Endoscopic treatment of calcific tendinitis of the gluteus maximus. A case report
Tratamiento endoscópico de tendinitis calcificante del glúteo mayor. A propósito de un caso
Resumen:
La tendinitis calcificante es una patología frecuente; en cambio, su prevalencia y localización en el tendón del glúteo mayor es extremadamente rara y se dispone de escasa bibliografía sobre su tratamiento. Presentamos un caso de una mujer de 46 años que presentaba dolor en la región posterolateral de la cadera, junto con radiculopatía ipsilateral, secundarios a tendinitis calcificante del glúteo mayor. Debido a la gravedad, cronicidad y resistencia de los síntomas, se realizó intervención quirúrgica consistente en limpieza endoscópica intratendón. Los controles radiográficos postoperatorios demuestran una extirpación prácticamente completa. La paciente se mantiene asintomática y sin recurrencia al año de la intervención. Solo existe publicado un caso semejante a este con éxito similar.
La endoscopia debe ser considerada como una opción de tratamiento eficaz frente a la tendinitis calcificante del glúteo mayor resistente al tratamiento conservador, presentando adicionalmente la menor morbilidad de la cirugía endoscópica con respecto a la cirugía abierta.
Abstract:
While calcific tendinitis is a common disorder, its prevalence and location in the gluteus maximus tendon is extremely rare, and there is little literature on its treatment. We present the case of a 46-year-old woman who presented with pain in the posterolateral region of the hip, together with ipsilateral radiculopathy, secondary to calcific tendinitis of the gluteus maximus. Due to the severity, chronicity and resistance of the symptoms, surgery consisting of endoscopic intratendon cleaning was decided. The postoperative radiographic examinations demonstrate virtually complete excision. The patient remains asymptomatic and without recurrence one year after surgery. There is only a single previous published case similar to this one, reporting similar success.
Endoscopy should be considered as an effective treatment option for calcific tendinitis of the gluteus maximus resistant to conservative management, with the additional advantage of the lesser morbidity of endoscopic surgery compared to open surgery.
Introduction
Calcific tendinitis is a relatively common disorder, caused by the excessive depositing of calcium hydroxyapatite crystals in the tendons. It typically affects patients between the third and sixth decades of life, with a higher prevalence in females. The joints most commonly involved in this disorder are the shoulder and hip(1). Calcific tendinitis in the proximity of the coxofemoral joint accounts for 5.4% of all cases in individuals over 15 years of age, occurring most frequently in the tendons of the rectus femoris and gluteus medius(2). The initial treatment of calcific tendinitis consists of oral nonsteroidal antiinflammatory drugs, physiotherapy, image-guided corticosteroid infiltration, high-intensity focused ultrasound, percutaneous ultrasound-guided barbotage, and shockwave therapy(3). The main indication for surgery is in cases that prove refractory to conservative treatment, with symptoms that limit the activities of daily living.
There is a significant number of articles in the literature on the endoscopic treatment of calcific tendinitis of the gluteus medius. In contrast, there is not much evidence on the surgical treatment of calcific tendinitis of the gluteus maximus. In an exhaustive literature search, we found only one article (a case report) describing endoscopic treatment for this condition(4). The present study describes a case of calcific tendinitis of the gluteus maximus successfully treated by endoscopic surgery.
Clinical case
The patient was a 46-year-old woman presenting chronic pain for the past three years, with an insidious onset, located in the posterolateral area of the right hip, at the level of the insertion of the gluteus maximus tendon. In addition, she reported radiculopathy in the right lower limb, with dysesthesia.
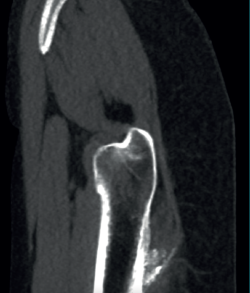
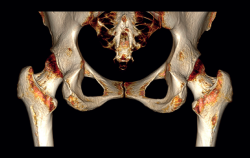
The physical examination revealed a limp-free gait and complete joint balance, with no positive signs of femoroacetabular impingement or inguinal pain. Muscle strength was preserved and similar to that of the contralateral side. She experienced intense pain on palpation of the insertion of the gluteus maximus, referred proximally to the ipsilateral buttock. The pain was reproduced on extension against resistance, and prevented sitting for long periods. Plain radiographic and computed tomography (CT) images revealed calcific tendinosis affecting the aponeurotic prolongation of the gluteus maximus in proximity to its insertion in the upper region of the linea aspera of the femur (Figures 1 and 2) Magnetic resonance imaging (MRI) of the hip showed a labral tear, that proved asymptomatic in the physical examination. In view of the clinical picture of radicular pain, an MRI scan of the lumbar spine and subgluteal space was also performed, ruling out radicular involvement or sciatic neuritis. Her previous treatment over the three years of evolution of the disorder included oral nonsteroidal anti-inflammatory drugs, a specific physiotherapy programme and several ultrasound-guided corticosteroid injections with positive results - though a last session showed no response. Due to the severity and chronicity of the symptoms and their resistance to conservative treatment, surgery was decided to clean and remove the intratendon calcification endoscopically.
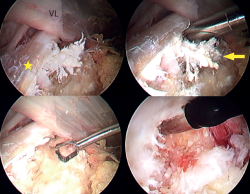
Under combined (spinal and general) anaesthesia, the patient was placed on the traction table in supine decubitus with the contralateral leg in abduction. The hip to be operated upon was placed in 10-15ºflexion with slight approximation towards the neutral midline. The hip was minimally distracted by the longitudinal traction combined with pressure from a perineal post, and the foot of the leg to be operated upon was internally rotated to bring the femoral neck parallel to the floor, tilting the table 10° towards the opposite side. The calcification was then located using fluoroscopy, and two portals were created in the peritrochanteric space using the all inside technique. The first (vision) portal was located at the level of the vastus crest in the area of the modified anterior portal, and the second (working) portal was located distal and anterolateral at the level of the calcification. A trochanteric bursectomy was performed to visualise the gluteus maximus tendon and, once the latter was located, the calcification was identified, characterised by a whitish colour with a coral-like appearance and pasty consistency, and then removed using motorised instruments, curette and radiofrequency (Figure 3). Finally, the integrity of the tendon was checked, and complete removal of the calcification was confirmed under visual control. Postoperatively, a nonsteroidal antiinflammatory drug (naproxen) was prescribed for three weeks as prophylaxis for heterotopic ossifications.
A usual rehabilitation protocol after hip arthroscopy / endoscopy was applied, with crutch-assisted weight bearing for three weeks and circumduction movements plus stationary cycling for 15 minutes, four times a day. The patient was advised to avoid extension and long stride exercises in order to prevent possible gluteus maximus tendon injuries. She reported complete reversal of the symptoms, including the radicular pain, with a return to physical activity and sports three months after surgery. One year after the operation, the patient remained asymptomatic in any activity, with complete disappearance and no recurrence of the calcification (Figure 4).
Discussion
Calcific tendinitis evolves in different phases, each characterised by specific radiological images and symptoms. The disorder begins with the formative phase, in which a region of the tendon, for an unknown reason, undergoes fibrocartilaginous transformation. This is followed by a calcification phase that may cause pain of mechanical characteristics. The next phase is the resorptive phase, characterised by peripheral neovascularisation and the migration of macrophages that absorb the calcium deposit. This is the stage of greatest pain intensity. Finally, in the reabsorption phase, the fibroblasts restore the normal pattern of the tendon(1). The hip is the second most common joint affected by calcific tendinitis. The tendons most frequently involved are those of the rectus femoris (the direct head more than the indirect head of the muscle). These are followed by the gluteal tendons (with a greater prevalence of the medius over the maximus) and, to a lesser extent, other tendons such as those of the adductors, the piriformis, the iliopsoas, the ischiotibial and the sartorius muscles.
Depending on the tendon affected, the differential diagnosis includes various conditions: infections, tumours (such as parosteal osteosarcoma), lumbar radiculopathy, avulsion fracture, myositis ossificans, os acetabuli or sesamoid bones(5).
In terms of anatomy, the gluteus maximus originates from the posterior gluteal line, the posterior surface of the sacrum and coccyx, and the sacrotuberous ligament. Its upper fibres insert into the iliotibial band, and the lower fibres insert into the linea aspera of the femur. This muscle is innervated by the inferior gluteal nerve (L5, S1 and S2). Its actions are thigh extension and external rotation of the femur(5).
Calcific tendinitis of the gluteus maximus typically occurs in the fibres that insert on the posterolateral aspect of the femur(8). With regard to the clinical features of calcific tendinitis of the gluteus maximus, the pain usually has an insidious onset with periods of exacerbation related to physical activity. The acute symptoms, understood as lasting less than three weeks, are related to larger initial lesions, and are more prevalent in young patients. The symptomatology in such cases is of greater intensity and recovery is more satisfactory compared to patients with chronic symptoms. Calcifications with delimited margins respond better to treatment than lesions with irregular margins(9).
On physical examination, hip range of motion is full, painless and symmetrical to the contralateral side. Moreover, muscle strength is usually preserved and walking is usually normal, though antalgic gait may be observed. Of note is intense pain on palpation in the affected buttock and over the femoral insertion of the gluteus maximus tendon, distal to the trochanteric bursa(10,11). Cases of sciatic pain together with a positive neural tension test (seated slump test)have also been described(8,12,13). In these cases the differential diagnosis should be made with so-called deep gluteal syndrome, a syndrome characterised by pain and/or dysesthesia in the buttock, hip or posterior thigh, together with radicular pain due to impingement of the sciatic nerve, which is located posterior to the insertion of the gluteus maximus at a distance of 3-6 cm, in the subgluteal space. One of the causes of this is compressive fibrous bands running between the posterior surface of the greater trochanter and the gluteus maximus(14,15,16).
In cases of calcific tendinopathy of the gluteus maximus, calcifications in the femoral metaphysis can be seen on plain radiographs, though a normal image may also be seen. Therefore, CT and/or MRI scans are usually necessary for establishing the diagnosis, exhibiting an irregularity or cortical erosion at the insertion of the gluteus maximus in the gluteal tuberosity, located on the posterolateral surface of the femur, distal to the greater trochanter, accompanied by areas of tendon calcification, local inflammatory signs and, in some cases, partial intratendinous ruptures(17). Use can also be made of CT-guided single-photon emission computed tomography (SPECT-CT), which pinpoints the anatomical location and assesses the activity of the lesion, and is of interest in the differential diagnosis in oncological patients(18).
Regarding the treatment of calcific tendinitis and specifically concerning the aforementioned disorder of the gluteus maximus tendon, the initial indication is conservative treatment, based on the prescription of oral nonsteroidal antiinflammatory drugs and physiotherapy. Sang-Min Park et al. reported that in 66% of the cases, the symptoms caused by calcific tendinitis were resolved within 2.5 months, without the need for any interventional technique or surgery(3). In patients who do not respond to conservative treatment, techniques such as imaging-guided corticosteroid infiltration, high-intensity focused ultrasound, percutaneous ultrasound-guided barbotage, and shockwave therapy are indicated. Hema Nalini Choudur et al. described imaging-guided (fluoroscopy or CT) corticosteroid-anaesthesia infiltration in these cases, achieving a return to daily activities in all patients, with complete resolution of the pain within a maximum period of 6 months(19). Hannae Jo et al. described percutaneous ultrasound-guided barbotage in a patient where conservative treatment and shock wave therapy had been ineffective - achieving both symptoms relief and resolution of the calcification on the radiographs(13). Kwang-Jun Oh et al. used shockwave therapy for the treatment of calcific tendinitis around the hip, achieving optimal clinical and radiological outcomes with a follow-up period of 15 months(20). Champ L. Baker et al. described percutaneous ultrasound-guided tenotomy for gluteal tendinopathy, achieving pain relief and functional improvement as assessed by validated questionnaires, with no reported complications(21).
Surgery is indicated in cases where both conservative treatment and the techniques described above prove ineffective and the symptoms limit the activities of daily living of the patient. Manoj Kumar et al. presented a case of calcific tendinitis of the gluteus maximus treated by open surgery with a large incision size and extensive soft tissue dissection(8). Ariel A. Williams et al. in turn described a similar case in a golfer. The authors performed open surgery involving debridement of the tendinosis and repair of the tendon using sutures with anchorings(10). Regarding the endoscopic technique, most of the published articles refer to the treatment of calcific tendinitis of the gluteus medius. In 2003, Utku Kandemir et al. reported the first case of calcific tendinitis of the gluteus medius and minimus subjected to endoscopic surgery, recommending this technique due to its effectiveness and low morbidity(22). Subsequently, Chen Jean et al. and Lee Wen Qiang et al. successfully reproduced this endoscopic debridement technique in similar patients(23,24). Justin J. Mitchell et al. described the endoscopic surgical technique for trochanteric bursectomy and iliotibial band lengthening for the treatment of trochanteric bursitis. Although such surgery is technically demanding, it offers complete visualisation of the trochanteric bursal space, as well as certain advantages over the open technique: minimal incisions, less soft tissue dissection and reduced blood losses(25).
In 2021, Charles A. Su et al. published for the first time an article on the endoscopic treatment of calcific tendinitis of the gluteus maximus involving trochanteric bursectomy and debridement of the calcification in a manner similar to that described in this case(4). The use of nonsteroidal antiinflammatory drugs to prevent postoperative calcifications was published by Randelli in arthroscopic hip surgery, evidencing high efficacy(26). The present study describes the second case of calcific tendinitis of the gluteus maximus treated by endoscopic surgery, considering it to be a reproducible and effective technique.
Conclusions
Endoscopic surgery for calcific tendinitis of the gluteus maximus allows controlled excisional debridement under direct vision, with the additional advantages of less morbidity, smaller incisions, less soft tissue injury (including a lesser risk of sciatic nerve problems thanks to the direct and magnified vision), less blood loss, a shorter exposure time and therefore less risk of infection, and much faster recovery compared with open surgery.
Figuras
Figure 1. Right hip. Posteroanterior 3D CT view showing calcific tendinosis affecting the aponeurotic prolongaation of the gluteus maximus in proximity to its insertion in the upper region of the linea aspera of the femur (arrow).
Figure 2. Right hip. Sagittal CT view showing calcification of the gluteus maximus at the insertion site on the femur.
Figure 3. Right hip. Arthroscopic view in the peritrochanteric space showing a whitish, coral-shaped calcification (arrow) at the insertion area of the gluteus maximus tendon in the femur (star). Removal using motorised instruments, curette and radiofrequency. VL: vastus lateralis.
Información del artículo
Cita bibliográfica
Autores
Luis Pérez Carro
Servicio de Cirugia Ortopedica y Traumatología. Hospital Clínica Mompía. Santander. Cantabria.
Servicio de Cirugia Ortopedica y Traumatología. Hospital Marqués Valdecilla. Santander
Servicio de Cirugia Ortopedica y Traumatología. Centro Médico Lealtad. Santander
Luis Antonio Ruiz Villanueva
Hospital Mompía. Santander, Cantabria
Óscar Pérez Fernández
Facultad de Medicina Universidad de Cantabria
Hospital Mompía. Santander, Cantabria
Alvaro Cerezal
Hospital Universitario La Paz. Madrid
Lorena Trueba Sánchez
Hospital Mompía. Santander, Cantabria
Cirugía Ortopédica y Traumatología. Hospital Universitario de Burgos
Santiago Abad Repiso
Hospital Mompía. Santander, Cantabria
Servicio de Cirugía Ortopédica y Traumatología. Centro Médico Lealtad. Santander
Ethical responsibilities
Conflicts of interest. The authors state that they have no conflicts of interest.
Financial support. This study has received no financial support.
Protection of people and animals. The authors declare that this research has not involved human or animal experimentation.
Data confidentiality. The authors declare that the protocols of their work centre referred to the publication of patient information have been followed.
Right to privacy and informed consent. The authors declare that no patient data appear in this article.
Referencias bibliográficas
-
1Siegal DS, Wu JS, Newman JS, Del Cura JL, Hochman MG. Calcific tendinitis: a pictorial review. Can Assoc Radiol J. 2009;60(5):263-72.
-
2Pope TL Jr, Keats TE. Case Report 733. Calcific Tendinitis of the Origin of the Medial and Lateral Heads of the Rectus Femoris Muscle and the Anterior Iliac Spin (AIIS). Skeletal Radiol. 1992;21(4):271-2.
-
3Park SM, Baek JH, Ko YB, Lee HJ, Park KJ, Ha YC. Management of acute calcific tendinitis around the hip joint. Am J Sports Med. 2014;42(11):2659-65.
-
4Su CA, Ina JG, Raji Y, Strony J, Philippon MJ, Salata MJ. Endoscopic Treatment of Calcific Tendinitis of the Gluteus Maximus: A Case Report. JBJS Case Connect. 2021;11(2):e20.00974-6.
-
5Draghi F, Cocco G, Lomoro P, Bortolotto C, Schiavone C. Non-rotator cuff calcific tendinopathy: ultrasonographic diagnosis and treatment. J Ultrasound. 2020;23(3):301-15.
-
6Mascarenhas R, Frank RM, Lee S, Salata MJ, Bush-Joseph C, Nho SJ. Endoscopic Treatment of Greater Trochanteric Pain Syndrome of the Hip. JBJS Rev. 2014;2(12):e2.
-
7Philippon MJ, Michalski MP, Campbell KJ, et al. Surgically Relevant Bony and Soft Tissue Anatomy of the Proximal Femur. Orthop J Sports Med. 2014;2(6):2325967114535188.
-
8Kumar M, D’Silva DF, Shah M, Parekh G. Calcific Tendonitis of the Gluteus Maximus Tendon: A Case Report and Review of the Literature. J Mahatma Gandhi Inst Med Sci. 2016;21(1):65.
-
9Yi SR, Lee MH, Yang BK, et al. Characterizing the Progression of Varying Types of Calcific Tendinitis around Hip. Hip Pelvis. 2015;27(4):265-72.
-
10Williams AA, Stang TS, Fritz J, Papp DF. Calcific Tendinitis of the Gluteus Maximus in a Golfer. Orthopedics. 2016;39(5):e997-e1000.
-
11Huang K, Murphy D, Dehghan N. Calcific tendinitis of the gluteus maximus of a 53-year-old woman. CMAJ. 2017;189(50):E1561.
-
12Singh JR, Yip K. Gluteus maximus calcific tendonosis: a rare cause of sciatic pain. Am J Phys Med Rehabil. 2015;94(2):165-7.
-
13Jo H, Kim G, Baek S, Park HW. Calcific Tendinopathy of the Gluteus Medius Mimicking Lumbar Radicular Pain Successfully Treated With Barbotage: A Case Report. Ann Rehabil Med. 2016;40(2):368-72.
-
14Reich MS, Shannon C, Tsai E, Salata MJ. Hip arthroscopy for extra-articular hip disease. Curr Rev Musculoskelet Med. 2013;6(3):250-7.
-
15Hernando MF, Cerezal L, Pérez-Carro L, Abascal F, Canga A. Deep gluteal syndrome: anatomy, imaging, and management of sciatic nerve entrapments in the subgluteal space. Skeletal Radiol. 2015;44(7):919-34.
-
16Carro LP, Hernando MF, Cerezal L, Navarro IS, Fernández AA, Castillo AO. Deep gluteal space problems: piriformis syndrome, ischiofemoral impingement and sciatic nerve release. Muscles Ligaments Tendons J. 2016;6(3):384-396.
-
17Pan J, Bredella MA. Imaging lesions of the lateral hip. Semin Musculoskelet Radiol. 2013;17(3):295-305.
-
18Van Damme K, De Coster L, Mermuys K, Van den Eeckhaut A, Walgraeve N, De Geeter F. Bone scan findings in calcific tendinitis at the gluteus maximus insertion: some illustrative cases. Radiol Case Rep. 2017;12(1):168-74.
-
19Choudur HN, Munk PL. Image-guided corticosteroid injection of calcific tendonitis of gluteus maximus. J Clin Rheumatol. 2006;12(4):176-8.
-
20Oh KJ, Yoon JR, Shin DS, Yang JH. Extracorporeal shock wave therapy for calcific tendinitis at unusual sites around the hip. Orthopedics. 2010;33(10):769.
-
21Baker CL Jr, Mahoney JR. Ultrasound-Guided Percutaneous Tenotomy for Gluteal Tendinopathy. Orthop J Sports Med. 2020;8(3):2325967120907868.
-
22Kandemir U, Bharam S, Philippon MJ, Fu FH. Endoscopic treatment of calcific tendinitis of gluteus medius and minimus. Arthroscopy. 2003;19(1):E4.
-
23Jian C, Dan W, Gangliang W. Endoscopic treatment for calcific tendinitis of the gluteus medius: A case report and review. Front Surg. 2022;9:917027.
-
24Wen Qiang L, Gen Lin F, Chia ZY. A 57-Year-Old Woman with Calcific Tendinitis of the Gluteus Medius Presenting with Right Lateral Hip Pain Managed by Endoscopic Debridement. Am J Case Rep. 2023;24:e938661.
-
25Mitchell JJ, Chahla J, Vap AR, et al. Endoscopic Trochanteric Bursectomy and Iliotibial Band Release for Persistent Trochanteric Bursitis. Arthrosc Tech. 2016;5(5):e1185-e1189.
-
26Randelli F, Pierannunzii L, Banci L, Ragone V, Aliprandi A, Buly R. Heterotopic ossifications after arthroscopic management of femoroacetabular impingement: the role of NSAID prophylaxis. J Orthop Traumatol. 2010;11(4):245-50.
Descargar artículo:
Licencia:
Este contenido es de acceso abierto (Open-Access) y se ha distribuido bajo los términos de la licencia Creative Commons CC BY-NC-ND (Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional) que permite usar, distribuir y reproducir en cualquier medio siempre que se citen a los autores y no se utilice para fines comerciales ni para hacer obras derivadas.
Comparte este contenido
En esta edición
- We are living a golden age in Spanish arthroscopic surgery
- Alteration of the coronal and sagittal axes of the knee and its implication in the failure of anterior cruciate ligament reconstruction. A systematic review
- Arthroscopic acetabular microfractures of the hip: survival and clinical outcome of the technique with a minimum follow-up of 5 years
- Hip arthroscopy provides medical personnel with an early and complete return to work. A multicentre study
- Novel articles on combined ligamentous injury of the anterior cruciate ligament and medial ligament complex of the knee
- Anteroinferior shoulder instability. Essential articles
- Treatment of shoulder instability with bone defects using a combination of arthroscopic bone block and <em>remplissage</em> techniques
- Reconstruction of the rotator cuff using a triple-row arthroscopic technique. Surgical technique
- Endoscopic treatment of calcific tendinitis of the gluteus maximus. A case report
- Incomplete discoid medial meniscus presenting coalescence with the anterior cruciate ligament
Más en PUBMED
Más en Google Scholar
Más en ORCID


Revista Española de Artroscopia y Cirugía Articular está distribuida bajo una licencia de Creative Commons Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional.