S, Bonanzinga T, Marcheggiani Muccioli GM, Giordano G, Bruni D, Bignozzi S, et al. Does chronic medial collateral ligament laxity influence the outcome of anterior cruciate ligament reconstruction?: a prospective evaluation with a minimum three-year follow-up. J Bone Joint Surg Br. 2011 Aug;93(8):1060-4.
-
11Zhang H, Sun Y, Han X, Wang Y, Wang L, Alquhali A, Bai X. Simultaneous Reconstruction of the Anterior Cruciate Ligament and Medial Collateral Ligament in Patients with Chronic ACL-MCL Lesions. Am J Sports Med. 2014;42:1675-81.
-
12Kovachevich R, Shah JP, Arens AM, Stuart MJ, Dahm DL, Levy B. Operative management of the medial collateral ligament in the multi-ligament injured knee: an evidence-based systematic review. Knee Surg Sports Traumatol Arthrosc. 2009;17:823-29.
-
13Gelber PE, Drager J, Maheshwer B, Leyes M, Barenius B, Robinson J, et al. Large variability exists in the management of posterolateral corner injuries in the global surgical community. Knee Surg Sports Traumatol Arthrosc. 2020;28:2116-23.
-
14Stannard JP, Black BS, Azbell C, Volgas DA. Posteromedial corner injury in knee dislocations. J Knee Surg. 2012;25:429-34.
-
15Fanelli GC. Evaluation and treatment of medial instability of the knee. Sports Med Arthrosc Rev. 2015 Jun;23(2):61-2.
-
16Laprade RF, Wijdicks CA. Surgical technique: development of an anatomic medial knee reconstruction. Clin Orthop Relat Res. 2012;470:806-14.
-
17Krukhaug Y, Mølster A, Rodt A, Strand T. Lateral ligament injuries of the knee. Knee Surg Sports Traumatol Arthrosc. 1998;6(1):21-5.
-
18Fanelli GC, Larson RV. Practical management of posterolateral instability of the knee. Arthroscopy. 2002;18:1-8.
-
19Sonnery-Cottet B, Praz C, Rosenstiel N, Blakeney WG, Ouanezar H, Kandhari V, et al. Epidemiological Evaluation of Meniscal Ramp Lesions in 3214 Anterior Cruciate Ligament-Injured Knees From the SANTI Study Group Database: A Risk Factor Analysis and Study of Secondary Meniscectomy Rates Following 769 Ramp Repairs. Am J Sports Med. 2018;46:3189-97.
-
20Strobel M. Manual of Arthroscopic Surgery. New York, NY: Springer; 1988.
-
21Yeo Y, Ahn JM, Kim H, Kang Y, Lee E, Lee JW, Kang HS. MR evaluation of the meniscal ramp lesion in patients with anterior cruciate ligament tear. Skeletal Radiol. 2018;47:1683-9.
-
22DePhillipo NN, Moatshe G, Brady A, Chahla J, Aman ZS, Dornan GJ, et al. Effect of Meniscocapsular and Meniscotibial Lesions in ACL-Deficient and ACL-Reconstructed Knees: A Biomechanical Study. Am J Sports Med. 2018 Aug;46(10):2422-31.
-
23Kumar NS, Spencer T, Cote MP, Arciero RA, Edgar C. Is Edema at the Posterior Medial Tibial Plateau Indicative of a Ramp Lesion? An Examination of 307 Patients With Anterior Cruciate Ligament Reconstruction and Medial Meniscal Tears. Orthop J Sports Med. 2018;6:1-6.
-
24Sonnery-Cottet B, Conteduca J, Thaunat M, Gunepin FX, Seil R. Hidden lesions of the posterior horn of the medial meniscus: a systematic arthroscopic exploration of the concealed portion of the knee. Am J Sports Med. 2014;42:921-6.
-
25Stephen JM, Halewood C, Kittl C, Bollen SR, Williams A, Amis AA. Posteromedial meniscocapsular lesions increase tibiofemoral joint laxity with anterior cruciate ligament deficiency, and their repair reduces laxity. Am J Sports Med. 2016;44:400-8.
-
26Liu X, Feng H, Hong L, Zhang H. [A prospective randomized control trial of arthroscopic surgery for stable ramp lesion of the medial meniscus]. Zhonghua Wai Ke Za Zhi. 2017;55:161-5.
-
27Liu X, Zhang H, Feng H, Hong L, Wang XS, Song GY. Is It Necessary to Repair Stable Ramp Lesions of the Medial Meniscus During Anterior Cruciate Ligament Reconstruction? A Prospective Randomized Controlled Trial. Am J Sports Med. 2017;45:1004-11.
-
28Negrín R, Reyes NO, Íñiguez M, Pellegrini JJ, Wainer M, Duboy J. Meniscal Ramp Lesion Repair Using an All-Inside Technique. Arthrosc Tech. 2018;7:e265-e270.
-
29Buyukdogan K, Laidlaw MS, Miller MD. Meniscal ramp lesion repair by a trans-septal portal technique. Arthrosc Tech. 2017;6:e1379-e1386.
-
30Tang X, Marshall B, Wang JH, Zhu J, Li J, Smolinski P, Fu FH. Lateral Meniscal Posterior Root Repair With Anterior Cruciate Ligament Reconstruction Better Restores Knee Stability. Am J Sports Med. 2019 Jan;47(1):59-65.
-
31Allaire R, Muriuki M, Gilbertson L, Harner CD. Biomechanical Consequences of a Tear of the Posterior Root of the Medial Meniscus: Similar to Total Meniscectomy. J Bone Joint Surg Am. 2008;90:1922-31.
-
32Frank JM, Moatshe G, Brady AW, Dornan GJ, Coggins A, Muckenhirn KJ, et al. Lateral Meniscus Posterior Root and Meniscofemoral Ligaments as Stabilizing Structures in the ACL-Deficient Knee: A Biomechanical Study. Orthop J Sports Med. 2017;5(6):232596711769575.
-
33LaPrade RF, Ho CP, James E, Crespo B, LaPrade CM, Matheny LM. Diagnostic accuracy of 3.0 T magnetic resonance imaging for the detection of meniscus posterior root pathology. Knee Surg Sports Traumatol Arthrosc. 2015;23:152-7.
-
34Harper KW, Helms CA, Lambert HS, Higgins LD. Radial Meniscal Tears: Significance, Incidence, and MR Appearance. Am J Roent. 2005;185:1429-34.
-
35Pache S, Aman ZS, Kennedy M, Nakama GY, Moatshe G, Zeigler C, LaPrade RF. Meniscal Root Tears: Current Concepts Review. Arch Bone Jt Surg. 2018;6:250-9.
-
36Ahn JH, Lee YS, Chang JY, Chang MJ, Eun SS, Kim SM. Arthroscopic all inside repair of the lateral meniscus root tear. Knee. 2009;16:77-80.
-
37LaPrade RF, Matheny LM, Moulton SG, James EW, Dean CS. Posterior Meniscal Root Repairs: Outcomes of an Anatomic Transtibial Pull-Out Technique. Am J Sports Med. 2017;45:884-91.
-
38Bernhardson AS, Aman ZS, Dornan GJ, Kemler BR, Storaci HW, Brady AW, et al. Tibial Slope and Its Effect on Force in Anterior Cruciate Ligament Grafts: Anterior Cruciate Ligament Force Increases Linearly as Posterior Tibial Slope Increases. Am J Sports Med. 2019 Feb;47(2):296-302.
-
39Dejour D, Saffarini M, Demey G, Baverel L. Tibial slope correction combined with second revision ACL produces good knee stability and prevents graft rupture. Knee Surg Sports Traumatol Arthrosc. 2015;23:2846-52.
-
40Hinckel BB, Demange MK, Gobbi RG, Pécora JR, Camanho GL. The Effect of Mechanical Varus on Anterior Cruciate Ligament and Lateral Collateral Ligament Stress: Finite Element Analyses. Orthopedics. 2016 Jul 1;39(4):e729-36.
-
41Chahla J, Dean CS, Moatshe G, Mitchell JJ, Cram TR, Yacuzzi C, LaPrade RF. Meniscal Ramp Lesions: Anatomy, Incidence, Diagnosis, and Treatment. Orthop J Sports Med. 2016 Jul 26;4(7):2325967116657815.
-
42Guess TM, Razu S. Loading of the medial meniscus in the ACL deficient knee: a multibody computational study. Med Eng Phys. 2017 Mar;41:26-34.
-
43Bonasia D, Dettoni F, Palazzolo A, Rossi R. Opening Wedge High Tibial Osteotomy and Anterior Cruciate Ligament Reconstruction or Revision. Arthrosc Tech. 2017;6:1735-41.
-
44Fujisawa Y, Masuhara K, Shiomi S. The effect of high tibial osteotomy on osteoarthritis of the knee. An arthroscopic study of 54 knee joints. Orthop Clin North Am. 1979;10:585-608.
-
45Wang Z, Zeng Y, She W, Luo X, Cai L. Is opening-wedge high tibial osteotomy superior to closing-wedge high tibial osteotomy in treatment of unicompartmental osteoarthritis? A meta-analysis of randomized controlled trials. Int J Surg. 2018 Dec;60:153-63.
-
46Noyes MF, Mayfield W, Barber-Westin S, Albright J, Heckmann T. Opening Wedge High Tibial Osteotomy: An Operative Technique and Rehabilitation Program to Decrease Complications and Promote Early Union and Function. Am J Sports Med. 2006;34:1263-73.
-
47Pérez-Mañanes R, Arnal-Burró J, Manaute J, Rodríguez F, Vaquero J. D Surgical Printing Cutting Guides for Open-Wedge High Tibial Osteotomy: Do It Yourself. J Knee Surg. 2016;29:690-5.
-
48Petruse R, Cofaru N, Cofaru I. Customizable Patient-Specific Cutting Guide for High Tibial Osteotomy. Acta Universitatis Cibiniensis. Technical Series. 2019;71:49-54.
-
49Hevesi M, Macalena JA, Wu IT, Camp CL, Levy BA, Arendt EA, et al. High tibial osteotomy with modern PEEK implants is safe and leads to lower hardware removal rates when compared to conventional metal fixation: a multi-center comparison study. Knee Surg Sports Traumatol Arthrosc. 2019;27:1280-90.
-
50Sonnery-Cottet B, Thaunat M, Freychet B, Pupim BHB, Murphy CG, Claes S. Outcome of a combined anterior cruciate ligament and anterolateral ligament reconstruction technique with a minimum 2-year follow-up. Am J Sports Med. 2015:43:1598-605.
-
51Webster KE, Kate E, Feller JA. Exploring the high reinjury rate in younger patients undergoing anterior cruciate ligament reconstruction. Am J Sports Med. 2016;44:2827-32.
-
52Getgood A, Brown C, Lording T, Amis A, Claes S, Geesling A, Musahi V. The anterolateral complex of the knee: results from the international ALC consensus group meeting. Knee Surg Sports Trauma Arthrosc. 2019;27:166-76.
-
53Kittl C, El-Daou H, Athwal K, Gupte C, Weiler A, William A, Amis A. The role of anterolateral structures and the ACL in controlling laxity of the intact and ACL-dificient knee. Am J Sports Med. 2016 Feb;44(2):345-54.
-
54Inderhaug E, Stephen J, Williams A, Amis A. Anterolateral tenodesis or anterolateral ligament complex reconstruction. Am J Sports Med. 2017 Nov;45(13):3089-97.
-
55Smith PA, Thomas DM, Pomajzl RJ, Bley JA, Pfeiffer FM, Cook JL. A Biomechanical Study of the Role of the Anterolateral Ligament and the Deep Iliotibial Band for Control of a Simulated Pivot Shift With Comparison of Minimally Invasive Extra-articular Anterolateral Tendon Graft Reconstruction Versus Modified Lemaire Reconstruction After Anterior Cruciate Ligament Reconstruction. Arthroscopy. 2019 May;35(5):1473-83.
-
56Hewison CE, Tran MN, Kaniki N, Remtulla A, Bryant D, Getgood AM. Lateral Extra-articular Tenodesis Reduces Rotational Laxity When Combined With Anterior Cruciate Ligament Reconstruction: A Systematic Review of the Literature. Arthroscopy. 2015 Oct;31(10):2022-34.
-
57Sonnery-Cottet B, Barbosa N, Tuteja S, Daggett M, Kajetanek C, Thaunat M. Minimally invasive anterolateral ligament reconstruction in the setting of anterior cruciate ligament injury. Arthrosc Tech. 2016;5:211-5.
-
58Delaloye JR, Murar J ,González M, Amaral T, Kakatkar V, Sonnery-Cottet B. Clinical outcomes after combined anterior cruciate ligament and anterolateral ligament reconstruction. Tech Orthop. 2018;33:225-31.
-
59Pernin J, Verdonk P, Aït Si Selmi T, Massin P, Neyret P. Long-Term Follow-up of 24.5 Years After Intra-Articular Anterior Cruciate Ligament Reconstruction With Lateral Extra-Articular Augmentation. Am J Sports Med. 2010;38:1094-102.
-
60Zaffagnini S, Marchegigiani Muccioli GM, Grassi A, Roberti di Sarsina T, Signorelli C, Urrizola F, et al. Over-the-top ACL Reconstruction Plus Extra-Articular Lateral Tenodesis With Hamstring Tendon Grafts. Prospective Evaluation With 20 Years Minimum Follow-up. Am J Sports Med. 2017;45:3233-42.
Descargar artículo:
Licencia:
Este contenido es de acceso abierto (Open-Access) y se ha distribuido bajo los términos de la licencia Creative Commons CC BY-NC-ND (Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional) que permite usar, distribuir y reproducir en cualquier medio siempre que se citen a los autores y no se utilice para fines comerciales ni para hacer obras derivadas.
Comparte este contenido
En esta edición
- <em>REACA</em>: school for authors
- Reconstruction of the medial patellofemoral ligament is effective in treating lateral patellofemoral instability, even in the presence of trochlear dysplasia. A review of 18 cases
- Results of the survey on the use of ultrasound among the members of the Spanish Association of Arthroscopy (Asociación Española de Artroscopia [AEA])
- Management of anterior glenohumeral instability without significant glenoid bone damage
- Rehabilitation following anterior capsulolabral arthroscopic Bankart repair: a guide for the young arthroscopist
- Diagnosis and management of injuries of the anterior cruciate ligament in skeletally immature patients. A narrative review
- Residual instability after reconstruction surgery of the anterior cruciate ligament. What are we missing?
- Posterolateral instability of the knee following osteochondral fracture including the femoral insertion of the popliteus tendon. A case report
- Meso-type long portion of the biceps: normal anatomical variant
- Instructions for authors (Apr. 2021)
Más en PUBMED
Más en Google Scholar
Más en ORCID


Revista Española de Artroscopia y Cirugía Articular está distribuida bajo una licencia de Creative Commons Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional.