Hip arthroscopy provides medical personnel with an early and complete return to work. A multicentre study
La artroscopia de cadera proporciona en el personal médico una reincorporación laboral temprana y completa. Estudio multicéntrico
Resumen:
Objetivos: describir los resultados funcionales y datos laborales en un grupo de pacientes médicos intervenidos de cirugía artroscópica de cadera (CAC) para el tratamiento del choque femoroacetabular (CFA) por cirujanos de alto volumen.
Material y método: se llevó a cabo una revisión retrospectiva con carácter multicéntrico de las CAC llevadas a cabo en personal médico como tratamiento del CFA por cirujanos de alto volumen. Se recogieron datos demográficos, parámetros funcionales, necesidad de CAC de revisión o conversión a prótesis total de cadera (PTC), nivel y tiempo de reincorporación a la actividad laboral y grado de satisfacción con el resultado de la cirugía.
Resultados: se intervinieron 40 caderas en 40 pacientes, 22 mujeres (55%) y 18 hombres (45%). El tiempo medio de seguimiento fue de 7,1 ± 3,8 años (1-12). Al final del seguimiento se obtuvo una mejoría estadísticamente significativa en las escalas Hip Outcome Score-Activities of Daily Living (HOS-ADL) e International Hip Outcome Tool 12 (i-HOT12) (de 60,1 ± 14,2 y 40,4 ± 16,2 preoperatorio a 86,8 ± 8,9 y 77 ± 11,6 postoperatorio, respectivamente; p < 0,001). Requirieron reintervención 5 pacientes (12,5%) durante el seguimiento, 2 CAC de revisión (5%), 1 caso de tenotomía de aductores (2,5%) y 2 conversiones a PTC (5%) por mala evolución a los 32 y 104 meses desde la CAC inicial. Todos los pacientes se reincorporaron a su puesto de trabajo tras la intervención con un tiempo medio de baja de 3,8 ± 1,8 meses (1-8). El grado de satisfacción con el resultado de la cirugía fue alto o muy alto en el 90% de los pacientes (muy alto 55%, alto 35%, medio 7,5% y bajo 2,5%).
Conclusiones: la CAC como tratamiento del CFA en el personal médico proporciona una mejoría de los parámetros funcionales y permite una reincorporación laboral temprana y al mismo nivel de actividad que antes de la lesión con una baja tasa de reintervenciones y conversión a PTC tras un seguimiento medio superior a 7 años.
Nivel de evidencia: estudio nivel IV, serie de casos retrospectiva.
Relevancia clínica: el presente estudio es el primero que describe los datos demográficos, laborales, resultados funcionales y necesidad de CAC de revisión o conversión a PTC en personal médico sometido a CAC por CFA.
Abstract:
Objectives: To describe the functional outcomes and occupational data in a group of medical personnel undergoing arthroscopic hip surgery (AHS) for the treatment of femoroacetabular impingement (FAI) by high-volume surgeons.
Methods: A multicentre retrospective review was made of AHS performed in medical personnel as treatment of FAI by high-volume surgeons. Demographic data, functional parameters, need for revision AHS or conversion to total hip replacement (THR), the level and time of return to work, and the degree of satisfaction with the outcome of surgery were recorded.
Results: A total of 40 hips were operated upon in 40 patients: 22 women (55%) and 18 men (45%). The mean duration of follow-up was 7.1 ± 3.8 years (range 1-12). At the end of follow-up, statistically significant improvement was recorded in the Hip Outcome Score-Activities of Daily Living (HOS-ADL) and International Hip Outcome Tool 12 (i-HOT12) scales (from 60.1 ± 14.2 and 40.4 ± 16.2 preoperatively to 86.8 ± 8.9 and 77 ± 11.6 postoperatively, respectively; p < 0.001). Five patients (12.5%) required reoperation during follow-up: 2 revision AHS (5%), 1 case of adductor tenotomy (2.5%), and 2 conversions to THR (5%), due to poor outcomes at 32 and 104 months after initial AHS. All patients returned to work after surgery, with a mean time off work of 3.8 ± 1.8 months (range 1-8). The degree of satisfaction with the outcome of surgery was high or very high in 90% of the patients (very high 55%, high 35%, medium 7.5% and low 2.5%).
Conclusions: Arthroscopic hip surgery as a treatment for FAI in medical personnel results in improved functional parameters and allows an early return to work with the same level of activity as before the injury, with a low reintervention and conversion to THR rate after a mean follow-up over 7 years.
Level of evidence: Level IV study, retrospective case series.
Clinical relevance: The present study is the first to describe the demographics, occupational data, functional outcomes and need for revision AHS or conversion to THR in medical personnel undergoing AHS due to FAI.
Introduction
In view of its good results, arthroscopic hip surgery (AHS) has been gaining popularity as the treatment of choice for frequent hip joint injuries such as femoroacetabular impingement (FAI) and labral disorders(1). Most of the studies published to date have reported excellent results with this technique in the treatment of FAI, with significant improvement in pain and functional parameters, provided that the indication is made correctly and surgery is accompanied by adequate rehabilitation therapy(2).
A number of publications have analysed the outcomes of AHS in the treatment of FAI in different population groups, most of them involving professional athletes and military personnel, given their high functional demand. In professional athletes, the percentage return to sports activity is over 80%, and most athletes are able to return to their pre-injury level of activity(3). In the case of military personnel, around 75% remain in service for the first two years after surgery, although this percentage drops to 50% over medium term follow-up(4).
Although the level of physical activity in the medical profession is lower than that of professional athletes and military personnel, most physicians dedicate many hours to their work, with variable physical exertion. To date, no studies have examined the clinical and functional outcomes of AHS in the treatment of FAI among medical personnel. Our working hypothesis is that AHS offers this population group improved functional parameters with complications similar to those seen in the general population. The present study was carried out to evaluate the demographic characteristics, functional outcomes, satisfaction and return to work in a group of medical patients subjected to arthroscopic surgery for FAI by high-volume surgeons.
Material and methods
Patient selection
A retrospective review was made, using a multicentre database of patients with FAI subjected to AHS. The multicentre operating group consisted of 7 surgeons from 7 different hospital centres, with a minimum experience in this technique of 10 years and a minimum of 40 cases per year, all belonging to the Iberian Group of Hip Preservation Surgery (Grupo Ibérico de Cirugía de Preservación de Cadera [GIPCA]). All patients were evaluated by the surgeon in charge at each hospital centre. A joint encrypted database (Microsoft Excel, Microsoft Corporation, Redmond, WA, USA) was used for all centres for data collection and extraction, which was carried out by an independent analyst. The inclusion criteria were patients belonging to the medical profession undergoing AHS due to FAI. The exclusion criteria were revision surgery or AHS as treatment for other disorders (isolated tendon injuries, tumours or trauma).
Surgical technique
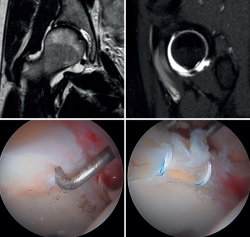
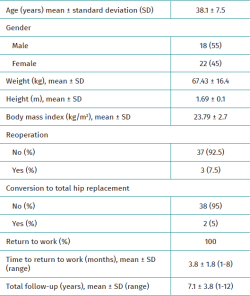
All surgeries were performed in the supine position and on a traction table with perineal post. The anterolateral, mid-anterior and distal anterolateral portals were used. In order to be able to perform the necessary procedures in each patient, an interportal capsulotomy was used in all cases in the central compartment (bony treatment of the acetabular rim, debridement of chondral lesions to secure stable edges, microfractures, labral debridement or repair), except in young women with signs of joint hyperlaxity, in which case independent capsulotomies were used (Figure 1). In patients with cam-type deformities (alpha angle >55°), a T-capsulotomy (with different edge traction systems, and only in those patients with difficult access to the femoral bump) was performed to gain access to the peripheral compartment and resect the femoral deformity until an adequate head-neck transition was achieved to prevent conflicts of space, tested by intraoperative dynamic examination to confirm adequate correction (Figure 2). The intraoperative procedures made are described in Table 1.
reacae.31181.fs2311029en-figure2.png
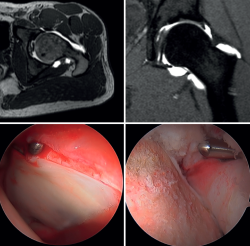
Figure 2. Combined femoroacetabular impingement in a middle-aged male patient. At top, axial and sagittal views of the preoperative MRI study, showing a deformity at the head-neck transition (left) and a chondrolabral junction lesion with excess coverage in the upper area (right). At bottom, intraoperative details of the chondrolabral junction lesion (left) and correction of the femoral deformity (right).
Clinical outcomes
Demographic data, functional scores preoperatively and one year after surgery, the need for reoperation or prosthetic surgery throughout follow-up, time and level of return to work, and satisfaction with the outcome of surgery at the end of follow-up were collected. The functional scales included the Hip Outcome Score-Activities of Daily Living (HOS-ADL) and the International Hip Outcome Tool 12 (i-HOT-12)(5,6). Calculation was made of the percentage of patients achieving a minimum clinically important difference (MCID), the patient acceptable symptom state (PASS), and the substantial clinical benefit (SCB) scores for both functional scales at one year after surgery. The MCID was defined as a postoperative increase of over 8.8 and 15.1 points, PASS as a postoperative score of over 89.7 and 69.1 points, and SCB as a postoperative score of over 89.7 and 72.6 points for the HOS-ADL and i-HOT12 scales, respectively(7).
Statistical analysis
Continuous variables were reported as the mean and standard deviation. Categorical variables were presented as percentages. In the case of the continuous variables, the Shapiro-Wilk test was used to assess normal distribution of the data. For continuous variables, the Student t-test or the Mann-Whitney U-test was used, as applicable. Statistical significance was considered for p < 0.5. The statistical analysis was performed using the SPSS version 26 statistical package (IBM Corporation, Armonk, NY, USA).
Results
Demographic data
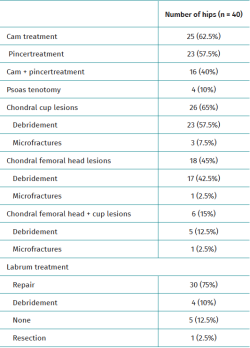
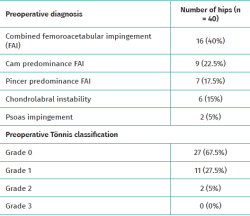
Out of a total of 43 patients, 40 (representing 40 hips) met the study inclusion criteria (93%). The mean age, weight, height and body mass index (BMI) were 38.1 ± 7.5 years, 67.4 ± 16.4 kg, 1.69 ± 0.1 m and 23.8 ± 2.7 kg/m2, respectively. There were 22 women (55%) and 18 men (45%). The demographic data, diagnoses and degree of preoperative joint degeneration are detailed in Tables 2 and 3.
Clinical outcomes and complications
The mean duration of follow-up was 7.1 ± 3.8 years (range 1-12). Statistically significant improvement of the HOS-ADL and i-HOT12 scores was recorded at one year after surgery (from 60.1 ± 14.1 and 40.4 ± 16.2 preoperatively to 87 ± 8.9 and 77 ± 11.6 postoperatively, respectively; p < 0.001). The percentage of patients achieving MCID, PASS and SCB at one year after surgery was 87.5%, 41.7% and 41.7% for the HOS-ADL scale, and 77.2%, 85.7% and 87.5% for the i-HOT12 scale, respectively. Five patients (12.5%) required reoperation during follow-up: two revision AHS (5%) due to labral suture failure; one adductor tenotomy (2.5%) due to inguinal pain and inability to perform full abduction; and two conversions to total hip replacement (THR) (5%) due to poor outcomes at 32 and 104 months after initial AHS. Both of these patients presented moderate chondral lesions (Tönnis classification grade 2) prior to first surgery.
Occupational outcomes
All patients returned to work after surgery, with a mean time off work of 3.8 ± 1.8 months (range 1-8). The percentage of patients on call or with shifts of more than 12 hours was the same before the injury and at the end of follow-up (4 out of 40; 10%). There were no statistically significant differences between the weekly working hours before the injury (45.4 ± 9.5) and at the end of follow-up (47.6 ± 10.9). Satisfaction with the outcome of surgery at the end of follow-up was high or very high in 90% of the patients (very high 55%, high 35%, average 7.5% and low 2.5%).
Discussion
The most relevant finding of the present multicentre study was that AHS as treatment for FAI allowed the medical personnel to fully return to work at a level similar to that before the injury, and with a high degree of satisfaction with the treatment received. In addition to the above, significant improvement of the functional parameters was achieved one year after the operation compared to the pre-treatment values.
There are data on the return to work after AHS in the general population, though most studies focus on elite athletes and military personnel(3,4,8,9,10,11). Although to varying degrees, the reported return to work rates are lower than those obtained in the present study. In the general population, the average percentage of patients returning to work at any level is 71.4%, with a range of 55-100%. The reported full return to work rate is 50.9%, while 15.5% (range 5-46) of the patients return to a lower or modified work intensity level(4). The average return to work time in the general population is 115 days, with a range from 17-219 days(8).
In athletes, the return to sports activity rate in general is 85%, with an average follow-up of around two years. The proportion of professional athletes who are able to return to elite sports ranges from 82-93.3%. This proportion decreases in the case of recreational sports, where the return rates vary between 66.7-84%(11). Approximately 70% of the athletes return to sports activity at a level similar to or higher than before the injury. The mean time to return to sports is 7.4 months(3).
In the case of military personnel, the return to service rate is around 75%. However, on analysing the proportion of military personnel that return to service without limitations (i.e., similar to the return to sports activity at pre-injury level in athletes), the figure is much lower (around 47%). The average time to return to service is highly variable, ranging from 1-2 years in some studies, and up to 6 years in others(4,9). Postoperative improvement of the pain and functional parameters is significantly higher in special forces and infantry personnel, with their return to service ratio being comparable to that of the return to sports activity in elite athletes(10). Although the medical profession is characterised by a lower level of activity than professional athletes or military personnel, in the present study 100% of the patients returned to their previous work activity, and both the percentage of patients working on call or in shifts of more than 12 hours and the number of weekly working hours did not differ between pre-injury and the end of follow-up. The mean time to return to work was under 120 days.
Although the return to work, sports or service has been used as a measure of success after AHS, functional parameters also contribute information on the outcomes achieved. All studies describe clinically and statistically significant improvement of functional parameters in athletes and military personnel when compared to the presurgery condition(10,12-20). In the present study, significant improvements were obtained in the postoperative values one year after the operation on the HOS-ADL and iHOT-12 scales compared to the presurgical values. In this same line, 87.5%, 41.7% and 41.7% of the patients achieved MCID, PASS and SCB with the HOS-ADL scale, versus 77.3%, 85.7% and 87.5% with the i-HOT12 scale, respectively. The difference in the percentage of patients achieving PASS and SCB between the two scales can be explained by the fact that the i-HOT12 questionnaire, unlike the HOS-ADL, assesses emotional, social, occupational and lifestyle aspects. Furthermore, while MCID assesses the proportion of patients achieving minimal clinical benefit, PASS and SCB assess the proportion of patients achieving complete and sufficient satisfaction, respectively.
Regarding the need for further surgery or conversion to THR, athletes are undoubtedly the most studied population group. The reoperation rate in this group ranges from 8.6-40% depending on the series(21-29). On strictly considering new hip preservation surgeries, the reoperation rate ranges from 3.6-15.2%. The frequency of conversion to THR ranges from 0-33.3%. In the present study the reoperation rate was low (12.5%), with a mean follow-up of 7 years; two were revision AHS due to failure of the previous labral suture, and one adductor tenotomy was performed due to inability for full abduction. The frequency of conversion to THR was also lower than in most published studies (2 cases; 5%), and conversion took place an average of 6 months after initial AHS. Both cases involved patients with moderate presurgical arthritic signs, Tönnis classification grade 2, where the indication of AHS is controversial.
The present study has a number of limitations. Firstly, the retrospective design of the study leads to selection bias. Secondly, the study does not take into account several factors that may have influenced the return to work, such as economic needs, social factors and disability insurance coverage issues. Thirdly, as this was a multicentre study, not all patients followed the same rehabilitation and recovery protocol. It is important to note that the present series represents the results of an experienced group of hip preserving surgeons in a specific population cohort; the results obtained therefore should be extrapolated with caution.
Conclusions
The results obtained indicate that AHS in medical personnel results in improved functional parameters and allows an early return to work with the same level of activity as before the injury, with a low reintervention and conversion to prosthetic surgery rate after a mean follow-up over 7 years.
Figuras
Figure 1. Chondrolabral injury in a young female patient. At top, coronal and sagittal views of the preoperative MRI study, showing the chondrolabral junction lesion in the anterosuperior region. At bottom, intraoperative details of the chondrolabral lesion (left) and after stabilisation (right).
Figure 2. Combined femoroacetabular impingement in a middle-aged male patient. At top, axial and sagittal views of the preoperative MRI study, showing a deformity at the head-neck transition (left) and a chondrolabral junction lesion with excess coverage in the upper area (right). At bottom, intraoperative details of the chondrolabral junction lesion (left) and correction of the femoral deformity (right).
Tablas
Información del artículo
Cita bibliográfica
Autores
David Serrano Toledano
Centro COT. Hospital Viamed Santa Ángela de la Cruz. Sevilla
Roberto Seijas Vázquez
Servicio de Cirugía Ortopédica y Traumatología. Fundación García-Cugat. Barcelona
Cirugía Ortopédica y Traumatología. Hospital Quirón. Barcelona
Servicio de Cirugía Ortopédica y Traumatología. Fundació Hospital de Mollet. Mollet del Vallès. Barcelona
Universitat Internacional de Catalunya. Barcelona
Javier Sanz Reig
Traumatología Vistahermosa. HLA Clínica Vistahermosa. Alicant
Grupo Ibérico de Preservación de Cadera (GIPCA)
Servicio de Cirugía Ortopédica y Traumatología. Clínica Vistahermosa. Alicante
Luis Pérez Carro
Servicio de Cirugia Ortopedica y Traumatología. Hospital Clínica Mompía. Santander. Cantabria.
Servicio de Cirugia Ortopedica y Traumatología. Hospital Marqués Valdecilla. Santander
Servicio de Cirugia Ortopedica y Traumatología. Centro Médico Lealtad. Santander
Miguel Cañones Martín
Hospital Universitario Infanta Leonor. Madrid
Jorge Fabián Urraza
Hospital Sanitas CIMA. Barcelona
Raúl Torres Eguia
Unidad de Cadera, Departamento de COT, Clínica CEMTRO, Madrid, España
Juan Ribera Zabalbescoa
Centro COT. Hospital Viamed Santa Ángela de la Cruz. Sevilla
Ethical responsibilities
Conflicts of interest. The authors state that they have no conflicts of interest.
Financial support. This study has received no financial support.
Protection of people and animals. The authors declare that this research has not involved human or animal experimentation.
Data confidentiality. The authors declare that the protocols of their work centre referred to the publication of patient information have been followed.
Right to privacy and informed consent. The authors have obtained informed consent from the patients and/or subjects cited in the article. The mentioned document is filed by the corresponding author.
Referencias bibliográficas
-
1Minkara AA, Westermann RW, Rosneck J, Lynch TS. Systematic review and meta-analysis of outcomes after hip arthroscopy in femoroacetabular impingement. Am J Sports Med. 2019;47(2):488-500.
-
2Menge TJ, Briggs KK, Dornan GJ, McNamara SC, Philippon MJ. Survivorship and outcomes 10 years following hip arthroscopy for femoroacetabular impingement: labral debridement compared with labral repair. J Bone Joint Surg Am. 2017;99(12):997-1004.
-
3Lee MS, Owens JS, Fong S, et al. Athletes report favorable outcomes at 5-year minimum follow-up after primary hip arthroscopy: a systematic review. Arthroscopy. 2023;39(2):510-28.
-
4Reiman MP, Peters S, Rhon DI. Most military service members return to activity duty with limitations after surgery for femoroacetabular impingement syndrome: a systematic review. Arthroscopy. 2018;34(09):2713-25.
-
5Martin RL, Kelly BT, Philippong MJ. Evidence of validity for the hip outcome score. Arthroscopy. 2006;22:1304-11.
-
6Martin RL, Philippon MJ. Evidence of reliability and responsiveness for the hip outcome score. Arthroscopy. 2008;24:676-82.
-
7Nwachukwu BU, Beck EC, Kunze KN, Chahla J, Rasio J, Nho S. Defining the clinically meaningful outcomes for arthroscopic treatment of femoroacetabular impingement syndrome at minimun 5-year follow up. Am J Sports Med. 2020;48(4):901-7.
-
8Blaeser AM, Mojica ES, Mannino BJ, Youm T. Return to work after primary hip arthroscopy. A systematic review and meta-analysis. Am J Sports Med. 2023;51(5):1340-6.
-
9Yoo JI, Lee TH, Kim JY, Kim JH, Chan YC. Outcomes of hip arthroscopy in a military population are similar to those in the civilian population: matched paired analysis at 2 years. Arthroscopy. 2018;34(7):2096-101.
-
10Thomas DD, Bernhardson AS, Bernstein E, Bewing CB. Hip arthroscopy for femoroacetabular impingement in a military population. Am J Sports Med. 2017;45(14):3298-304.
-
11O’Connor M, Westermann RW, Rosneck J, Lynch S. Returno to play after hip arthroscopy. A systematic review and meta-analysis. Am J Sports Med. 2018;46(11):2780-8.
-
12Boykin RE, Patterson D, Briggs KK, Dee A, Philippon MJ. Results of arthroscopic labral reconstruction of the hip in elite athletes. Am J Sport Med. 2013;41(10):2296-301.
-
13Byrd JT, Jones KS. Arthroscopic management of femoroacetabular impingement: minimum 2-year follow-up. Arthroscopy. 2011;27(10):1379-88.
-
14Klingenstein GG, Martin R, Kivlan B, Kelly BT. Hip injuries in the overhead athlete. Clin Orthop Relat Res. 2012;470(6):1579-85.
-
15Malviya A, Paliobeis CP, Villar RN. Do professional athletes perform better than recreational athletes after arthroscopy for femoroacetabular impingement? Clin Orthop Relat Res. 2013;471(8):2477-83.
-
16Polesello GC, Lima FR, Guimaraes RP, Ricioli W Jr, Queiroz MC. Arthroscopic treatment of femoroacetabular impingement: minimum five-year follow-up. Hip Int. 2014;24(4):381-6.
-
17Saavedra M, Moraga R, Díaz P, Camacho D, Mardones R. Comparative analysis of kinesiotherapy rehabilitation after hip arthroscopy, quantified by Harris and Vail hip scores: a retrospective study. Muscles Ligaments Tendons J. 2016;6(3):420.
-
18Sansone M, Ahldén M, Jonasson P, et al. Good results after hip arthroscopy for femoroacetabular impingement in top-level athletes. Orthop J Sports Med. 2015;3(2):1-8.
-
19Byrd JW, Jones KS, Schmitz LM, Doner GP. Hip arthroscopy in the warrior athlete: 2 to 10 years outcomes. J Hip Preservation Surg. 2016;3:68-71.
-
20Bennett AN, Nixon J, Roberts A, Barker-Davies R, Villar R, Houghton JM. Prospective 12-month functional and vocational outcomes of hip arthroscopy for femoroacetabular impingement as part of an evidence-based hip pain rehabilitation pathway in an active military population. BMJ Open Sport Exerc Med. 2016;2(1):e000144.
-
21Byrd JWT, Jones. KS. Hip arthroscopy in athletes: 10-year follow-up. Am J Sports Med 2009;37:2140-3.
-
22Jiménez AE, Monahan PF, Owens JS, et al. High-level athletes who did not return to sport for reasons unrelated to their hip achieve successful midterm outcomes with a benchmarking against high-level athletes who returned to sport. Arthroscopy. 2022;38:1879-87.
-
23Chen AW, Craig MJ, Yuen LC, Ortiz-Declet V, Maldonado DR, Domb BG. Five-year outcomes and return to sport of runner undergoing hip arthroscopy for labral tears with or without femoroacetabular impingement. Am J Sports Med. 2019;47:1459-66.
-
24Maldonado DR, Yelton MJ, Rosinsky PJ, et al. Return to play after hip arthroscopy among tennis players: outcomes with minimum five-year follow-up. BMC Musculoeskelt Disord. 2020;21(400).
-
25Jiménez AE, Glein RM, Owens JS, et al. Predictors of achieving the patient acceptable symptomatic state at minimum 5-year follow-up following primary hip arthroscopy in the adolescent athlete. J Pediatr Orthop. 2022;42:e277-e284.
-
26Perets I, Craig MJ, Mu BH, Maldonado DR, Litrenta JM, Domb BG. Midterm outcomes and return to sports among athletes undergoing hip arthroscopy. Am J Sports Med. 2018;46:1661-7.
-
27Lindman I, Öhlin A, Desai N, et al. Five-Year outcomes after arthroscopic surgery for femoroacetabular impingement syndrome in elite athletes. Am J Sports Med. 2020;48:1416-22.
-
28Jiménez AE, Monahn PF, Maldonado DR, et al. comparing midterm outcomes of high-level athletes versus nonathletes undergoing primary hip arthroscopy: a propensity-matched comparison with minimum 5-year follow-up. Am J Sports Med. 2021;49:3592-601.
-
29Menge TJ, Briggs KK, Rahl MD, Philippon MJ. Hip arthroscopy for femoroacetabular impingement in adolescents: 10-year patient-reported outcomes. Am J Sports Med. 2021;49:76-81.
Descargar artículo:
Licencia:
Este contenido es de acceso abierto (Open-Access) y se ha distribuido bajo los términos de la licencia Creative Commons CC BY-NC-ND (Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional) que permite usar, distribuir y reproducir en cualquier medio siempre que se citen a los autores y no se utilice para fines comerciales ni para hacer obras derivadas.
Comparte este contenido
En esta edición
- We are living a golden age in Spanish arthroscopic surgery
- Alteration of the coronal and sagittal axes of the knee and its implication in the failure of anterior cruciate ligament reconstruction. A systematic review
- Arthroscopic acetabular microfractures of the hip: survival and clinical outcome of the technique with a minimum follow-up of 5 years
- Hip arthroscopy provides medical personnel with an early and complete return to work. A multicentre study
- Novel articles on combined ligamentous injury of the anterior cruciate ligament and medial ligament complex of the knee
- Anteroinferior shoulder instability. Essential articles
- Treatment of shoulder instability with bone defects using a combination of arthroscopic bone block and <em>remplissage</em> techniques
- Reconstruction of the rotator cuff using a triple-row arthroscopic technique. Surgical technique
- Endoscopic treatment of calcific tendinitis of the gluteus maximus. A case report
- Incomplete discoid medial meniscus presenting coalescence with the anterior cruciate ligament
Más en PUBMED
Más en Google Scholar
Más en ORCID


Revista Española de Artroscopia y Cirugía Articular está distribuida bajo una licencia de Creative Commons Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional.