Treatment of shoulder instability with bone defects using a combination of arthroscopic bone block and remplissage techniques
Tratamiento de la inestabilidad de hombro con defectos óseos mediante la combinación de las técnicas artroscópicas de tope óseo y remplissage
Resumen:
Se describe la técnica de adición de remplissage a una técnica de tope óseo con autoinjerto de cresta ilíaca por método artroscópico. La indicación principal de este procedimiento es la inestabilidad glenohumeral anterior acompañada de una pérdida ósea crítica de la glenoides > 17,3%, además de la presencia de un defecto de Hill-Sachs que condiciona una lesión off-track. El procedimiento se puede desarrollar siguiendo los siguientes cuatro pasos: 1) obtención del injerto: se lleva a cabo mediante un abordaje sobre la cresta ilíaca para obtener un autoinjerto de 20 × 10 × 10 mm; 2) preparación del remplissage: consiste en la colocación de 1 o 2 anclajes en el defecto de Hill-Sachs y el paso de sus suturas a través de la cápsula posterior dejándolas sin anudar temporalmente. Mientras tanto, un segundo cirujano procede a realizar la preparación del injerto; 3) introducción y fijación del injerto: una vez preparado, el injerto se introduce y fija utilizando un sistema de suspensión para su correcto posicionamiento; 4) finalmente, para completar el procedimiento, se realiza la plicatura capsulolabral y el anudado de las suturas del remplissage.
Abstract:
The technique of adding remplissage to a bone block technique with an iliac crest autograft via arthroscopy is described. The main indication for this procedure is anterior glenohumeral instability accompanied by critical glenoid bone loss > 17.3%, in addition to the presence of a Hill-Sachs defect resulting in an off-tracklesion. The procedure can be carried out in four steps: 1) harvesting of the graft: this is carried out over the iliac crest to obtain a 20 × 10 × 10 mm autograft; 2) preparation of remplissage: this consists of placing 1 or 2 anchors in the Hill-Sachs defect and passing their sutures through the posterior capsule, leaving them temporarily untied. Meanwhile, a second surgeon proceeds to prepare the graft; 3) insertion and fixation of the graft: once prepared, the graft is inserted and fixed using a suspension system for its correct positioning; and 4) finally, to complete the procedure, capsulolabral plication and knotting of the remplissage sutures are performed.
Introduction
The decision to provide surgical treatment for patients with anterior glenohumeral instability has classically been reserved for those individuals with recurrent instability. However, the indication is changing in favour of surgical stabilisation after a first episode in patients with hyperlaxity and in young people involved in contact or competitive sports(1). In deciding the surgical approach, it is crucial to consider the percentage bone loss of the glenoid and proximal humerus. The Sugaya perfect circle technique is used to calculate the percentage of glenoid bone loss(1).
Due to the high frequency of concomitant glenoid and humeral head injuries, calculation of the glenoid contact area in relation to the humeral head, or glenoid track, was developed. This term, originally investigated by Yamamoto, analyses the area of contact between the humeral head and the glenoid in relation to bony injuries resulting from glenohumeral dislocation. In an anatomical study, he determined that the glenoid track in an uninjured shoulder corresponds to 84% of the glenoid width.
This figure was later modified to 83% in another study by Omori and published by Di Giacomo(2,3). Its calculation aims to assess the risk of Hill-Sachs lesion engagement with the anterior margin of the glenoid in the position of maximum abduction and external rotation of the shoulder(4). Knowledge of this parameter will help us in deciding the best surgical approach in each case. Thus, when the Hill-Sachs lesion interval is greater than the glenoid track value, it is considered to be an off-track lesion, indicating an increased risk of humeral head engagement. On the other hand, when the interval is smaller than the glenoid track value, it is referred to as an on-track lesion, and engagement in this case is very unlikely(5).
Although there is debate about the percentage of glenoid loss in decision making, it is considered appropriate to combine remplissage with the arthroscopic Bankart procedure in off-track lesions with losses < 25%(6). According to De Froda, for glenoid bone losses < 13.5%, a Bankart repair can be chosen in the presence of on-track lesions, and a remplissage procedure can be added if the lesions are off-track. It is therefore important in all cases to make a correct assessment of the bone lesions and their potential engagement or off-track effect. On the other hand, in the presence of glenoid losses > 17.3%, glenoid bone reconstruction is indicated(7).
Among the therapeutic options, the technique described by Michel Latarjet is widely known, though the current tendency is to increasingly use iliac crest autograft and allograft techniques(8). These free bone graft procedures are more anatomical alternatives, and their short-term results are promising(9).
This study presents an arthroscopic technique involving the combination of both procedures: bone block grafting and remplissage.
Presentation of the technique
Indications
Anterior glenohumeral shoulder instability is frequently associated with bipolar off-track bone lesions with glenoid loss > 17.3%, with treatment being based on glenoid reconstruction techniques. However, these procedures alone do not resolve bone loss of the proximal humerus. This posterior humeral head defect or Hill-Sachs lesion leads to increased recurrence of anterior glenohumeral instability. As treatment, the arthroscopic remplissage technique, described by Wolf and Pollack, involves advancing the infraspinatus tendon and posterior capsule to the bony defect of the humeral head using bone anchorings(10). As a result, the engagement effect disappears and dislocation is prevented(11). It is thus reasonable to postulate that the combination of a bone block procedure and a remplissage technique will offer better outcomes in these patients than each procedure separately, or in comparison to isolated Latarjet surgery(12).
Image assessment
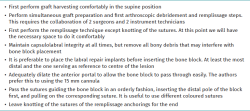
Computed arthrography (CT-arthrography) or magnetic resonance imaging (MRI) is used to determine the glenoid track in all cases. To measure the defects we use the tools provided by PACS (Picture Archiving and Communication System). To assess glenoid lesions, we must select the sagittal section where the defect is largest (generally the most superficial section). Similarly, to determine the Hill-Sachs interval, we use the axial view showing the greatest extension of the mentioned interval(13). The formula proposed by Di Giacomo is applied, and we determine the engaging or non-engaging nature of the lesions (Figure 1).
reacae.31181.fs2306016en-figure1.png
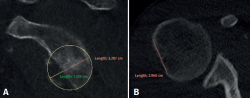
Figure 1. Measurement of the glenoid contact area or glenoid track. A: sagittal view showing the glenoid defect; B: axial view of the humeral head showing the Hill-Sachs interval, larger than the size of the Hill-Sachs lesion alone. In this case, it is a right shoulder with a Hill-Sachs interval greater than the calculation of the glenoid lesion. It is therefore an engaging or off-track injury.
Surgical technique
The procedure is carried out by combining two known techniques: the remplissage technique described by Wolf(10) and the bone block technique described by Taverna(14). We develop this in four steps (Video 1).
reacae.31181.fs2306016en-video1.png

Video 1. Two-technique procedure: remplissage and bone block. https://fondoscience.s3.eu-west-1.amazonaws.com/fs-reaca-videos/reaca.fs...
First step: harvesting of the graft
This is done with the patient in the supine position under general anaesthesia and interscalene block. A 3-cm approach is made over the anterosuperior iliac spine, and a graft measuring approximately 28 × 20 mm is obtained with the aid of an oscillating saw, adapting the amount to the size of the bone defect. However, a size of 20 × 10 × 10 mm is described as adequate(8). The wound is closed and the sterile fields are removed.
Second step: remplissage and graft preparation
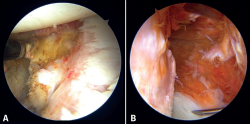
The patient is repositioned in lateral decubitus. Before placing the fields, a physical examination is performed to check glenohumeral instability with the modified anterior and posterior drawer tests(15). The humeral head is shown to engage in the glenoid with the arm in abduction and external rotation(6) (Video 1). Longitudinal traction is applied to the limb to be operated upon, according to the standard arthroscopy procedure. Arthroscopy is started through the posterior portal. An initial assessment of the location and extent of the lesions is made (Figure 2); the anterior portal is established under direct vision with the aid of a needle, 1-2 cm inferomedial to the anterolateral corner of the acromion, to penetrate within the rotator interval. An anterosuperior portal and a posteroinferior auxiliary portal are also established using an outside-in technique 2-3 cm below the posterior portal(16).
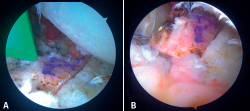
First, the glenoid is debrided with the aid of a shaver-type motor, and free bodies and bony debris are removed. The labrum and capsule are detached together from the glenoid margin, creating a wide recess to accommodate the graft, and the surface is prepared by creating bleeding edges with a burr. Then, using a posteroinferior auxiliary portal established under direct vision (Figure 3A), remplissage is started with debridement of the Hill-Sachs lesion and the placement of two bone implants - in this case HealicoilRegenesorb® (Smith & Nephew Inc., Andover, MA, USA) 4.5 mm double suture Ultrabraid® N.2 (Smith & Nephew Inc., Andover, MA, USA ) (Figures 3B and 3C). The 8 extremities are retrieved, passing them through the capsule approximately 1 cm apart and using a Sling-Shot® device (Stryker) (Figures 3D, 3E and 3F). The extremities are left untied in the posterior portal.
reacae.31181.fs2306016en-figure3.png
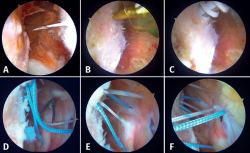
Figure 3. Performance of remplissage. A: location of the posteroinferior auxiliary portal under direct vision, checking good access to the Hill-Sachs lesion with a catheter; B: identification of the humeral defect and positioning of the punch; C: placement of the first anchoring in the distal part of the defect; D: retrieval of each suture through different points using the sling-shot passer; E: distribution of the four sutures of the first implant passed through at four different capsular points; F: distribution of the eight sutures of the two implants.
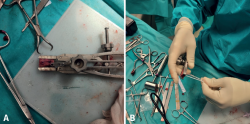
During this time, a second surgeon prepares the graft, giving it a rectangular shape and a size of 20 × 10 × 10 mm. To do so, he/she uses the instruments of the Glenoid Bone Loss® system (Smith & Nephew), drilling two holes with a 2.8 mm drill and spaced 10 mm apart, assisted by the specific graft preparation forceps (Figure 4A).
On the preparation table, one suture of the upper loop is passed through the upper orifice of the bone block and the lower loop through the lower orifice. These two suture loops are then used to close the double EndoButton® (Smith & Nephew) and thread the implant through each orifice of the block. Tightening is applied until both buttons are seated on the free surface of the bone block (Figure 4B).
Third step: insertion and fixation of the graft. Capsulolabral reconstruction
We then start the bone block technique, rearranging the posterior portal so that a Wissinger-Rod® guide (Smith & Nephew) is rested on the glenoid surface and can be directed to the centre of the glenoid defect (Figures 5A and 5B). Next, we slide a hemi-cannulated guide or Glenoid Drill Guide® (Smith & Nephew) over it, the Wissinger-Rod® is removed, and the hook-ended articular arm of the guide is passed through it. This is positioned in the centre of the glenoid defect and is assembled onto the guide handle. The two cannulas that guide the perforations are also passed through the same handle in a posterior-anterior direction, making point incisions in the skin. The assembly is adjusted and cannulated sheaths, each mounted on a specific 2.8-mm drill, are inserted through the two cannulas; drilling is made until they protrude at the anterior surface of the glenoid neck, followed by withdrawal until they are flush with the glenoid neck. A nylon loop is passed through each sheath to retrieve the sutures.
reacae.31181.fs2306016en-figure5.png
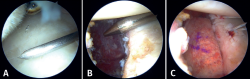
Figure 5. Rearrangement of the posterior portal for correct positioning of the hook-ended articular arm of the guide, resting on the surface of the glenoid and fixed in the centre of the lesion. A: with catheter; B: with Wissinger-Rod®; C: the position of the bone block is visualised prior to fixation of the suspension system.
Using the anterosuperior portal for vision, two anchorings are positioned for subsequent labral reconstruction. We use Suturefix Ultra® or Suturefix Curved® implants (Smith & Nephew), one at the midpoint of the lesion and another as distal as possible; we retrieve their extremities to the posterior portal.
Then, the bone block (lower part first) is guided through the metal cannula or directly through the extended anterior approach, followed by loop suture pulling and tightening, one by one. The bone block is positioned with the help of the hook guide. Once the position is considered to be satisfactory (Figure 5C), the implant sutures are passed through two buttons posteriorly using the suture retriever. Both are then advanced anteriorly (with a slip knot and a knot pusher) until they rest on the posterior surface of the glenoid neck (Figures 6A and 6B). Then, the sutures threaded to the posterior buttons are knotted using a Nice-type knot and tightened, as indicated by the technique, using a specific tensor up to 50 N. After doing this with both sutures, they are tightened again to 100 N and three safety half knots are added.
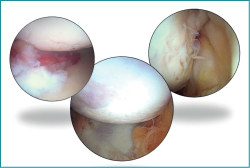
Fourth step: capsulolabral plication and knotting of the remplissage
Once the bone block is secured, the sutures of the implants previously placed at the anterior margin of the glenoid lesion are retrieved, and repair is carried out of the labrum and capsule over the bone graft according to the usual technique. Finally, the suture extremities of the implants placed in the Hill-Sachs lesion are knotted from the posterior portal, reducing the defect and completing the remplissage technique(17). The result obtained is assessed (Figure 7) and the procedure is completed by suturing the portals and immobilising the limb with a standard thoracic bandage.
Postoperative protocol
The postoperative period is divided into four phases, progressing from passive to active exercises, and on to muscle strengthening.
Phase 1 comprises the first three postoperative weeks and begins with passive mobility of the scapula in conjunction with active mobility of the elbow, wrist and fingers. Patients should wear the sling at all times except during hygiene or exercise(18).
Phase 2 starts in the fourth week. The aim here is to begin active mobility of the shoulder and to abandon the use of the sling. The focus should be on stretching the posterior capsule during the first two weeks of this phase. From the sixth postoperative week, passive internal and external rotation is started according to tolerance, with the shoulder in varying degrees of abduction, while active shoulder flexion is continued up to 145°.
Phase 3 begins approximately in the tenth postoperative week. Muscle strengthening of the subscapularis, biceps brachii, pectoralis major and the rest of the muscles should be started. At the end of this phase, active flexion, passive external rotation in abduction and adequate activity of the rotator cuff muscles should be completed.
Phase 4 begins at 16 weeks, focusing on activities above head level, and ends with functionality similar to that before the injury(18,19).
Advice and tips (Table 1)
Discussion
Recurrent anterior glenohumeral instability may be associated with larger bipolar bone defects. Although a significant Hill-Sachs lesion may occur in 23.1% of the cases after a first dislocation, important glenoid bone loss is observed in only 4.4% of the cases. However, repetitive events contribute to the formation of larger defects in both structures(20).
In addition, the age of the patient at the time of first dislocation also influences the size of the bipolar defect, with larger sizes occurring in patients > 30 years of age compared to younger individuals(20).
The preoperative assessment of this bipolar bone loss is crucial in therapeutic decision making, since intraoperative assessment to estimate glenoid bone loss may not always be accurate(21). The systematic use of radiological picture archiving and communication system (better known as PACS) tools is recommended for the assessment of these lesions. Accordingly, Shin et al. defined critical percentage glenoid bone loss as 17.3%, beyond which a procedure with reconstruction of the bone defect should be indicated(22). In their work, De Froda et al. established that arthroscopic repair is reliable in the presence of glenoid bone loss < 13.5% and, in agreement with Shin, they advise reconstruction of the bone defect in losses of over 17.3%. In addition, De Froda et al. defined what may be called a "grey" zone between 13.5% and 17.3%, where the decision should be individualised in each case. In sum, when glenoid bone loss > 17.3%, reconstruction of the glenoid bone defect would be indicated and, in cases where loss > 13.5% but < 17.3%, the activity level, expectations and goals of the patient should be taken into account in deciding between glenoid reconstruction versusarthroscopic Bankart repair(6,7).
According to Moroder, there are no clinical or radiographic differences between iliac crest bone block reconstruction techniques and Latarjet surgery in patients with anterior glenohumeral instability and bipolar bone loss(23). Posteriorly, Callegari, using models with bipolar bone loss, demonstrated that both procedures result in comparable biomechanical and clinical results. This suggests that both options may be equally effective in this group of patients(9). However, a cadaver study showed that when the humeral head defect exceeds 31%, the Latarjet technique fails to prevent dislocation. This suggests that, in injuries of this magnitude, it may also be necessary to correct the humeral head defect, such as with remplissage(24). According to studies in models such as those of Callegari, the addition of the latter technique to a bone block procedure results in greater resistance to anterior translation and greater force is required to cause dislocation compared to Latarjet surgery and a bone block procedure alone. Its addition should, in theory, reduce the risk of recurrence of instability and therefore justifies the use of the technique described in this article(9). Furthermore, although additional treatment of the humeral head defect during a Latarjet procedure is considered unnecessary, since it theoretically eliminates the engagement effect, it has been seen that this does not occur in 11.8% of the cases. This could be a cause of relapse even in the first two postoperative years(25).
Another reason why it is advisable to use a bone block technique compared to arthroscopic Latarjet is that it is technically less demanding. Furthermore, the latter is limited by the anatomy of the coracoid process, and its precise measurement for use as a graft can be arthroscopically complicated, unlike in bone block surgery, where harvesting and measurement can be done accurately(9).
Lastly, the main advantage of the described technique is that it allows the Hill-Sachs defect, the labral lesion and glenoid reconstruction to be addressed arthroscopically in the same surgical step. The combination of these procedures has been reported to improve shoulder stability, especially in the presence of significant bipolar defects(26). In addition, the graft can be precisely measured and accurately modified(9).
Conclusions
Because of the reported advantages of arthroscopic bone block procedures and the need for humeral head augmentation in large off-track type bipolar defects, this surgical technique is presented with the aim of enabling its replication. It is expected that this technique may potentially involve fewer complications compared to non-anatomical techniques.
Supplementary material
The video of the technique accompanying this article can be seen at (Video 1):
Figuras
Figure 1. Measurement of the glenoid contact area or glenoid track. A: sagittal view showing the glenoid defect; B: axial view of the humeral head showing the Hill-Sachs interval, larger than the size of the Hill-Sachs lesion alone. In this case, it is a right shoulder with a Hill-Sachs interval greater than the calculation of the glenoid lesion. It is therefore an engaging or off-track injury.
Video 1. Two-technique procedure: remplissage and bone block. https://fondoscience.s3.eu-west-1.amazonaws.com/fs-reaca-videos/reaca.fs...
Figure 2. Corroboration of injuries. A: of the glenoid; B: of the humeral head. A right shoulder with anterosuperior viewing portal for this and the rest of the figures.
Figure 3. Performance of remplissage. A: location of the posteroinferior auxiliary portal under direct vision, checking good access to the Hill-Sachs lesion with a catheter; B: identification of the humeral defect and positioning of the punch; C: placement of the first anchoring in the distal part of the defect; D: retrieval of each suture through different points using the sling-shot passer; E: distribution of the four sutures of the first implant passed through at four different capsular points; F: distribution of the eight sutures of the two implants.
Figure 4. Detail of the preparation of the bone block with the specific instrumentation of the Glenoid Bone Loss® system (Smith & Nephew). A: the amount of bone graft harvested is measured; B: sutures have been threaded over the buttons, which have been seated on the free surface of the graft.
Figure 5. Rearrangement of the posterior portal for correct positioning of the hook-ended articular arm of the guide, resting on the surface of the glenoid and fixed in the centre of the lesion. A: with catheter; B: with Wissinger-Rod®; C: the position of the bone block is visualised prior to fixation of the suspension system.
Figure 6. Position of the graft in the bone block technique during fixation and after fixation with the suspension system.
Figure 7. Photomontage of the result obtained: the image at left shows reduction of the labrum over the graft; the central image shows final centring of the humeral head; and the image at right shows reduction of the posterior recess after the knotting of the remplissage.
Tablas
Información del artículo
Cita bibliográfica
Autores
Omar Agüero Álvarez
Hospital Instituto Nacional de Rehabilitación. Ciudad de México
Hospital Policlínica Gipuzkoa. Grupo Quirónsalud. Donostia. San Sebastián
Asier Cuéllar Ayestarán
Instituto Vasco de Cirugía Ortopédica-Traumatología (IVCOT). Policlínica Gipuzkoa Quirón-Salud. Donostia-San Sebastián, Gipuzkoa
Adrián Cuéllar Ayestarán
Instituto Vasco de Cirugía Ortopédica-Traumatología (IVCOT). Policlínica Gipuzkoa Quirón-Salud. Donostia-San Sebastián, Gipuzkoa
Ricardo Cuéllar Gutiérrez
Instituto Vasco de Cirugía Ortopédica-Traumatología (IVCOT). Policlínica Gipuzkoa Quirón-Salud. Donostia-San Sebastián, Gipuzkoa
Ethical responsibilities
Conflicts of interest. The authors state that they have no conflicts of interest.
Financial support. This study has received no financial support.
Protection of people and animals. The authors declare that this research has not involved human or animal experimentation.
Data confidentiality. The authors declare that the protocols of their work centre referred to the publication of patient information have been followed.
Right to privacy and informed consent. The authors declare that no patient data appear in this article.
Referencias bibliográficas
-
1Moya D, Aydin N, Yamamoto N, et al. Current concepts in anterior glenohumeral instability: diagnosis and treatment. SICOT J. 2021;7:48.
-
2Giacomo GD, Itoi E, Burkhart SS. Evolving Concept of Bipolar Bone Loss and the Hill-Sachs Lesion: From “Engaging/Non-Engaging” Lesion to “On-Track/Off-Track” Lesion. Arthroscopy. 2014;30(1):90-8.
-
3Yamamoto N, Itoi E, Abe H, et al. Contact between the glenoid and the humeral head in abduction, external rotation, and horizontal extension: a new concept of glenoid track. J Shoulder Elbow Surg. 2007;16(5):649-56.
-
4Awh M. Off-track Shoulder Lesions. Radsource; 2021. Disponible en: https://radsource.us/off-track-shoulder-lesions/.
-
5Mook WR, Petri M, Greenspoon JA, Horan MP, Dornan GJ, Millett PJ. Clinical and Anatomic Predictors of Outcomes After the Latarjet Procedure for the Treatment of Anterior Glenohumeral Instability With Combined Glenoid and Humeral Bone Defects. Am J Sports Med. 2016;44(6):1407-16.
-
6Ezagüi L, Baggio L, Brotat M, Gómez Cáceres A, Yebra Pareja JC. Manejo de la inestabilidad anterior de hombro con defectos óseos. Rev Esp Artrosc Cir Articul. 2021;28(3). Disponible en: https://fondoscience.com/reaca/vol28-fasc3-num73/fs2007039-manejo-inestabilidad-anterior-hombro.
-
7DeFroda S, Bokshan S, Stern E, Sullivan K, Owens BD. Arthroscopic Bankart Repair for the Management of Anterior Shoulder Instability: Indications and Outcomes. Curr Rev Musculoskelet Med. 2017;10(4):442-51.
-
8Delgado Del Caño C, Díaz Heredia J, Ruiz Díaz R, et al. Bloque óseo artroscópico anterior con sistema de fijación de doble botón cortical con guía posterior para la inestabilidad anterior de hombro con defecto glenoideo. Técnica quirúrgica. Rev Esp Artrosc Cir Articul. 2021;28(4). Disponible en: https://fondoscience.com/reaca/vol28-fasc4-num74/fs2110033-bloque-oseo-artroscopico-anterior.
-
9Callegari JJ, McGarry M, Crook L, et al. The Addition of Remplissage to Free Bone Block Restores Translation and Stiffness Compared to Bone Block Alone or Latarjet in a Bipolar Bone Loss Model. Arthroscopy. 2022;38(9):2609-17.
-
10Buza JAI, Iyengar JJ, Anakwenze OA, Ahmad CS, Levine WN. Arthroscopic Hill-Sachs Remplissage: A Systematic Review. JBJS. 2014;96(7):549.
-
11Hurley ET, Toale JP, Davey MS, et al. Remplissage for anterior shoulder instability with Hill-Sachs lesions: a systematic review and meta-analysis. J Shoulder Elbow Surg. 2020;29(12):2487-94.
-
12Feldman MD. Editorial Commentary: Free Bone Block With Remplissage Provides Less Translation Than Free Bone Block Alone in Shoulder Instability Patients With Bipolar Bone Loss. Arthrosc J Arthrosc Relat Surg. 2022;38(9):2618-9.
-
13Gyftopoulos S, Beltran LS, Bookman J, Rokito A. MRI Evaluation of Bipolar Bone Loss Using the On-Track Off-Track Method: A Feasibility Study. Am J Roentgenol. 2015;205(4):848-52.
-
14Taverna E, Garavaglia G, Perfetti C, Ufenast H, Sconfienza LM, Guarrella V. An arthroscopic bone block procedure is effective in restoring stability, allowing return to sports in cases of glenohumeral instability with glenoid bone deficiency. Knee Surg Sports Traumatol Arthrosc. 2018;26(12):3780-7.
-
15Cuéllar R, González J, De La Herrán G, Usabiaga J. Exploration of Glenohumeral Instability Under Anesthesia: The Shoulder Jerk Test. Arthrosc J Arthrosc Relat Surg. 2005;21(6):672-9.
-
16Paxton ES, Backus J, Keener J, Brophy RH. Shoulder Arthroscopy: Basic Principles of Positioning, Anesthesia, and Portal Anatomy. J Am Acad Orthop Surg. 2013;21(6):332-42.
-
17Memon SD, Dimock RAC, Shah J, Ajami S, Imam M, Narvani AA. Arthroscopic Allograft Bone Block Procedure with Remplissage for Bipolar Lesions. Arch Bone Joint Surg. 2022;10(10):899-910.
-
18Fedorka CJ, Mulcahey MK. Recurrent anterior shoulder instability: a review of the Latarjet procedure and its postoperative rehabilitation. Phys Sportsmed. 2015;43(1):73-9.
-
19Brigham and Women's Hospital. Department of Rehabilitation Services. Anterior Stabilization of the Shoulder: Latarjet Protocol. Disponible en: https://www.brighamandwomens.org/assets/BWH/patients-and-families/rehabilitation-services/pdfs/shoulder-latarjet.pdf.
-
20Nakagawa S, Sahara W, Kinugasa K, Uchida R, Mae T. Bipolar Bone Defects in Shoulders With Primary Instability: Dislocation Versus Subluxation. Orthop J Sports Med. 2021;9(5):232596712110035.
-
21Gouveia K, Rizvi SFH, Dagher D, Leroux T, Bedi A, Khan M. Assessing Bone Loss in the Unstable Shoulder: a Scoping Review. Curr Rev Musculoskelet Med. 2022;15(5):369-76.
-
22Shin SJ, Kim RG, Jeon YS, Kwon TH. Critical Value of Anterior Glenoid Bone Loss That Leads to Recurrent Glenohumeral Instability After Arthroscopic Bankart Repair. Am J Sports Med. 2017;45(9):1975-81.
-
23Moroder P, Schulz E, Wierer G, et al. Neer Award 2019: Latarjet procedure vs. iliac crest bone graft transfer for treatment of anterior shoulder instability with glenoid bone loss: a prospective randomized trial. J Shoulder Elbow Surg. 2019;28(7):1298-307.
-
24Patel RM, Walia P, Gottschalk L, et al. The Effects of Latarjet Reconstruction on Glenohumeral Kinematics in the Presence of Combined Bony Defects: A Cadaveric Model. Am J Sports Med. 2016;44(7):1818-24.
-
25Calvo C, Calvo J, Rojas D, Valencia M, Calvo E. Clinical Relevance of Persistent Off-Track Hill-Sachs Lesion After Arthroscopic Latarjet Procedure. Am J Sports Med. 2021;49(8):2006-12.
-
26Bonnevialle N, Baltassat A, Martinel V, Barret H, Mansat P. Arthroscopic Distal Clavicle Bone Bock Combined With Hill-Sachs Remplissage for Primary Anterior Shoulder Instability Treatment. Arthrosc Tech. 2024;13(3):102882.
Descargar artículo:
Licencia:
Este contenido es de acceso abierto (Open-Access) y se ha distribuido bajo los términos de la licencia Creative Commons CC BY-NC-ND (Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional) que permite usar, distribuir y reproducir en cualquier medio siempre que se citen a los autores y no se utilice para fines comerciales ni para hacer obras derivadas.
Comparte este contenido
En esta edición
- We are living a golden age in Spanish arthroscopic surgery
- Alteration of the coronal and sagittal axes of the knee and its implication in the failure of anterior cruciate ligament reconstruction. A systematic review
- Arthroscopic acetabular microfractures of the hip: survival and clinical outcome of the technique with a minimum follow-up of 5 years
- Hip arthroscopy provides medical personnel with an early and complete return to work. A multicentre study
- Novel articles on combined ligamentous injury of the anterior cruciate ligament and medial ligament complex of the knee
- Anteroinferior shoulder instability. Essential articles
- Treatment of shoulder instability with bone defects using a combination of arthroscopic bone block and <em>remplissage</em> techniques
- Reconstruction of the rotator cuff using a triple-row arthroscopic technique. Surgical technique
- Endoscopic treatment of calcific tendinitis of the gluteus maximus. A case report
- Incomplete discoid medial meniscus presenting coalescence with the anterior cruciate ligament
Más en Google Scholar


Revista Española de Artroscopia y Cirugía Articular está distribuida bajo una licencia de Creative Commons Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional.