Arthroscopic acetabular microfractures of the hip: survival and clinical outcome of the technique with a minimum follow-up of 5 years
Microfracturas acetabulares artroscópicas de cadera: supervivencia y resultado clínico de la técnica con seguimiento mínimo de 5 años
Resumen:
Objetivo: determinar la supervivencia y el resultado clínico de la microfractura artroscópica en una cohorte de pacientes con lesión condral de espesor completo a nivel acetabular en el choque femoroacetabular (CFA) con seguimiento mínimo de 5 años.
Métodos: estudio multicéntrico retrospectivo de una base de datos prospectiva de pacientes con CFA y lesión condral acetabular de espesor completo tratada mediante microfracturas con seguimiento mínimo de 5 años. Se registraron variables epidemiológicas, tiempo de evolución de la sintomatología, hallazgos y técnicas artroscópicas, valoración clínica mediante el cuestionario Hip Outcome Score-Activities of Daily Living (HOS-AVD), valoración radiológica, complicaciones, reintervenciones y supervivencia de la técnica.
Resultados: se incluyeron en el estudio 88 caderas. El seguimiento medio fue de 86,8 meses (desviación estándar –DE–: 30). La puntuación media se incrementó de manera estadísticamente significativa en el cuestionario HOS-AVD de 64,8 (DE: 20,4) a 86,9 puntos (DE: 12,6). Precisaron reintervención quirúrgica 8 pacientes (9%). La supervivencia de la técnica quirúrgica a los 62 meses de seguimiento fue del 91,6%.
Conclusiones: a 5 años de seguimiento mínimo, la microfractura como tratamiento de la lesión condral de espesor completo en el paciente intervenido mediante cirugía artroscópica de cadera (CAC) por CFA permite obtener incrementos significativos en el cuestionario HOS-AVD, con una supervivencia de la técnica quirúrgica del 91,6% a 62 meses. La mejoría clínica se consigue en el primer año postoperatorio y se mantienen hasta el quinto año tras la cirugía.
Nivel de evidencia: nivel III.
Relevancia clínica: es importante conocer los resultados de supervivencia y clínicos de la técnica quirúrgica más utilizada en el tratamiento de la lesión condral de espesor completo a un seguimiento mayor de 5 años. Actualmente, son escasos los estudios con seguimiento a medio y largo plazo.
Abstract:
Objective: To determine the survival and clinical outcomes of arthroscopic microfractures in a cohort of patients with full-thickness chondral injury at acetabular level in femoroacetabular impingement (FAI) with a minimum follow-up of 5 years.
Methods: A retrospective multicentre study was made of a prospective database of patients with FAI and full-thickness acetabular chondral injury treated by microfracture with a minimum follow-up of 5 years. Epidemiological variables, symptoms evolution time, arthroscopic findings and techniques, clinical assessment using the Hip Outcome Score-Activities of Daily Living (HOS-AVD) questionnaire, radiological assessment, complications, reinterventions and survival of the technique were recorded.
Results: A total of 88 hips were included in the study. The mean duration of follow-up was 86.8 months (standard deviation [SD]: 30). The mean HOS-AVD score increased significantly from 64.8 (SD: 20.4) to 86.9 points (SD: 12.6). Eight patients (9%) required repeat surgery. Survival of the surgical technique at 62 months follow-up was 91.6%.
Conclusions: After a minimum 5-year follow-up period, microfracture as a treatment for full-thickness chondral injury in patients undergoing arthroscopic hip surgery (AHS) due to FAI results in significant increases in the HOS-AVD score, with a survival of the surgical technique of 91.6% at 62 months. Clinical improvement is achieved in the first postoperative year and is maintained until the fifth year after surgery.
Level of evidence: level III.
Clinical relevance: it is important to know the survival and clinical outcomes of the most commonly used surgical technique for treating full-thickness chondral injury after a follow-up period of over 5 years. At present, studies involving medium and long-term follow-up are scarce.
Introduction
Chondral injury is a limiting factor in joint preservation surgery. Femoroacetabular impingement (FAI) is one of the most common causes of chondral injury of the hip(1). Arthroscopic hip surgery (AHS) has made it possible to detect these chondral lesions, with an incidence of up to 70.3% described in one study(2). Repair procedures and regeneration techniques have been described for the treatment of chondral injuries. Repair procedures require a viable chondrocyte. However, at the time of diagnosis, the chondral lesion may be a full-thickness injury, and in this case regeneration techniques are indicated(3).
Microfracture is a chondral regeneration technique indicated for focal full-thickness lesions with a stable or repairable labrum and a size of less than 400 mm2 (4,5). The technique involves drilling holes in the subchondral bone to allow bone marrow, progenitor cells and growth factors to fill the chondral defect and regenerate the tissue(6). This technique can be performed directly at the time of diagnosis, using AHS, with no associated morbidity, since no donor site is needed, and the procedure is moreover inexpensive. A drawback compared to other regeneration techniques is that the regenerated tissue does not have the same properties as native cartilage, and there are doubts about its durability(7). Previous studies have shown satisfactory results with this technique, albeit with short-term follow-up periods(1,8,9).
The present study was carried out to determine the clinical outcome and survival of the arthroscopic microfracture technique in a cohort of patients with full-thickness chondral injury in FAI, with a minimum follow-up of 5 years. Our working hypothesis was that the microfracture chondral regeneration technique would result in a significant increase in the clinical assessment scores, with a minimum medium-term survival of 90%.
Methods
Patient selection
A retrospective, multicentre study was made of a prospective AHS database between January 2012 and December 2017. The inclusion criteria were a patient age between 18-55 years, a diagnosis of FAI, Tönnis stage 0-1, joint height > 2 mm, full-thickness acetabular cartilage lesion treated by microfracture, and a minimum follow-up of 5 years. Patients with hip dysplasia determined by a centre-edge angle of less than25°, Legg-Calvé-Perthes disease, previous hip surgery, avascular necrosis, and an age of under 18 or over 55 years were excluded. The diagnosis of FAI was based on the anamnesis, examination and complementary tests.
All patients gave informed consent to inclusion in the study, which was approved by the Clinical Research Ethics Committee (CREC) of Hospital Universitario de Elche (Spain), with Registration Code PI 05/2022.
Surgical technique
Arthroscopic hip surgery was performed with the patient in the supine position using anterolateral, mid-anterior and distal anterolateral arthroscopic portals. Cam-type and pincer-type morphologies were treated by acetabular and femoral osteoplasty under arthroscopic and radiological control. The labral injury was repaired or debrided while preserving as much of the labrum as possible(10), capable of maintaining the clot of cells from the subchondral bone.
The chondral lesion was assessed according to the Outerbridgeclassification(11). Once the full-thickness chondral lesion was identified, its size (width and length) was determined. The unstable delaminated cartilage and calcified layer were then resected. The perforations were made with a 30° and45°punch, perpendicular to the subchondral bone, from the periphery to the centre of the lesion, and spaced 3-4 mm apart. On completion, the intraarticular fluid inflow was cut off to confirm the outflow of fat and blood droplets from the subchondral bone through the punctures made (Figure 1). The area of the cartilage lesion was calculated using the formula: height × width, and was classified as less than 200 mm2, between 200-350 mm2, or over 350 mm2 (12).
reacae.31181.fs2312031en-figure1.png
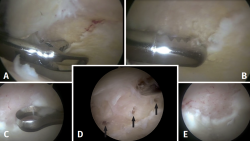
Figure 1. Intraoperative view of a right hip from the anterolateral portal with70°optics. Insertion of instruments from the mid-anterior portal. A: resection of the unstable delaminated cartilage with forceps; B: resection of the unstable delaminated cartilage with motor; C: resection of the calcified layer with curette; D: microfractures (black arrows); E: cutting of joint fluid inflow to confirm the outflow of fat and blood droplets from the subchondral bone.
Primary variable
The Hip Outcome Score-Activities of Daily Living (HOS-ADL) questionnaire(13), translated into Spanish and validated(14), was used for clinical assessment. These assessments were made preoperatively, at 6 months, at one year, and annually thereafter. Clinical significance was determined from the minimum clinically important difference (MCID), patient acceptable symptom state (PASS) and substantial clinical benefit (SCB) scores for HOS-ADL at 5-year follow-up. The threshold values for clinical significance were 10.2 points for MCID, 92.2 points for PASS and 94.6 points for SCB(15).
Secondary variables
Epidemiological variables, symptoms evolution time, arthroscopic findings and techniques, and radiological assessment were recorded.
An anteroposterior radiological study of the pelvis in the standing position and axial Dunn view was requested in all patients. The presence of cam and/or pincer type lesions, the height of the joint interline in the loading zone, alpha angle, Wiberg angle of acetabular coverage, Tönnis angle, and degree of joint degeneration according to the Tönnis scale(16) were determined.
In order to detect the presence of avascular necrosis, or labral or articular cartilage damage, magnetic resonance imaging (MRI) was requested preoperatively in all patients.
Postoperative management
Passive mobility was started at 24 hours, with restriction of hip rotations for four weeks. No mobility-restricting orthoses were used. Assisted partial weight bearing with two crutches was allowed for four weeks.
Survival of the technique
Survival of the technique was determined by the need for revision AHS or conversion to total hip replacement (THR).
Statistical analysis
The statistical analyses were made using the SPSS version 20.0 statistical package (SPSS Inc., Chicago, IL, USA). Normal data distribution was assessed with the Kolmogorov-Smirnov test. The Student t-test or Mann-Whitney U-test and analysis of variance (ANOVA) were used for the comparison of continuous variables. In the case of categorical variables, use was made of the chi-square test for variables with a normal distribution, or the Mantel-Haenszel test for nonparametric data. Statistical significance was considered for p ≤ 0.05. Survival of the technique with the need for reoperation as endpoint was determined with the Kaplan-Meier test.
Results
General findings
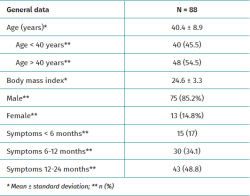
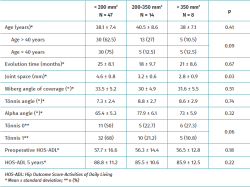
Eighty-eight hips were included in the study. The epidemiological variables and symptoms evolution time are shown in Table 1.
Radiologically, cam lesions were the most frequent type of FAI, being recorded in 35 hips (39.7%), followed by mixed types in 33 hips (37.5%) and pincer lesions in 20 hips (22.8%).
Intraoperative findings
Labral tears were identified in 79 hips (89.8%). Of these, 77 (97.4%) underwent labral repair and two (2.6%) were subjected to debridement.
All hips had full-thickness chondral lesions. The full-thickness chondral lesions were measured in 69 hips (78.4%). Their mean size was 19.3 mm in length (standard deviation [SD]: 9.5; range: 9-40 mm) and 10.0 mm in width (SD: 5.7; range: 8-30 mm). All the lesions were located at chondrolabral junction level. The mean area of the full-thickness chondral lesions was 209.2 mm2 (SD: 167; range: 50-750 mm2); 68.3% (47 hips) were < 200 mm2, 20.2% (14 hips) were between 200-350 mm2, and 11.5% (8 hips) were > 350 mm2. One patient (1.1%) had a chondral lesion of the femoral head.
Clinical findings
The mean duration of follow-up was 86.8 months (SD: 30; range: 60-142 months).
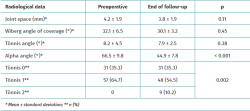
The radiological variables recorded preoperatively and at the end of follow-up are shown in Table 2. The mean degree of correction of the alpha angle was 21.6° (SD: 10.4°), the decrease being statistically significant. Nine patients (10.2%) progressed from Tönnis stage 1 to 2 at the end of follow-up.
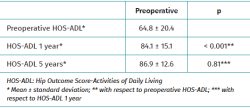
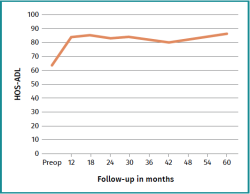
The mean score of the HOS-ADL questionnaire increased significantly at the end of follow-up. The most significant improvement was recorded in the first postoperative year, with no significant difference between the scores at the first and fifth year of follow-up (Table 3 and Figure 2). After 5 years of follow-up, 86.1% of the patients achieved MCID, 71.7% PASS and 61.3% SCB.
Complications, reinterventions and survival
There were no complications related to the microfracture technique or the hip arthroscopy technique.
At 5 years minimum follow-up, 8 patients (9%) required surgical reintervention: four (4.5%) underwent revision AHS and four (4.5%) were converted to THR. Revision AHS was performed at 8, 12, 14 and 15 months of follow-up, and conversion to THR at 28 months (patient with acetabular chondral lesion > 350 mm2 and chondral lesion of the femoral head), 59 months, 62 months (patient with acetabular chondral lesion > 350 mm2) and 113 months of follow-up. The survival rate of the surgical technique after 62 months of follow-up was 91.6% (95% CI: 85.6-97.6) (Figure 3).
Analysis according to the extent of the chondral lesion
The analysis of patients with the measurement of chondral lesion size revealed a significantly lower preoperative joint height in patients with lesions > 350 mm2 (Table 4). Of the 9 patients who progressed from Tönnis stage 1 to 2, a total of 5 had a chondral lesion > 350 mm2. In turn, the four patients who required revision AHS and two patients who required conversion to THR at 59 and 62 months of follow-up had a chondral lesion > 350 mm2. None of the patients with a chondral lesion < 350 mm2 experienced worsening of their degree of joint degeneration or required reoperation.
Discussion
According to our results, microfracture AHS as a treatment for full-thickness chondral lesions yields satisfactory results and a survival rate of 91.6% after a minimum of 5 years of follow-up.
In a systematic review of 11 studies including 267 patients on the indications and outcomes of microfracture in the treatment of FAI-associated chondral injury, MacDonald reported satisfactory clinical results over a mean follow-up of 29 months(17). Comparative studies have also been published between patients with chondral injuries subjected to microfracture treatment and patients without chondral injuries, with no significant differences being found in the clinical outcomes after a minimum follow-up of two(18,19) and three years(20). Recently, Akhtar published a systematic review on the results of hip chondral injury treatment, in which microfracture was seen to be the most commonly used technique. Of the 27 studies included in the review, 17 (with a total of 597 hips) analysed the outcome of microfractures, though only one study involved a follow-up period of more than 5 years. The review concluded that microfractures lead to significant increases in the score of the clinical assessment questionnaires used(9,21). In our series, the mean HOS-ADL score increased significantly at the end of follow-up; clinical improvement was achieved in the first year post-surgery, and was maintained 5 years after surgery.
Regarding the clinical significance of HOS-ADL, Luo(22) reported that 89.8% of 57 patients with one year of follow-up achieved MCID, while Kucharik(23) found that 25% achieved MCID, 56% PASS and 56% SCB, in 31 patients with one year of follow-up. In our 5-year minimum follow-up series involving the HOS-ADL, 86.1% of the patients achieved MCID, 71.7% PASS and 61.3% SCB.
The protocols for postoperative management after microfracture treatment lack consensus regarding no weight bearing or allowing partial weight bearing with crutches, or as regards the indicated time. Several studies recommend partial weight bearing with crutches between 4 and 16 weeks(1,16).
In his systematic review, Akhtar reported that only 13 studies analysed the size of the chondral lesion, with a mean size between 40-360 mm2. Of these 13 studies, 5 reported no correlation between chondral lesion size and the clinical outcomes(9). However, Kester, in his series of 33 patients, reported that poor clinical outcomes of microfracture are associated with chondral lesions larger than 390 mm2 after four years of follow-up(24). In turn, Loppini reported a negative correlation between chondral lesion size and clinical outcome over two years of follow-up, in his series of 62 patients(16). In our series, with a mean lesion size of 209 mm2, we found no significant differences in the HOS-ADL scores according to the size of the chondral lesion after 5 years of follow-up. However, we did record a greater progression of degenerative disease and need for reintervention in patients with chondral lesions > 350 mm2.
Complications associated with microfracture treatment are reported in 0-7.5% of the cases(9). In our series there were no complications associated with the surgical technique.
According to the systematic review published in 2023, the rates corresponding to revision AHS and conversion to THR after microfracture ranged from 0-18.2% and 0-34.6%, with a technique survival rate of 59.1-100% at 6-53 months of follow-up(9). The results of our series were similar, with revision AHS and conversion to THR in 4.5% of the cases, and a 91.6% survival rate at 62 months. However, Akhtar reported an increase in reintervention rate and a decrease in survival of the technique compared to the systematic review published by O'Connor in 2018(8,9). In turn, Domb published the outcomes of 22 hips with a minimum follow-up of 10 years, with a microfracture technique survival rate of 77%(25). In a study published in 2015, Fontana reported that the presence of a cam-type lesion, cartilage defect sizes > 400 mm2 an association with cartilage lesions of the femoral head, and a preoperative Modified Harris Hip Score (mHHS) of < 50 points were risk factors for conversion to THR(26).
Our study has limitations. Since patients with microfractures have also had other added surgical procedures, it is difficult to know the isolated effect of microfracture treatment upon the final clinical outcome. The data were collected prospectively, but this is a retrospective study. Furthermore, the study lacks a control group. On the other hand, the size of the chondral lesion was not recorded in all patients. Longer follow-up is needed to confirm the stability of the results obtained.
As strengths, this is a multicentre study, with an acceptable sample size and a medium-term follow-up.
Conclusions
After a minimum 5-year follow-up period, microfracture as a treatment for full-thickness chondral injury in patients undergoing AHS due to FAI results in significant increases in the HOS-ADL score, with a survival of the surgical technique of 91.6% at 62 months. Clinical improvement is achieved in the first postoperative year and is maintained until the fifth year after surgery.
Figuras
Figure 1. Intraoperative view of a right hip from the anterolateral portal with70°optics. Insertion of instruments from the mid-anterior portal. A: resection of the unstable delaminated cartilage with forceps; B: resection of the unstable delaminated cartilage with motor; C: resection of the calcified layer with curette; D: microfractures (black arrows); E: cutting of joint fluid inflow to confirm the outflow of fat and blood droplets from the subchondral bone.
Figure 2. Clinical evolution during the minimum 5 years of follow-up according to the Hip Outcome Score-Activities of Daily Living (HOS-ADL).
Tablas
Información del artículo
Cita bibliográfica
Autores
Javier Sanz Reig
Traumatología Vistahermosa. HLA Clínica Vistahermosa. Alicant
Grupo Ibérico de Preservación de Cadera (GIPCA)
Servicio de Cirugía Ortopédica y Traumatología. Clínica Vistahermosa. Alicante
Jesús Más Martínez
Traumatología Vistahermosa. HLA Clínica Vistahermosa. Alicante, España
Grupo Ibérico de Preservación de Cadera (GIPCA)
Alberto López Reyes
Hospital Viamed Santa Ángela de la Cruz. Sevilla
Grupo Ibérico de Preservación de Cadera (GIPCA)
Ana Castel Oñate
Unidad de Cadera. Hospital Universitario Príncipe de Asturias. Alcalá de Henares, Madrid
Grupo Ibérico de Preservación de Cadera (GIPCA)
Cirugía Ortopédica y Traumatología (COT). Hospital Universitario Príncipe de Asturias. Madrid
Joan Cabello Gallardo
Imove Traumatología. Barcelona
Hospital Germans Trias i Pujol. Badalona
Grupo Ibérico de Preservación de Cadera (GIPCA)
Marc Tey Pons
Unidad de Cadera. iMove Traumatología. Hospital Mi Tres Torres. Barcelona
I-Move Traumatologia. Barcelona
Grupo Ibérico de Preservación de Cadera (GIPCA)
Hospital Universitari Parc Taulí. Sabadell
Universidad Pompeu Fabra
Unidad de Cadera. Servicio de Cirugía Ortopédica y Traumatología. Hospital del Mar. Barcelona
Unidad de Artroscopia y Rodilla. ICATME-Institut Universitari Dexeus. Universitat Autònoma de Barcelona
Ethical responsibilities
Conflicts of interest. The authors state that they have no conflicts of interest.
Financial support. This study has received no financial support.
Protection of people and animals. The authors declare that this research has not involved human or animal experimentation.
Data confidentiality. The authors declare that the protocols of their work centre referred to the publication of patient information have been followed.
Right to privacy and informed consent. The authors declare that no patient data appear in this article.
Referencias bibliográficas
-
1Nakano N, Gohal C, Duong A, Ayeni OR, Khanduja V. Outcomes of cartilage repair techniques for chondral injury in the hip-a systematic review. Int Orthop. 2018;42:2309-22.
-
2Más Martínez J, Sanz-Reig J, Verdú Román CM, Bustamante Suárez de Puga D, Morales Santías M, Martínez Giménez E. Tönnis stage 0 and 1 acetabular rim cartilage injuries: incidence, grade, location and associated pre-surgical factors. Rev Esp Cir Ortop Traumatol. 2017;61:154-61.
-
3Bagheri K, Sierra F, Jamali AA. Acetabular Cartilage Repair: State of the Art in Surgical Treatment. J Hip Preserv Surg. 2020;7:205-24.
-
4Maldonado DR, Chen JW, Lall AC, et al. Microfracture in Hip Arthroscopy. Keep It Simple! Arthrosc Tech. 2019;8:e1063-e1067.
-
5Mella C, Núñez A, Villalón I. Treatment of acetabular chondral lesions with microfracture technique. SICOT J. 2017;3,45.
-
6Green CJ, Beck A, Wood D, Zheng MH. The biology and clinical evidence of microfracture in hip preservation surgery. J Hip Preserv Surg. 2016;3(2):108-23.
-
7Frisbie DD, Oxford JT, Southwood L, et al. Early events in cartilage repair after subchondral bone microfracture. Clin Orthop Relat Res. 2003;(407):215-27.
-
8O’Connor M, Minkara AA, Westermann RW, Rosneck J, Lynch TS. Outcomes of Joint Preservation Procedures for Cartilage Injuries in the Hip: A Systematic Review and Meta-analysis. Orthop J Sports Med. 2018;6:2325967118776944.
-
9Akhtar M, Wen J, Razick D, et al. Outcomes of Arthroscopic Joint Preservation Techniques for Chondral Lesions of the Hip: An Updated Systematic Review. Arthroscopy. 2023;29:S0749-8063(23)00948-9.
-
10Freehill MT, Safran MR. The labrum of the hip: diagnosis and rationale for surgical correction. Clin Sports Med. 2011;30:293-315.
-
11Bhatia S, Nowak DD, Briggs KK, Patterson DC, Philippon MJ. Outerbridge grade IV cartilage lesions in the hip identified at arthroscopy. Arthroscopy. 2016;32:814-9.
-
12Loppini M, La Camera F, Gambaro FM, Ruggeri R, Grappiolo G, Della Rocca F. Sport Activity and Clinical Outcomes after Hip Arthroscopy with Acetabular Microfractures at a Minimum 2-Year Follow-Up: A Matched-Pair Controlled Study. Life (Basel). 2022;12(8):1107.
-
13Martin RL, Philippon MJ. Evidence of Validity for the Hip Outcome Score in Hip Arthroscopy. Arthroscopy. 2007;23:822-6.
-
14Seijas R, Sallent A, Ruiz-Ibán MA, et al. Validation of the Spanish version of the Hip Outcome Score: a multicenter study. Health Qual Life Outcomes. 2014;12:70.
-
15Nwachukwu BU, Beck EC, Kunze KN, Chahla J, Rasio J, Nho SJ. Defining the Clinically Meaningful Outcomes for Arthroscopic Treatment of Femoroacetabular Impingement Syndrome at Minimum 5-Year Follow-up. Am J Sports Med. 2020;48:901-7.
-
16Mascarenhas VV, Castro MO, Rego PA, et al. The Lisbon Agreement on Femoroacetabular Impingement Imaging-part 1: overview. Eur Radiol. 2020;30:5281-97.
-
17MacDonald AE, Bedi A, Horner NS, et al. Indications and Outcomes for Microfracture as an Adjunct to Hip Arthroscopy for Treatment of Chondral Defects in Patients With Femoroacetabular Impingement: A Systematic Review. Arthroscopy. 2016;32:190-200.
-
18Domb BG, Gupta A, Dunne KF, Gui C, Chandrasekaran S, Lodhia P. Microfracture in the Hip: Results of a Matched-Cohort Controlled Study With 2-Year Follow-up. Am J Sports Med. 2015;43:1865-74.
-
19Lodhia P, Gui C, Chandrasekaran S, Suárez-Ahedo C, Vemula SP, Domb BG. Microfracture in the hip: a matched-control study with average 3-year follow-up. J Hip Preserv Surg. 2015;2:417-27.
-
20Más Martínez J, Sanz-Reig J, Verdú Román CM, Bustamante Suárez de Puga D, Morales Santías M, Martínez Giménez E. Arthroscopic hip surgery with a microfracture procedure of acetabular full-thickness chondral damage. Cohort study with a 3-year follow-up. Rev Esp Cir Ortop Traumatol. 2018;62:248-56.
-
21Domb BG, Lee MS, Annin S, et al. Patients Who Underwent Primary Hip Arthroscopy for Femoroacetabular Impingement with Acetabular Microfracture Show 77% Survivorship at 10-Year Follow-Up. Arthroscopy. 2023;39:1185-94.
-
22Luo TD, Beck EC, Trammell AP, et al. Hip Arthroscopic Microfracture Augmented With Platelet-Rich Plasma-Infused Micronized Cartilage Allograft Significantly Improves Functional Outcomes. Arthroscopy. 2022;38:2819-26.
-
23Kucharik MP, Abraham PF, Nazal MR, et al. Treatment of Full-Thickness Acetabular Chondral Flaps During Hip Arthroscopy: Bone Marrow Aspirate Concentrate Versus Microfracture. Orthop J Sports Med. 2021;9:23259671211059170.
-
24Kester BS, Begly JP, Capogna B, Chenard K, Youm T. Four-Year Outcomes Following Arthroscopic Microfracture of the Hip in Patients with Advanced Chondral Lesions. Bull Hosp Jt Dis (2013). 2020;78:123-30.
-
25Domb BG, Lee MS, Annin S, et al. Patients Who Underwent Primary Hip Arthroscopy for Femoroacetabular Impingement with Acetabular Microfracture Show 77% Survivorship at 10-Year Follow-Up. Arthroscopy. 2023;39:1185-94.
-
26Fontana A, de Girolamo L. Sustained five-year benefit of autologous matrix-induced chondrogenesis for femoral acetabular impingement-induced chondral lesions compared with microfracture treatment. Bone Joint J. 2015;97:628-35.
Descargar artículo:
Licencia:
Este contenido es de acceso abierto (Open-Access) y se ha distribuido bajo los términos de la licencia Creative Commons CC BY-NC-ND (Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional) que permite usar, distribuir y reproducir en cualquier medio siempre que se citen a los autores y no se utilice para fines comerciales ni para hacer obras derivadas.
Comparte este contenido
En esta edición
- We are living a golden age in Spanish arthroscopic surgery
- Alteration of the coronal and sagittal axes of the knee and its implication in the failure of anterior cruciate ligament reconstruction. A systematic review
- Arthroscopic acetabular microfractures of the hip: survival and clinical outcome of the technique with a minimum follow-up of 5 years
- Hip arthroscopy provides medical personnel with an early and complete return to work. A multicentre study
- Novel articles on combined ligamentous injury of the anterior cruciate ligament and medial ligament complex of the knee
- Anteroinferior shoulder instability. Essential articles
- Treatment of shoulder instability with bone defects using a combination of arthroscopic bone block and <em>remplissage</em> techniques
- Reconstruction of the rotator cuff using a triple-row arthroscopic technique. Surgical technique
- Endoscopic treatment of calcific tendinitis of the gluteus maximus. A case report
- Incomplete discoid medial meniscus presenting coalescence with the anterior cruciate ligament
Más en PUBMED
Más en Google Scholar
Más en ORCID


Revista Española de Artroscopia y Cirugía Articular está distribuida bajo una licencia de Creative Commons Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional.