Results of the survey on the use of ultrasound among the members of the Spanish Association of Arthroscopy (Asociación Española de Artroscopia [AEA])
Resultados de la encuesta sobre el uso del ecógrafo realizada a los socios de la Asociación Española de Artroscopia (AEA)
Resumen:
Objetivo: conocer la implementación y el uso de la ecografía musculoesquelética (Eco MSK) en las consultas del aparato locomotor por parte de los especialistas en cirugía ortopédica y artroscopia dentro del seno de la AEA. Asimismo, si se realizan terapias ecoguiadas (TEG) o cirugías ecoasistidas (CEA).
Método: se envió, a través de la secretaría técnica, una encuesta a todos los socios de la AEA que constaba de 23 preguntas con 2 o 3 posibles respuestas cada una. Se recibieron 82 encuestas, 70 respondidas por traumatólogos (85%) y 12 (15%) por médicos del deporte y otras especialidades (todos socios de la AEA).
Resultados: el 60% de los participantes de la encuesta ya estaban utilizando la Eco MSK en su práctica diaria, con formación en cursos y máster acreditados, aunque el 66% llevaba menos de 3 años usándola. A la hora de confirmar el diagnóstico, un 46% se apoya en otras pruebas de imagen. El 41% realiza “todas” las técnicas de infiltración de forma ecoguiada y el 85% de los encuestados no tiene experiencia en CEA, aunque el 80% considera que tiene un futuro interesante.
Conclusiones: existe un alto grado de satisfacción con el uso de la Eco MSK (86% de los participantes). La principal limitación de este estudio es el número de personas que respondieron a la encuesta (82) en relación con el total de los destinatarios de la misma (1.200).
Nivel de evidencia: IV.
Abstract:
Objective: to determine the implementation and use of musculoskeletal ultrasound (Eco MSK) in locomotor system clinics on the part of specialists in orthopedic surgery and arthroscopy in the setting of the Spanish Association of Arthroscopy (AEA). The performance of ultrasound-guided therapy (UGT) or ultrasound-assisted surgery (UAS) was also evaluated.
Method: the technical secretariat distributed a survey to all members of the AEA, consisting of 23 questions with 2 or 3 possible answers each. A total of 82 completed surveys were received: 70 answered by traumatologists (85%) and 12 by sports physicians and other specialists (15%) (all of them members of the AEA).
Results: sixty percent of the responders were already using Eco MSK in their daily practice, with training through accredited courses and master programs - though 66% had been using the technique for less than three years. For confirming the diagnosis, 46% relied on other imaging tests. Forty-one percent performed "all" infiltration techniques under ultrasound guidance, and 85% of those surveyed had no experience with UAS - though 80% considered it to have a promising future.
Conclusions: high satisfaction with the use of Eco MSK was observed (86% of the participants). The main limitation of the study is the small sample size: 82 responders out of 1200 professionals that received the survey.
Level of evidence: IV.
Introduction
As a diagnostic technique, ultrasound is efficient, inexpensive, easy to use and without adverse effects, and can prove useful in many osteomuscular conditions(1). Ultrasound in orthopedic surgery and traumatology is an adjunct to medical practice that adds information to the patient case history and physical examination, improves the understanding of the lesion on the part of the patient, increases confidence in the care received, and moreover allows certain treatments to be carried out in the same procedure(2). Based on the above, there appears to be a gradually increasing use of musculoskeletal ultrasound (Eco MSK) in locomotor system clinics in Spain.
In this regard, mention must be made of the work started years ago by other specialists such as rheumatologists, sports and occupational medicine physicians, general practitioners, rehabilitators, and even (within our own field) pediatric orthopedists. On the other hand, many courses, sessions and textbooks have served to encourage an increasingly large percentage of traumatologists to use this tool and know it in-depth, in what one of the authors in a Letter to the Editor has termed the "stethoscope of the traumatologist"(3). The percentage of colleagues within the Spanish Association of Arthroscopy (Asociación Española de Artroscopia [AEA]) that use the technique, and their degree of satisfaction with it, are not known, however (Figure 1).
The primary objective of this article was to directly determine the percentage of use of Eco MSK among the members of the AEA in both the clinic and in the operating room. The secondary objectives were to determine whether ultrasound-guided therapy (UGT) and/or ultrasound-assisted surgery (UAS) are used, and the degree of personal satisfaction with the outcomes obtained. Lastly, we sought to determine whether these techniques are contemplated by the medical insurance companies.
The authors belong to the Muscle and Tendon Injuries Study Group (Grupo de Estudio de Lesiones Musculares y Tendinosas [GELMUT]) within the AEA.
Material and methods
The survey was carried out in September 2019 in Google Forms format. It consisted of a heading with a brief presentation, and 23 questions (see Table 1) defined among the authors, each with two or three possible answers, and distributed into 5 sections (Introduction, Training, Care practice, Professional problems and Conclusions). The 23 questions were defined and agreed upon by the members of the GELMUT selected for the development and distribution of the survey with the aim of obtaining the maximum information on the use of Eco MSK for both diagnostic purposes and as an adjunct to ultrasound-guided treatments. The questions were mutually excluding.
The technical secretariat distributed the survey in October 2019 to all the members of the AEA via e-mail (with a reminder after 10 days), and was also made public on the social networks (Instagram, Twitter and Facebook). A three-month period was allowed for completion and return of the survey. The results obtained were studied and analysed.
Results
A total of 82 completed surveys were received (7% of the members of the AEA): 70 were answered by traumatologists (85%) and the rest by sports physicians (9%) and other specialists (6%) (all members of the AEA). The number of subjects that answered each question, and the answers obtained, are reported in Table 1.
Discussion
The use of Eco MSK was seen to be widespread among the participants in the survey (86%), generated high satisfaction in their clinical practice, and afforded more complete and efficient patient care. We consider these findings to be very positive, since the intervention times are markedly shortened, confidence is increased, more disease conditions are diagnosed, and in particular there is a lesser need for other complementary tests(9), with a decrease in healthcare costs and the affording of real-time patient treatment(10,11).
A survey such as that used in the present study is effective in evidencing the situation, since it offers an up-to-date "snapshot" of the practice of the technique among the members of the AEA. Although participation in this first survey has been low (only 7% of the members of the AEA), it was seen that 60% of the responders are already using Eco MSK in their daily practice. However, we are still far from full incorporation of the technique, as evidenced by similar surveys conducted in other countries(4). On the other hand, 80% of those who do not use the technique plan to do so over the short term. Such progression may be because ultrasound affords security not only in application to diagnosis but also in carrying out invasive techniques(5) and in the postoperative control of certain disease conditions(6). It is also known that ultrasound and the physicians that perform the technique in the clinic offer security and confidence for the patients(2). Considering the usefulness of ultrasound in the clinic, some professionals have referred to it as their "third hand"(7).
The use of Eco MSK is increasingly widespread due to its many advantages, including the fact that it is accessible, innocuous, non-invasive and painless, easily repeatable and allows the evaluation of organs and structures in motion and in real time(1). Likewise, it is relatively inexpensive (the cost of these systems having decreased drastically in recent years), particularly when compared to other techniques such as magnetic resonance imaging (MRI) or computed tomography (CT), and the systems used are small in size, without affecting image quality(8). It is encouraging that 80% of those who do not use the technique plan to do so over the short term, as evidenced by our survey.
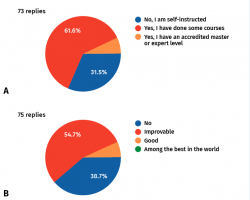
A total of 61.5% of the responders had already participated in training courses (Figure 2A), and 7% had even completed an accredited master. Nevertheless, 31.5% had received no such training and were "self-instructed" in the use of the technique. Thirty-nine percent of the responders considered that the level of Eco MSK practice among traumatologists in Spain is not good (Figure 2B). Only 16% claimed to read articles, books or monographs, see videos on ultrasound, or belong to study groups. In this regard, mention must be made of the EcoSemed group (of the Spanish Society of Sports Medicine [Sociedad Española de Medicina Deportiva]) and Gesmute (of the Spanish Society of Sports Traumatology [Sociedad Española de Traumatología Deportiva]). The AEA has created the GELMUT.
In the care setting, it can be concluded that Eco MSK has been in use for a short time: 66% of the responders had been using the technique for less than three years, while 35% had been using it for over three years.
A total of 61% of the responders applied Eco MSK in all joints, and only 39% exclusively used the technique as a means to perform UGT.
Forty-one percent routinely performed ultrasound-guided interventional procedures, and 37% claimed to be starting such practices. In turn, 76% of the professionals considered that these techniques are clearly more efficient and cause fewer side effects. We found that there are members of the AEA that do not use ultrasound on a daily basis, i.e., they have not included the technique in their diagnostic repertoire but have occasionally performed ultrasound-guided interventional procedures.
With regard to professional problems, only 8% of those surveyed reported ultrasound as being contemplated by medical insurance companies, i.e., the immense majority (92%) have no such coverage. This same percentage considered the creation of a unified consultation + Eco MSK fee (forfait) to be an interesting possibility. In private medical practice, we consider that the medical and insurance companies should contemplate this technique, which we refer to as a "dressed consultation", including the use of ultrasound by orthopedic surgeons and traumatologists that hold official accreditation of their training in ultrasound, as a unified consultation + Eco MSK fee - as occurs in other specialties such as Gynecology and Obstetrics, Urology or Vascular Surgery. The scientific societies, the Professional Union of Private Practice Physicians (Unión Profesional de Médicos de Ejercicio Libre [Unipromel]), and the official physician associations have important work to do in this regard.
One of the key considerations for developing this practice is the availability of an ultrasound system in our clinic (according to the results of the survey, only 28% of the responders currently have such equipment). The need to share the ultrasound system with other Departments (i.e., not having it close at hand), or the need to appoint the patient for a visit on some other day, limits the possibility of using the technique as needed, and slows the process and resolution of the disease condition.
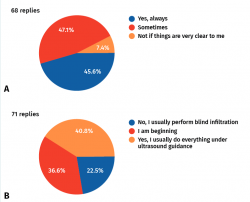
For confirming the diagnosis, 46% of the responders always relied on other imaging tests, 47% did so only occasionally, and 7% did not request other tests if the diagnosis could be established in conjunction with the physical examination (Figure 3).
Most of the professionals (85%) had no experience with UAS (such surgery currently being performed by only 15%) - though 80% considered it to have a promising future. According to the available data, UGT appears to be safe and effective(12,13,14). In general, ultrasound-assisted techniques are more precise than injections guided by anatomical reference points(15), and they moreover allow many disease conditions to be resolved without having to resort to the operating room(16).
However, the body of evidence is still limited, due to sample size and quality issues. Future research should focus on these treatments based on randomized, controlled prospective designs involving larger samples and possibly in comparison with other treatment modalities, with a view to further establishing their safety, efficacy, cost-effectiveness and role in the treatment of musculoskeletal diseases. On the other hand, an interesting research line in UAS is being conducted, with promising perspectives(17).
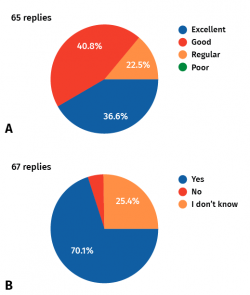
The participants in the survey reported high satisfaction (Figure 4) with Eco MSK (86% rated their experience as excellent or good), and 70% considered that their outcomes have improved as a result of introduction of the technique. A total of 77% of those surveyed expressed interest in joining the GELMUT of the AEA.
With regard to training in ultrasound, a range of face-to-face as well as onlinecourses are available. However, in order to ensure adequate training, it would be advisable to establish accredited levels with the awarding of the title of expert in the field. This would allow the adoption of uniform criteria, definition of the basic terminology, the issuing of reports and skilful management of Eco MSK, as occurs in other specialties. Traumatologists do not tend to have difficulties in this respect, since they have precise knowledge of the anatomy and experience (to one degree or other) with arthroscopic surgery, they afford triangulation and proprioception skills.
There are not many studies in the literature similar to our own, and only one has been targeted to traumatologists and another to rheumatologists. The first of these studies was published in 2017 by Wang et al.(4), who conducted a survey to assess the current use of Eco MSK for diagnostic purposes and for guided injections among surgeon members of the American Society for Surgery of the Hand (ASSH). The authors distributed a 22-question survey and used the chi-square test to evaluate differences in the use of ultrasound in relation to the characteristics of the participants. Of the latter, 304 (43%) reported having an ultrasound system in their clinic, while 362 (51%) used the technique for diagnostic purposes. A total of 8% of the responders used ultrasound to diagnose carpal tunnel syndrome, and 168 (23.5%) used it for guided injections. The study concluded that the use of ultrasound by surgeons of the upper extremity was divided between diagnostic applications, with fewer surgeons using the technique to diagnose carpal tunnel syndrome, and the performance of guided injections. The availability of the ultrasound system and its use for diagnostic purposes appeared to be influenced by the setting of the practice.
The second study was published in 2010 by Takase et al.(18), who conducted a survey among the members of the Japanese College of Rheumatology to describe the frequency with which they made use of Eco MSK. A total of 139 questionnaires were completed and analysed. Almost one third of the responders (32.4%) applied Eco MSK for patient treatment, and 87.8% considered it to be a useful tool. A lack of training was the main reason for not using Eco MSK.
Our survey is more complete than those commented above since it addresses different areas such as training, care practice and even professional problems - not only the utilization of Eco MSK as such.
The main limitation of the present study is the sample size: 82 responders out of 1200 professionals that received the survey (i.e., only 7% of the global members of the AEA). The authors intend to increase the participation percentage in following studies. Although it is true that 60% of the responders were already using Eco MSK in their clinical practice, this fact could have encouraged them to answer the survey - in contrast to those who were still not using the technique (measurement instrument bias).
Another limitation is the fact that the survey was only sent to members of the AEA, despite the fact that the technique is also useful in many other areas of traumatology and other specialties that deal with musculoskeletal disorders. It would be interesting to conduct a future survey with a greater number of orthopedic surgeons from all over the country, with implication of the regional and monographic societies, and even of the Spanish Society of Orthopedic Surgery and Traumatology (Sociedad Española de Cirugía Ortopédica y Traumatología [SECOT]).
Conclusions
Sixty percent of the responders were already using Eco MSK in their daily practice - though 66% had been using the technique for less than three years. Forty-one percent performed "all" infiltration techniques under ultrasound guidance (UGT). Eighty percent considered the technique, and even the concept of UAS, to have a promising future. Eight-six percent of the responders expressed high satisfaction with Eco MSK. The main limitation of the study is the small number of responders (n= 82; only 7% of the members of the AEA). It would be interesting to conduct a similar survey involving a greater participation of traumatologists, with a view to comparing the results and analysing tendencies.
Figuras
Figure 2. A: Do you have any accredited specific training?; B: Do you consider the level of musculoskeletal ultrasound practice among traumatologists in Spain to be good?
Figure 3. A: When indicating surgery, do you request any other imaging technique?; B: Do you have experience in ultrasound-guided treatments?
Figure 4. A: Degree of satisfaction with musculoskeletal ultrasound; B: Do you feel your outcomes to have improved since you started to use ultrasound?
Tablas
Información del artículo
Cita bibliográfica
Autores
Pedro Bernáldez Domínguez
Servicio de Traumatología y Ortopedia. Hospital Básico de Riotinto. Riotinto. Huelva
SportMe Medical Center. Sevilla
Hospital Infanta Elena. Huelva
Santos Moros Marco
Servicio de Traumatología. Hospital MAZ. Zaragoza
Cirugía Ortopédica y Traumatología. Unidad de Miembro Superior. Hospital MAZ Zaragoza. Arthrosport Zaragoza
Editor asociado de REACA
Servicio de Traumatología y Cirugía Ortopédica. Hospital de la Mutua MAZ. Zaragoza
Ethical responsibilities
Conflicts of interest. The authors state that they have no conflicts of interest.
Financial support. This study has received no financial support.
Protection of people and animals. The authors declare that this research has not involved studies in humans or in animals.
Data confidentiality. The authors declare that the protocols of their centre referred to the publication of patient information have been followed.
Right to privacy and informed consent. The authors declare that no patient data appear in this article.
Referencias bibliográficas
-
1Apard T. Ultrasonography for the orthopaedic surgeon. Orthop Traumatol Surg Res. 2019 Feb;105(1S):S7-S14.
-
2Kostopoulos D, Rawat M. Musculoskeletal ultrasound in orthopedic practice. J Bodyw Mov Ther. 2019 Oct;23(4):815-7.
-
3Bernáldez Domínguez, P. Alcántara Martos T. El ecógrafo: el fonendo del traumatólogo: utilidad diagnóstica y terapéutica. Rev S And Traum Ort. 2017;34(4/4):17-26.
-
4Wang WL, Kruse K, Fowler JR. A Survey of the Use of Ultrasound by Upper Extremity Surgeons. Hand (NY). 2017;12(1):31-8.
-
5Rutten MJ, Collins JM, Maresch BJ, Smeets JH, Janssen CM, Kiemeney LA, et al. Glenohumeral joint injection: a comparative study of ultrasoundand fluoroscopically guided techniques before MR arthrography. Eur Radiol. 2009;19:722-30.
-
6Plomb-Holmes C, Clavert P, Kolo F, Tay E, Lädermann A; French Arthroscopic Society. An orthopaedic surgeon's guide to ultrasound imaging of the healthy, pathological and postoperative shoulder. Orthop Traumatol Surg Res. 2018 Dec;104(8S):S219-S232.
-
7Bernáldez Domínguez, P. La tercera mano (carta al director). Rev S And Traum Ort. 2019;36(2/4):56-5.
-
8Soubeyrand M, Begin M, Pierrart J, Gagey O, Dumontier C, Guerini H. Ultrasonography for hand surgeons (lecture from the 46th meeting of French Society of Hand Surgery). Chir Main. 2011;30:368-84.
-
9Nazarian LN. The top 10 reasons musculoskeletal sonography is an important complementary or alternative technique to MRI. AJR Am J Roentgenol. 2008 Jun;190(6):1621-6.
-
10Parker L, Nazarian LN, Carrino JA, Morrison WB, Grimaldi G, Frangos AJ, et al. Musculoskeletal imaging: medicare use, costs, and potential for cost substitution. J Am Coll Radiol. 2008;5:182-8.
-
11Chiu CH, Chen P, Chen AC, Hsu KY, Chang SS, Chan YS, et al. Shoulder ultrasonography performed by orthopedic surgeons increases efficiency in diagnosis of rotator cuff tears. J Orthop Surg Res. 2017;12:63.
-
12Finnoff JT. The Evolution of Diagnostic and Interventional Ultrasound in Sports Medicine. PM R. 2016 Mar;8(3 Suppl):S133-8.
-
13Daley EL, Bajaj S, Bisson LJ, Cole BJ. Improving injection accuracy of the elbow, knee, and shoulder: does injection site and imaging make a difference? A systematic review. Am J Sports Med. 2011;39:656-2.
-
14Jiménez Díaz F. Ecografía musculoesquelética: nivel experto. Marbán; 2017.
-
15Lee RKL, Griffith JF. Top-Ten Tips for Ultrasound-Guided Joint Injection. Semin Musculoskelet Radiol. 2019 Aug;23(4):419-28.
-
16Fernandez-Jaén T, Sanz-Zapata F, Cortés JM, Balius-Mata R, Álvarez-Rey G, Garrido-González JI, et al. Proposal for a Clinical Analysis of Patellar Tendon Pathologies: In Search of Efficient Therapeutic Indications. Orthop J Sports Med. 2020 Aug 31;8(8):2325967120946312.
-
17Moroni S, Gibello AF, Zwierzina M, Nieves GC, Montes R, Sañudo J, et al. Ultrasound-guided decompression surgery of the distal tarsal tunnel: a novel technique for the distal tarsal tunnel syndrome-part III. Surg Radiol Anat. 2019 Mar;41(3):313-21.
-
18Takase K, Ohno S, Ideguchi H, Takeno M, Shirai A, Ishigatsubo Y. Use of musculoskeletal ultrasound in Japan: a survey of practicing rheumatologists. Mod Rheumatol. 2010 Aug;20(4):376-80.
Descargar artículo:
Licencia:
Este contenido es de acceso abierto (Open-Access) y se ha distribuido bajo los términos de la licencia Creative Commons CC BY-NC-ND (Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional) que permite usar, distribuir y reproducir en cualquier medio siempre que se citen a los autores y no se utilice para fines comerciales ni para hacer obras derivadas.
Comparte este contenido
En esta edición
- <em>REACA</em>: school for authors
- Reconstruction of the medial patellofemoral ligament is effective in treating lateral patellofemoral instability, even in the presence of trochlear dysplasia. A review of 18 cases
- Results of the survey on the use of ultrasound among the members of the Spanish Association of Arthroscopy (Asociación Española de Artroscopia [AEA])
- Management of anterior glenohumeral instability without significant glenoid bone damage
- Rehabilitation following anterior capsulolabral arthroscopic Bankart repair: a guide for the young arthroscopist
- Diagnosis and management of injuries of the anterior cruciate ligament in skeletally immature patients. A narrative review
- Residual instability after reconstruction surgery of the anterior cruciate ligament. What are we missing?
- Posterolateral instability of the knee following osteochondral fracture including the femoral insertion of the popliteus tendon. A case report
- Meso-type long portion of the biceps: normal anatomical variant
- Instructions for authors (Apr. 2021)
Más en PUBMED
Más en Google Scholar
Más en ORCID


Revista Española de Artroscopia y Cirugía Articular está distribuida bajo una licencia de Creative Commons Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional.