Reconstruction of the medial patellofemoral ligament is effective in treating lateral patellofemoral instability, even in the presence of trochlear dysplasia. A review of 18 cases
La reconstrucción del ligamento patelofemoral medial es eficaz en el tratamiento de la inestabilidad patelofemoral lateral, incluso en presencia de displasia troclear. Una revisión de 18 casos
Resumen:
Objetivos: discutir la necesidad de realizar trocleoplastia en presencia de displasia troclear (DT) en casos de inestabilidad patelofemoral (IPF) revisando los resultados quirúrgicos y funcionales en nuestra serie de pacientes.
Materiales y métodos: se realizó un estudio retrospectivo de una serie de 18 pacientes intervenidos mediante reconstrucción del ligamento patelofemoral medial (LPFM) con aloinjerto tendinoso fijado mediante 2 anclajes en rótula y túnel transóseo femoral. Se asoció osteotomía de anteromedialización del aparato extensor en 8 pacientes. Las variables estudiadas fueron la presencia de DT (según la clasificación de Dejour), la distancia entre la tuberosidad tibial anterior y el surco troclear (TA-GT), el resultado funcional posquirúrgico según la escala Kujala y los casos de recidiva de la disociación patelofemoral. Los resultados funcionales postoperatorios y las recidivas se analizaron en función del grado de DT asociado.
Resultados: la edad media fue de 24,5 ± 7,6 años en el momento de la cirugía, con un 66% de pacientes mujeres. El tiempo medio de seguimiento postoperatorio fue de 6,5 años (rango: 1 a 12 años). Se encontró algún grado de DT en un 77,8% de los pacientes: 4 casos de tróclea de tipo A de Dejour, 3 casos de tipo B, 2 casos de tipo C y 5 casos de tipo D. En los casos con un TA-GT aumentado (33,3%) se asoció una osteotomía tibial de anteromedialización. Hubo 1 caso de recidiva de inestabilidad en el postoperatorio. No hubo diferencias en los resultados funcionales postoperatorios entre los grupos con presencia o ausencia de DT (p > 0,05). Tampoco en el caso de las recidivas.
Conclusiones: la reconstrucción del LPFM es una técnica segura y eficaz para el manejo de la IPF. La presencia de DT no parece condicionar un peor resultado funcional o mayor tasa de recidivas.
Nivel de evidencia: 4.
Relevancia clínica: la IPF es una entidad frecuente en nuestra práctica diaria y la presencia de DT ha asociado clásicamente técnicas como la trocleoplastia a su manejo. Este estudio refleja la experiencia positiva del no uso de esta técnica en presencia de DT y pretende aportar evidencia a favor de la abstención terapéutica en presencia de esta alteración anatómica.
Abstract:
Objectives: To assess the need for trochleoplasty in the presence of trochlear dysplasia (TD) in cases of patellofemoral instability (PFI), and review the surgical and functional outcomes in our series of patients.
Material and methods: A retrospective study was made of 18 patients subjected to reconstruction of the medial patellofemoral ligament (MPFL) with a tendon allograft affixed by two anchorings in the patella and transosseous femoral tunnel. Anteromedialisation osteotomy of the extensor apparatus was added in 8 patients. The study parameters were the presence of TD (according to the Dejour classification), the distance between the anterior tibial tuberosity and the trochlear groove (TT-TG), the postoperative functional outcome according to the Kajula scale, and the cases of patellofemoral dissociation relapse. The postoperative functional outcomes and relapses were analysed according to the grade of associated TD.
Results: The mean patient age was 24.5 ± 7.6 years at the time of surgery, and 66% of the patients were women. The mean postoperative follow-up was 6.5 years (range: 1-12 years). Some grade of TD was recorded in 77.8% of the patients: four cases of Dejour type A trochlea, three cases of type B, two cases of type C and 5 cases of type D. An anteromedialisation tibial osteotomy was added in the cases with increased AT-TG (33.3%). One instability relapse was recorded in the postoperative period. There were no differences in the postoperative functional outcomes between the groups with or without TD (p > 0.05). There likewise were no differences in the case of the relapses.
Conclusions: Reconstruction of the MPFL is a safe and effective technique for the management of PFI. The presence of TD does not appear to imply a poorer functional outcome or a higher relapse rate.
Level of evidence: 4.
Clinical relevance: Patellofemoral instability is a common condition in our daily practice, and the presence of TD classically has added techniques such as trochleoplasty to its management. This study reflects the positive experience of not using this technique in the presence of TD, and seeks to contribute evidence in favour of therapeutic abstention in the case of this anatomical alteration.
Introduction
Patellofemoral instability (PFI) is caused by anatomical and mechanical factors, affecting congruence between the joint surfaces of the patella and the femoral trochlear groove secondary to a triggering traumatic event (via a direct or indirect mechanism). It is characterized by instability following a first dislocation episode, with a probability of repeat luxation of up to 50%(1).
The main mechanism restricting lateral displacement of the patella in the first 30° of flexion is the medial patellofemoral ligament (MPFL), which is responsible for up to 60% of containment of the joint(2). This ligament is located in the thickness of the deep layers of the medial patellofemoral (PF) complex of the knee, and extends from the groove between the medial femoral epicondyle and tubercle of the adductor magnus to the upper two-thirds of the medial margin of the patella(3). According to Nomura, some degree of damage to this ligament is found in 96% of all patients with some patellar luxation episode, since its elongation capacity is only 20-30%(4). Many studies now warrant the efficacy and safety of reconstruction of the MPFL as a technique for correcting PFI(5).
Trochlear dysplasia (TD) has been defined as one of the main factors predisposing to PFI(6). Initially described by Henri Dejour and subsequently modified by his son, David Dejour (1998), the Dejour classification divides this alteration into four types: type A, with a trochlear angle of over 145° (trochlear flattening); type B, with a flat trochlea and the appearance of a proximal supratrochlear crest; type C, flattening with hypoplasia of the medial condyle; and type D; trochlear flattening with hypoplasia of the medial condyle and supratrochlear crest(7). Trochleoplasty comprises a series of techniques for remodelling the proximal trochlear surface, and is indicated in patients with high grade TD - the main objective being to improve the morphology of the groove and eliminate the supratrochlear prominence(8). These techniques, which are usually combined with other surgical procedures, offer satisfactory outcomes, with improvement of the functional assessment scores and of the recurrent luxation rate. However, they are also characterized by a difficult learning curve and significant complications that have been described in different published series: increased anterior knee pain (11%), joint stiffness (2-46%), recurrent luxation (0.6-10.5%), repeat surgery (14-25%) and an unknown incidence (due to the lack of long-term studies) of degenerative chondral damage(8).
The present study discusses the indication of trochleoplasty in patients with PFI and high-grade TD. In this regard, a clinical review was made of our patients with PFI subjected to MPFL reconstruction surgery.
Material and methods
A descriptive case series analysis was made. The inclusion criteria were patients with PFI, defined by at least two episodes of complete patellofemoral dislocation, subjected to MPFL reconstruction surgery and with a postoperative follow-up period of at least one year. A total of 18 patients meeting these criteria were consecutively recruited covering the period between June 2006 and June 2017.
All patients underwent a preoperative study consisting of a physical examination with patellar displacement manoeuvres (flipping, trapping, patellar tracking), posteroanterior and lateral radiographs and computed tomography (CT) assessing the presence and magnitude of PFI, TD(9,10,11) and the distance between the tibial tuberosity and the trochlear groove (TT-TG)(12).
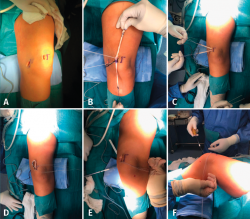
The patients were treated using a reconstruction technique with tissue bank plasty (semitendinosus, rectus internus or long flexor of the big toe) according to the procedure of Romero(13) (Figure 1). In those patients with a pathological TT-TG distance, a previous anteromedialisation osteotomy of the tibial tuberosity was carried out, affixed with two screws. In no case was anything done to the trochlea.
reaca.28272.fs2007042en-figure1.png
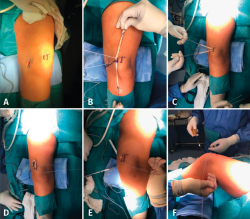
Figure 1. Surgical technique: following standard evaluation arthroscopic surgery, two longitudinal incisions measuring about 3 cm are made over the superomedial margin of the patella and over the medial epicondyle of the femur (A). Both beds are prepared: for the patella, the subperiosteal bone of this region is exposed and two radiolucent biocompatible anchorings measuring 2.3 mm, each preloaded with a thread, are placed (Bioraptor®, Smith & Nephew), spaced 1 cm apart. For the femoral bed, the Schöttle insertion point is identified and the femoral tunnel is drilled with a diameter of 6-7 mm, depending on the width of the plasty. The identification of this point was made based on radiographic references(29). The plasty is affixed to the patella, knotting its middle portion with the two sutures of the anchorings (B and C), and the ends of the plasty are passed over a plane superficial to the joint capsule of the knee, between both skin incisions (D). The free ends of the plasty are joined and inserted within the femoral tunnel, affixing them with a reabsorbable interference screw 1 mm larger than the drilled size of the femur (E). Fixation is made at 30° of flexion (F).
In the postoperative period the patients followed a standardized protocol of support according to tolerance, with orthosis in extension during the first three weeks, together with a protocol for controlled gain of joint range: first two weeks up to 30° of flexion, third and fourth week up to 60°, fifth and sixth week up to 90°, and allowing progression according to tolerance from the sixth week.
Postoperative assessment was made using the multiple choice questionnaire on satisfaction and the Kujala scale(14). We also collected data on the immediate and late complications following surgery, as well as on the appearance of new dislocations. The data were collected on a retrospective basis from the hospital case histories and telephone interviews.
The data were analysed comparing the functional outcomes and the recurrent luxation rate according to the type of TD involved. The patients were grouped according to the grade of TD measured from the plain radiographs and preoperative CT scan.
In view of the few individuals involved in the study, normal distribution of the quantitative variables was not assumed, and nonparametric statistical tests were used. The chi-squared test was used to compare qualitative variables, while the Kruskal-Wallis test was used for comparison of quantitative variables. The SPSS version 22.0 statistical package (IBM Corp., Armonk, NY, USA) was used throughout.
Results
All patients underwent complete follow-up without losses over time until discharge, and were adequately contacted for the telephone interview. The mean follow-up period was 6.5 years (range 1-12 years). The mean patient age at the time of surgery was 24.5 ± 7.6 years (range: 14-36). Most of the patients (66%) were women.
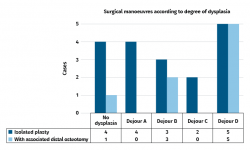
Some degree of TD was recorded in 14 of the 18 patients. Anteromedialization osteotomy of the extensor apparatus was added in 8 patients (45%) - the criterion being a TT-TG distance of over 20 mm in the preoperative CT study. Five of these patients corresponded to the group of individuals with high grade TD (statistically significantly association; p = 0.025) (Figure 2).
Final patient satisfaction with the outcomes was good or very good in 91% of the cases, as assessed by the simple multiple choice questionnaire. The postoperative Kujala score evidenced correct functional evolution over time: median 94 (interquartile range [IQR] 88.5-100). No comparison versus the preoperative values was made, as these were not available.
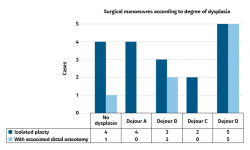
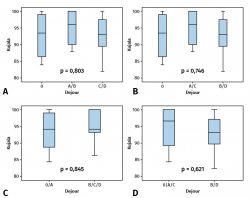
On examining the functional outcomes according to the grade of TD, no significant differences were observed in terms of the Kujala score (Figure 3) (p > 0.05 in all cases).
reaca.28272.fs2007042en-figure3.png
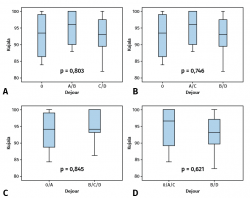
Figure 3. Statistical plots: comparative analysis of the functional outcomes measured by the Kujala score according to the degree of dysplasia (TD): absence of TD versus types A and B, and versus types C and D (A); absence of TD versus types A and C, and versus types B and D (B); absence of TD and type A versus types B, C and D (C); absence of TD and types A and C versus types B and D (D).
We identified two cases of recurrent patellofemoral luxation. The first corresponded to a 14-year-old male with failure of the technique and early atraumatic relapse. The patient presented open physes at the time of surgery, with a TT-TG distance of 18 mm. The postoperative CT scan showed the femoral fixation point to be very proximal to the anatomical point to save the physis. The patient underwent second surgery with allograft reconstruction of the MPFL, correcting the femoral insertion and adding osteotomy of the anterior tibial tuberosity (ATT)(performed because this represented relapse with a TT-TG distance at the upper limit of normal), followed by sustained symptoms improvement with no further episodes. This patient presented a type B trochlea. The second patient, with TD corresponding to type D, was detected during the telephone interview, since he had not consulted the centre again. Five years after the operation, the patient suffered another traumatic dislocation while practicing sports, with sporadic episodes thereafter. The patient rejected returning to the clinic, since he claimed to be leading a normal life, with few problems due to the instability episodes. No new surgery was therefore contemplated. This case was considered to represent genuine relapse, while the first case was regarded as an error of the technique.
During the postoperative period, two patients experienced discomfort with the fixation material: one reported discomfort with the ATT screws and the other experienced discomfort due to staple reinforcement of plasty fixation. Both patients remained asymptomatic after extraction surgery. There were no other postoperative complications.
Discussion
Many studies currently warrant the surgical management of chronic PFI. Our study showed satisfactory outcomes with the treatment of PFI in patients presenting different grades of TD, combining techniques such as reconstruction of the MPFL and osteotomy of the tibial tuberosity, when indicated.
Many current consensuses and algorithms postulate "customized" management, where depending on the identified predisposing structural component, surgery seeks to correct the causal element or elements(15,16). Trochleoplasty surgery comprises the manoeuvres needed to secure a more anatomical trochlear groove, in a more lateral position, and alleviate the supratrochlear eminence that could displace the patella outside its path in the first degrees of patellar flexion, as evidenced by biomechanical studies(17). Such surgery has demonstrated satisfactory outcomes in terms of the control of PFI. However, the same authors that defend this kind of surgery also admit an important incidence of complications in centres with good experience and case volumes, and agree that the procedure is technically demanding(18,19). In addition, the patella, which tends to develop flat (mirroring the dysplastic trochlea) effectively improves its anatomical position(9), but it has not been shown that improved joint congruence is achieved with an iatrogenically more anatomical trochlea. A number of issues remain to be solved, such as viability of the cartilage over the long term after surgery, as well as complications such as joint stiffness (2-46%), persistent or increased postoperative pain (11-100%), or the need for repeat surgery(20,21). On the other hand, an increasing number of studies confirm the efficacy and safety of MPFL reconstruction surgery(22,23), evidencing that the technique is safe and reproducible and represents a first choice option for dealing with this disease condition, with a low associated comorbidity rate.
Many studies warrant the use of both techniques; however, the existing literature is of moderate quality, and few authors have compared the outcomes of the two procedures. In 2006, Schöttle(24) compared the recurrent luxation rate between two populations in which only MPFL reconstruction surgery was performed. The luxation rate in the first group (no dysplasia or type A dysplasia) was 0%, versus 8.3% in the group of patients with high grade dysplasia (type B, C and D), In 2014, Hopper(25) found the recurrent luxation rate in knees with high grade dysplasia (Dejour type C and D - 11% of the study population) to reach 100% (7 out of 7 patients after isolated MPFL reconstruction) versus 9.6% in the group with mild dysplasia (Dejour type A and B). Some of these patients required rescue trochleoplasty surgery, with good outcomes. Such surgery was therefore recommended from the start in cases of high grade dysplasia. One of the largest studies reporting outcomes of MPFL reconstruction was published by Enderlein(22) (240 patients), with a TD rate of 70% in the studied population. The mentioned study did not report the recurrent luxation rate according to grades of dysplasia after reconstruction of the MPFL, though an inversely proportional relationship was observed between the grade of dysplasia and the Kujala score, with a general recurrent luxation rate of 4.5% in the study population with a high TD rate. In 2016, the German group of Balcarek(26) published a meta-analysis comparing the results of reconstruction of the MPFL alone versus trochleoplasty added to realignment of the extensor apparatus, in the presence of low grade TD (Dejour type A) and high grade TD (Dejour type B, C and D). The authors recorded similar functional improvement, with a difference in recurrent luxation rate of 2% and 7%, respectively, in both groups. The study concluded that trochleoplasty is the best option for avoiding recurrent luxation. However, the study design excluded studies of surgical reconstruction of the MPFL together with distal realignment of the extensor apparatus - in contrast to our own study, where this combination was indeed used - though it did analyse trochleoplasty associated to other techniques. Recent anatomical studies(6) have reported that the anatomical factors that predispose to PFI show a certain tendency to group together; it is therefore overly simplistic to compare the outcomes of trochleoplasty associated to other surgical procedures versus isolated MPFL reconstruction - a circumstance that appears to constitute a limitation of conclusions of the mentioned meta-analysis.
In this study distal realignment osteotomy has been associated to many of the cases of TD (with a statistically significant relationship). It could be pondered whether this association is responsible for the good outcomes obtained. However, the previously mentioned anatomical relationship(6), and the fact of surgical indication based on individual anatomical factors, reinforce our opinion that the outcomes are valid.
In our series a number of statistical analyses were made, comparing different groupings of TD, since the literature is not clear in defining what types of TD are considered to be high grade. Some studies describe the latter as corresponding to types B and D(16,20,27), due to the presence of the supratrochlear crest, while others define high grade TD as corresponding to types C and D(25), or types B, C and D(23,24,26). In our attempt to address these different positionings and to compare what those authors who defend trochleoplasty regard as surgical and non-surgical types of TD, we divided the dysplastic patients into different comparator groups - no differences being found in terms of functional outcome or the recurrence of luxation in any of the analyses made.
On interpreting the relapses, the case of failure of the technique in the patient with immature physes was not taken to represent a genuine relapse, in view of the clear associated human technical error - though the number of patients requiring repeat surgery did increase. The case of manifest relapse was indeed taken to represent relapse - with an appearance rate of 5.5% in our series that is similar to the data found in the literature(22,26).
With regard to the choice of type of graft for reconstruction plasty, a recent review has evidenced no superiority of any of the currently available materials(28), i.e., autograft, allograft and synthetic components, with respect to the rest. Due to the increase in surgery time, the concomitant morbidity on removing the autograft and the availability of allografts in our centre, we chose the latter type of plasty in our series, with no associated complications (plasty rupture, deinsertion, infection, etc.).
Our functional and surgical outcomes in reconstruction of the MPFL associated to distal realignment of the extensor apparatus (where indicated), even in the presence of high grade TD, are good and comparable to those of the patients with mild dysplasia or no dysplasia. Therefore it may be considered that the presence of PFI in high grade dysplasia can be initially treated with surgical techniques such as MPFL reconstruction and realignment of the extensor apparatus. Based on these data, we believe that the recommendation of "customized" surgery and trochleoplasty as the technique of first choice in patients with PFI and high grade TD could be relegated to a second line of intervention for postsurgical relapses - this in fact now becoming a widespread tendency.
With regard to the limitations of the present study, mention must be made of the design and limited sample size, which do not allow the drawing of firm conclusions. In effect, the number of cases was small, and this - together with the retrospective study design - implied that the conclusions lacked statistical power and were influenced by possible biases associated to these conditions. Due to the lack of preoperative values for comparison purposes, the validity of the postoperative functional outcomes must be viewed with caution. Furthermore, techniques (trochleoplasty) that have not been performed or analysed in the study have been discussed. In view of all the above, it therefore would be advisable to carry out comparative studies with a broader statistical base in order to draw definitive conclusions.
Conclusions
Reconstruction of the MPFL, in combination with distal realignment of the extensor apparatus, in individuals with a TT-TG distance of over 20 mm is a safe and effective technique for the management of lateral PFI. The presence of TD does not appear to imply a poorer functional outcome or a higher relapse rate.
Figuras
Figure 1. Surgical technique: following standard evaluation arthroscopic surgery, two longitudinal incisions measuring about 3 cm are made over the superomedial margin of the patella and over the medial epicondyle of the femur (A). Both beds are prepared: for the patella, the subperiosteal bone of this region is exposed and two radiolucent biocompatible anchorings measuring 2.3 mm, each preloaded with a thread, are placed (Bioraptor®, Smith & Nephew), spaced 1 cm apart. For the femoral bed, the Schöttle insertion point is identified and the femoral tunnel is drilled with a diameter of 6-7 mm, depending on the width of the plasty. The identification of this point was made based on radiographic references(29). The plasty is affixed to the patella, knotting its middle portion with the two sutures of the anchorings (B and C), and the ends of the plasty are passed over a plane superficial to the joint capsule of the knee, between both skin incisions (D). The free ends of the plasty are joined and inserted within the femoral tunnel, affixing them with a reabsorbable interference screw 1 mm larger than the drilled size of the femur (E). Fixation is made at 30° of flexion (F).
Figure 3. Statistical plots: comparative analysis of the functional outcomes measured by the Kujala score according to the degree of dysplasia (TD): absence of TD versus types A and B, and versus types C and D (A); absence of TD versus types A and C, and versus types B and D (B); absence of TD and type A versus types B, C and D (C); absence of TD and types A and C versus types B and D (D).
Información del artículo
Cita bibliográfica
Autores
Cristina Dauder Gallego
Hospital Universitario Fundación Alcorcón. Madrid
Homero Valencia García
Departamento de Cirugía Ortopédica y Traumatología. Hospital Universitario Fundación Alcorcón. Madrid
Lucía Villarrubia Arias
Hospital Universitario Fundación Alcorcón. Madrid
Carlos Gavín González
Unidad de Cirugía Ortopédica y Traumatología. Fundación Hospital Alcorcón. Alcorcón. Madrid
Hospital Quirón. Madrid
Ethical responsibilities
Conflicts of interest. The authors state that they have no conflicts of interest.
Financial support. This study has received no financial support.
Protection of people and animals. The authors declare that this research has not involved studies in humans or in animals.
Data confidentiality. The authors declare that the protocols of their centre referred to the publication of patient information have been followed.
Right to privacy and informed consent. The authors declare that no patient data appear in this article.
Referencias bibliográficas
-
1Fithian DC, Paxton EW, Stone ML, Silva P, Davis DK, Elias DA, White LM. Epidemiology and natural history of acute patellar dislocation. Am J Sports Med. 2004;32(5):1114-21.
-
2Conlan T, Garth WP Jr, Lemons JE. Evaluation of the medial soft-tissue restraints of the extensor mechanism of the knee. J Bone Joint Surg Am. 1993;75(5):682-93.
-
3Amis AA, Firer P, Mountney J, Senavongse W, Thomas NP. Anatomy and biomechanics of the medial patellofemoral ligament [published correction appears in Knee. 2004 Feb;11(1):73]. Knee. 2003;10(3):215-20.
-
4Nomura E. Classification of lesions of the medial patello-femoral ligament in patellar dislocation. Int Orthop. 1999;23(5):260-3.
-
5Dejour D, Le Coultre B. Osteotomies in patello-femoral instabilities. Sports Med Arthrosc Rev. 2007;15(1):39-46.
-
6Fitzpatrick CK, Steensen RN, Tumuluri A, Trinh T, Bentley J, Rullkoetter PJ. Computational analysis of factors contributing to patellar dislocation. J Orthop Res. 2016;34(3):444-53.
-
7Dejour H, Walch G, Nove-Josserand L, Guier C. Factors of patellar instability: an anatomic radiographic study. Knee Surg Sports Traumatol Arthrosc. 1994;2(1):19-26.
-
8Batailler C, Neyret P. Trochlear dysplasia: imaging and treatment options. EFORT Open Rev. 2018;3(5):240-7.
-
9Fucentese SF, Schöttle PB, Pfirrmann CW, Romero J. CT changes after trochleoplasty for symptomatic trochlear dysplasia. Knee Surg Sports Traumatol Arthrosc. 2007;15(2):168-74.
-
10Martínez S, Korobkin M, Fondren FB, Hedlund LW, Goldner JL. Computed tomography of the normal patellofemoral joint. Invest Radiol. 1983;18(3):249-53.
-
11Biedert RM, Bachmann M. Anterior-posterior trochlear measurements of normal and dysplastic trochlea by axial magnetic resonance imaging. Knee Surg Sports Traumatol Arthrosc. 2009;17(10):1225-30.
-
12Colvin AC, West RV. Patellar instability. J Bone Joint Surg Am. 2008;90(12):2751-62.
-
13Schottle PB, Romero J, Schmeling A, Weiler A. Technical note: anatomical reconstruction of the medial patellofemoral ligament using a free gracilis autograft. Arch Orthop Trauma Surg. 2008;128(5):479-84.
-
14Gómez-Valero S, García-Pérez F, Flórez-García MT, Miangolarra-Page JC. Revisión sistemática de los cuestionarios autocumplimentados adaptados al español para la valoración funcional de pacientes con afecciones de rodilla. Rev Esp Cir Ortop Traumatol. 2017;61(2):96-103.
-
15Weber AE, Nathani A, Dines JS, Allen AA, Shubin-Stein BE, Arendt EA, Bedi A. An Algorithmic Approach to the Management of Recurrent Lateral Patellar Dislocation. J Bone Joint Surg Am. 2016 Mar 2;98(5):417-27. Erratum in: J Bone Joint Surg Am. 2016 Jun 15;98(12):e54.
-
16Laidlaw MS, Diduch DR. Current Concepts in the Management of Patellar Instability. Indian J Orthop. 2017;51(5):493-504.
-
17Amis AA, Oguz C, Bull AM, Senavongse W, Dejour D. The effect of trochleoplasty on patellar stability and kinematics: a biomechanical study in vitro. J Bone Joint Surg Br. 2008;90(7):864-9.
-
18Donell ST, Joseph G, Hing CB, Marshall TJ. Modified Dejour trochleoplasty for severe dysplasia: operative technique and early clinical results. Knee. 2006;13(4):266-73.
-
19Verdonk R, Jansegers E, Stuyts B. Trochleoplasty in dysplastic knee trochlea. Knee Surg Sports Traumatol Arthrosc. 2005;13(7):529-33.
-
20Beaufils P, Thaunat M, Pujol N, Scheffler S, Rossi R, Carmont M. Trochleoplasty in major trochlear dysplasia: current concepts. Sports Med Arthrosc Rehabil Ther Technol. 2012;4:7.
-
21Von Knoch F, Böhm T, Bürgi ML, von Knoch M, Bereiter H. Trochleaplasty for recurrent patellar dislocation in association with trochlear dysplasia. A 4- to 14-year follow-up study. J Bone Joint Surg Br. 2006 Oct;88(10):1331-5.
-
22Enderlein D, Nielsen T, Christiansen SE, Faunø P, Lind M. Clinical outcome after reconstruction of the medial patellofemoral ligament in patients with recurrent patella instability. Knee Surg Sports Traumatol Arthrosc. 2014;22(10):2458-64.
-
23Kyung HS, Kim HJ. Medial Patellofemoral Ligament Reconstruction: A Comprehensive Review. Knee Surg Relat Res. 2015;27(3):133-40.
-
24Schöttle PB, Scheffler SU, Schwarck A, Weiler A. Arthroscopic medial retinacular repair after patellar dislocation with and without underlying trochlear dysplasia: a preliminary report. Arthroscopy. 2006;22(11):1192-8.
-
25Hopper GP, Leach WJ, Rooney BP, Walker CR, Blyth MJ. Does degree of trochlear dysplasia and position of femoral tunnel influence outcome after medial patellofemoral ligament reconstruction?. Am J Sports Med. 2014;42(3):716-22.
-
26Balcarek P, Rehn S, Howells NR, Eldridge JD, Kita K, Dejour D, et al. Results of medial patellofemoral ligament reconstruction compared with trochleoplasty plus individual extensor apparatus balancing in patellar instability caused by severe trochlear dysplasia: a systematic review and meta-analysis. Knee Surg Sports Traumatol Arthrosc. 2017;25(12):3869-77.
-
27Ntagiopoulos PG, Byn P, Dejour D. Midterm results of comprehensive surgical reconstruction including sulcus-deepening trochleoplasty in recurrent patellar dislocations with high-grade trochlear dysplasia. Am J Sports Med. 2013;41(5):998-1004.
-
28McNeilan RJ, Everhart JS, Mescher PK, Abouljoud M, Magnussen RA, Flanigan DC. Graft Choice in Isolated Medial Patellofemoral Ligament Reconstruction: A Systematic Review With Meta-analysis of Rates of Recurrent Instability and Patient-Reported Outcomes for Autograft, Allograft, and Synthetic Options. Arthroscopy. 2018;34(4):1340-54.
-
29Sanchís-Alfonso V. Guidelines for medial patellofemoral ligament reconstruction in chronic lateral patellar instability. J Am Acad Orthop Surg. 2014 Mar;22(3):175-82.
Descargar artículo:
Licencia:
Este contenido es de acceso abierto (Open-Access) y se ha distribuido bajo los términos de la licencia Creative Commons CC BY-NC-ND (Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional) que permite usar, distribuir y reproducir en cualquier medio siempre que se citen a los autores y no se utilice para fines comerciales ni para hacer obras derivadas.
Comparte este contenido
En esta edición
- <em>REACA</em>: school for authors
- Reconstruction of the medial patellofemoral ligament is effective in treating lateral patellofemoral instability, even in the presence of trochlear dysplasia. A review of 18 cases
- Results of the survey on the use of ultrasound among the members of the Spanish Association of Arthroscopy (Asociación Española de Artroscopia [AEA])
- Management of anterior glenohumeral instability without significant glenoid bone damage
- Rehabilitation following anterior capsulolabral arthroscopic Bankart repair: a guide for the young arthroscopist
- Diagnosis and management of injuries of the anterior cruciate ligament in skeletally immature patients. A narrative review
- Residual instability after reconstruction surgery of the anterior cruciate ligament. What are we missing?
- Posterolateral instability of the knee following osteochondral fracture including the femoral insertion of the popliteus tendon. A case report
- Meso-type long portion of the biceps: normal anatomical variant
- Instructions for authors (Apr. 2021)
Más en Google Scholar
Más en ORCID


Revista Española de Artroscopia y Cirugía Articular está distribuida bajo una licencia de Creative Commons Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional.