Novel articles on combined ligamentous injury of the anterior cruciate ligament and medial ligament complex of the knee
Artículos novedosos sobre lesión ligamentosa combinada del ligamento cruzado anterior y el complejo ligamentoso medial de la rodilla
Resumen:
En este artículo se revisa la literatura reciente sobre el manejo de las lesiones combinadas del ligamento cruzado anterior (LCA) y el ligamento colateral medial (LCM) de la rodilla. El manejo de esta lesión combinada es complejo. Es particularmente importante considerar ambos ligamentos en el tratamiento debido a su interacción biomecánica.
Los estudios revisados han encontrado que la reconstrucción aislada del LCA puede no ser suficiente para restaurar la estabilidad de la rodilla en casos de lesiones combinadas. Ball et al. (2020) demostraron que la laxitud anteromedial puede persistir si no se aborda también el LCM, lo que puede influir en los resultados a largo plazo de la cirugía de LCA.
Además, Svantesson et al. (2019) observaron un aumento en el riesgo de revisión del LCA en pacientes con lesiones combinadas tratadas de forma conservadora en comparación con aquellos sometidos a tratamiento quirúrgico. Este hallazgo subraya la importancia de considerar la reconstrucción simultánea del LCM cuando está comprometido.
El signo del “menisco flotante”, identificado por Funchal et al. (2019), emergió como un marcador significativo para la intervención quirúrgica del LCM en pacientes con lesiones combinadas, sugiriendo que su presencia podría indicar una mayor necesidad de reconstrucción para mejorar los resultados funcionales y reducir la probabilidad de fallo de la plastia del LCA.
En cuanto a la elección del injerto, Figueroa et al. (2020) recomiendan considerar el uso de aloinjertos para el LCM y autoinjertos para el LCA, adaptando la elección según las características individuales del paciente y las demandas funcionales de la rodilla.
Finalmente, Rao et al. (2022) proponen un enfoque terapéutico basado en una revisión sistemática, enfatizando la necesidad de un abordaje individualizado y la importancia de más investigaciones para establecer guías claras en el manejo de estas complejas lesiones.
Estos estudios resaltan la complejidad de las lesiones combinadas del LCA y el LCM, y enfatizan la importancia de un enfoque integral y personalizado para optimizar los resultados clínicos y funcionales en los pacientes afectados.
Abstract:
The present article reviews the recent literature on the management of combined anterior cruciate ligament (ACL) and medial collateral ligament (MCL) injuries of the knee. The management of this combined injury is complex. It is particularly important to consider both ligaments in the approach to treatment because of the biomechanical interaction between them.
The studies reviewed have found that isolated ACL reconstruction may not be sufficient to restore knee stability in cases of combined injuries. Ball et al. (2020) demonstrated that anteromedial laxity may persist if the MCL is not also addressed, which may influence the long-term outcome of ACL surgery.
In addition, Svantesson et al. (2019) observed an increased risk of ACL revision in patients with combined injuries treated conservatively compared to those undergoing surgical treatment. This finding highlights the importance of considering simultaneous reconstruction of the LCM when it is compromised.
The "floating meniscus"sign,identified by Funchal et al. (2019), emerged as a significant marker for MCL surgery in patients with combined injuries, suggesting that its presence may indicate a greater need for reconstruction in order to improve the functional outcomes and reduce the likelihood of ACL plasty failure.
Regarding the choice of graft, Figueroa et al. (2020) recommend considering the use of allografts for the MCL and autografts for the ACL, tailoring the choice according to the individual patient characteristics and the functional demands of the knee.
Finally, Rao et al. (2022) propose a therapeutic strategy based on a systematic review, emphasising the need for an individualised approach and the importance of further research to establish clear guidelines for the management of these complex lesions.
These studies highlight the complexity of combined ACL and MCL injuries, and emphasise the importance of a comprehensive and personalised approach in order to optimise the clinical and functional outcomes in the affected patients.
Introduction
Injuries of the medial collateral ligament (MCL) are the most common ligament injuries of the knee, and are often accompanied by damage to other structures such as the anterior cruciate ligament (ACL), posterior cruciate ligament (PCL), meniscal injuries or injuries of the posteromedial complex (PMC). Among the combined ligament injuries of the knee, the most frequent presentation is the combination of MCL and ACL. In this regard, associated damage of the MCL is found in 20-38% of the cases of ACL injury, resulting in increased knee instability(1).
The MCL consists of two fascicles, a more superficial fascicle (sMCL) and a deeper fascicle (dMCL), forming, together with the medial meniscus, the so-called medial meniscus ligament complex(2). Posterior to the sMCL lies the posterior oblique ligament (POL), which originates directly posterior to the origin of the sMCL and its insertion in three different components: a fascial component, in conjunction with the fibres of the semimembranosus; a capsular component, joining with the posteromedial capsule; and a ligamentous component, joining with the fibres of the sMCL(2).
The function of this medial ligament complex is to oppose valgus movements of the knee and external rotation of the tibia. The most common mechanism of injury is forced valgus, usually accompanied by external rotation and flexion of the knee(3). Injury may be due to direct trauma, in contact sports such as football or rugby, or through indirect twisting and valgus motion on a fixed foot(4).
Combined ACL and MCL injury should be suspected in any patient presenting with joint effusion, ecchymosis on the medial aspect of the knee and restricted mobility, along with exploratory stability test findings compatible with injury to these ligaments, such as the Lachman and pivot shift tests for the ACL, and the forced valgus stress test for the MCL.
After the physical examination, the indicated imaging studies include radiographs (Rx), with stress Rx in some cases, and magnetic resonance imaging (MRI). Once the diagnosis of combined ACL and MCL injury has been made, the most appropriate treatment is decided on an individualised basis.
This article reviews the current literature on multi-ligament knee injuries, focusing on the diagnostic and treatment methodologies for each of the possible clinical scenarios.
S. Ball et al., 2020(5)
In this study, presented in 2020, the authors define the importance and functionality of the intra- and extracapsular ligaments of the knee with respect to the restriction of anteromedial rotation. The biomechanical function of the knee ligaments is schematically detailed according to the movement performed (valgus, varus, rotation, etc.) in different degrees of joint flexion and taking into account the rest of the ligamentous structures that act in harmony.
This is a biomechanical study in which 12 cadaver knees were anchored to a robot that applied different force vectors in an attempt to replicate the tests commonly used in clinical practice to assess knee stability.
To identify the functionality of each ligament, cadaver knees with all the ligaments intact were used, and laxity tests were performed in full extension and flexion of 30º, 60º and90º. They then sequentially sectioned the ACL, sMCL, dMCL, posteromedial capsule and POL, using a different order pattern in each knee, while performing anteroposterior, rotational and varus-valgus stress manoeuvres at 0º, 30º, 60º and90º of flexion, with the aim of determining the degree to which each of these structures contributes to knee stability.
The authors found that the ACL is the single most important restriction to anterior translation, with the sMCL being the second most important element. The most important restrictors for tibial external rotation were the sMCL (when the knee is flexed 90°) and the dMCL (with the knee in extension) - this being the most important finding of the study. The ligamentous structures that most opposed tibial internal rotation between 0º and30º of flexion were the ACL and the POL together with the PMC and the sMCL, while at higher degrees of joint flexion, the greatest restriction to tibial internal rotation was found to be the ACL. The structure with the highest valgus resistance was the sMCL, especially in the first degrees of flexion.
With these results, the authors concluded that in the case of combined ACL and MCL injuries, isolated ACL reconstruction may be insufficient to restore native knee biomechanics, resulting in anteromedialrotatory instability (AMRI), which in turn may worsen both the clinical outcomes and survival of the reconstruction. However, as this was a biomechanical study, it has limitations that make it difficult to extrapolate the results obtained (experimental) to the much more complex reality of clinical practice.
E. Svantesson et al., 2019(6)
In this article published in 2019, a retrospective study was made of all ACL injuries in patients over 15 years of age (mean age: 27.9 years) between 2005 and 2016 from the Swedish national registry (19,457 patients in total). The patients were divided into groups according to whether ACL injury was single or combined (MCL or lateral collateral ligament [LCL]) and, in turn, according to the treatment of the collateral ligament injury (conservative, repair or reconstruction).
It is likely that patients in the combined ACL and MCL injury group would have had better outcomes if MCL repair or reconstruction had been performed in conjunction with ACL plasty. The data indicate that MCL surgery, in addition to ACL reconstruction, significantly improves the outcomes, reducing the risk of ACL revision surgery by 15%. In addition, the surgically treated patients had 20% less residual instability compared to those who underwent conservative MCL treatment.
Patients with isolated ACL injury had better functional test results at two years when compared to patients with combined ACL and MCL injury. Moreover, these differences were greater in those cases where the MCL had been treated surgically, with the poorest scores corresponding to the patients that underwent surgical repair of the MCL. However, no statistically significant differences were found on comparing the MCL reconstruction group with the MCL repair group.
One of the most important limitations of this study is the failure to determine the degree of MCL injury, conditioning the treatment and functional recovery of the patients.
The presence of such a high percentage of patients subjected to conservative MCL treatment and ACL reconstruction, who subsequently required revision surgery, highlights the importance of establishing a correct treatment indication for each patient. It is likely that patients in the combined ACL and MCL injury group would have had better outcomes if MCL repair or reconstruction had been performed in conjunction with ACL plasty. The data indicate that MCL surgery, in addition to ACL reconstruction, significantly improves the outcomes and reduces the risk of postoperative complications.
L.F.Z. Funchal et al., 2019(7)
These authors conducted a clinical trial with a minimum follow-up of two years, involving level of evidence I, and seeking to find differences between patients with combined ACL and MCL grade II injury and the so-called floating meniscus sign.
Injury to the meniscotibial ligament, which is the distal portion of the deep fascicle of the MCL, in some cases is so significant that it causes the mentioned floating meniscus sign. Although the sign can be seen on MRI images, it is much more evident when the medial compartment of the knee is viewed arthroscopically: applying a valgus manoeuvre results in supraphysiological opening of the compartment, so that the entire posterior horn of the internal meniscus, which is usually hidden by the medial condyle, can be visualised. On the other hand, the body of the meniscus "detaches" from the tibial plateau and accompanies the femoral condyle as it separates from the plateau (as the proximal portion of the dMCL is intact).
The patients were divided into two groups: one in which reconstructive treatment of both ligaments (ACL and MCL) was performed, and a second group in which ACL reconstruction and conservative treatment of the MCL was performed. The surgeries were performed 3-6 weeks after the injury.
The study demonstrated that, in patients with the floating meniscus sign, MCL reconstruction surgery resulted in fewer ACL plasty failures, less residual MCL laxity and better Tegner and Lysholm test scores at 24 months of follow-up than with conservative management of the MCL.
This is relevant, since most of the available studies only consider preoperative assessment and diagnostic tests to make the therapeutic decision on the lesion; in contrast, this study shows the importance of intraoperative assessment, which in some cases may change our opinion on the surgical indication for MCL.
F. Figueroa et al., 2020(8)
In this article, Figueroa et al. reviewed the literature to develop a scheme focused on the choice of the best graft in combined ACL and MCL injuries. Because the literature on this topic is very limited, they conducted the search by dividing the clinical scenario into three different questions: 1) What is the best graft in multi-ligament knee injuries?; 2) What is the best graft in MCL injuries?; and 3) What is the best graft in ACL injuries?
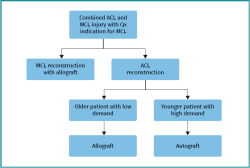
One of the important elements in planning reconstructive surgery for multi-ligament injuries is the choice of grafts to be used. When using an allograft and an autograft, the autograft can come from the ischiotibial area, patellar tendon or quadriceps tendon. If, for whatever reason, the surgeon chooses an ischiotibial autograft, the authors recommend maintaining the integrity of the fascia of the sartorius complex, due to its importance in valgus stability in a knee with a deficient MCL(9) (Figure 1).
Thus, the study suggests that in a combined ACL and MCL injury where reconstruction of both ligaments is necessary, the MCL should be reconstructed with an allograft, while the ACL - depending on patient physical demand - could be reconstructed with an allograft (older patients with low demand) or an autograft (young patients with high demand), preferably avoiding ischiotibial plasty.
This same article cites other studies that stress the importance of the semitendinosus-gracilis-sartorius complex or the importance of maintaining the integrity of the fascia of the sartorius if the decision is made to use this graft for plasty(9). This is a debated issue, and a number of studies suggest that the semimembranosus is the only element that does effectively contribute significantly to stability against forced valgus, which validates the use of ischiotibial grafts to reconstruct the medial side(10).
This study helps to understand the need for preservation of the tendons of the injured knee. However, it would be interesting to carry out a prospective and comparative study evaluating the differences in patients in whom one type of graft or another has been used, depending on the therapeutic scheme presented in the study, and thus see whether it is really effective in the population, which could constitute a new line of research.
R. Rao et al., 2022(11)
These authors conducted a systematic review of 52 articles to determine the differences in carrying out different treatments for combined ACL and MCL injuries. Among the 52 studies analysed, the results were assessed in different ways, the most frequent focus being on stability (anterior and valgus) and function as measured by the Lysholm scale. The systematic review was carried out according to the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guidelines, consulting the PubMed, OVID and Cochrane databases. Two independent reviewers evaluated the articles, including those publications that were original studies reporting clinical outcomes in the treatment of combined ACL and MCL injuries.
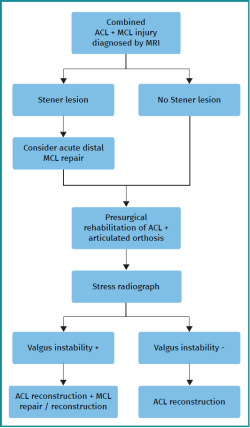
The systematic review defined the need for MCL surgery in those combined ACL and MCL injuries in which a Stener lesion is diagnosed (grade III MCL injury with distal tearing of the ligament and interposition of bony or soft tissue structures between the ligament and itstibialinsertion)(12) or in those patients who, after 6 weeks of rehabilitation with an articulating orthosis, continue to present medial instability confirmed by an increase in the medial opening at stress radiography.
The authors concluded that no clear treatment recommendation for combined ACL and MCL injury can currently be made, since good results have been published with both conservative and surgical (repair and reconstruction) management of the MCL. This lack of consensus encourages the conduction of further studies with a high level of evidence.
Nevertheless, following their systematic review, the authors proposed a therapeutic algorithm (Figure 2), which is the one they themselves use.
Conclusions
The surgical management of combined ACL and MCL injuries constitutes a significant challenge, due to their complexity. The decision between treating the MCL conservatively or surgically directly impacts upon the outcome of ACL reconstruction. The reviewed studies indicate that MCL surgery reduces the risk of ACL revision compared to conservative treatment, which involves a greater risk of complications. In addition, consideration should focus on the choice of graft, as well as on the management of anteromedial laxity, in order to optimise the surgical and functional outcomes.
In conclusion, an appropriate surgical strategy involving MCL repair or reconstruction can significantly improve the outcomes in patients with combined ACL and MCL injuries, thereby reducing the need for revision surgery and improving long-term knee stability. This suggests the importance of a personalised and meticulous approach to the management of these complex lesions.
Figuras
Figure 1. Schematic representation of the choice of graft according to Figueroa et al(8). ACL: anterior cruciate ligament; MCL: medial collateral ligament; Qx: surgery.
Información del artículo
Cita bibliográfica
Autores
Antonio Luis García Cebrián
Hospital Universitario de Igualada. Barcelona
Sergi Gil González
Unidad de Rodilla. Hospital Universitari Parc Taulí. Sabadell, Barcelona
Unidad de Pie y Tobillo. Parc de Salut Mar. Hospital de l’Esperança. Barcelona
Hospital Universitario de Igualada. Consorci Sanitari de l'Anoia
Ricardo Andrés Barja
Unidad de Rodilla. Hospital Universitari d'Igualada. Barcelona
Ethical responsibilities
Conflicts of interest. The authors state that they have no conflicts of interest.
Financial support. This study has received no financial support.
Protection of people and animals. The authors declare that this research has not involved human or animal experimentation.
Data confidentiality. The authors declare that the protocols of their work centre referred to the publication of patient information have been followed.
Right to privacy and informed consent. The authors declare that no patient data appear in this article.
Referencias bibliográficas
-
1Majewski M, Susanne H, Klaus S. Epidemiology of athletic knee injuries: a 10-year study. Knee. 2006;13:184-8.
-
2LaPrade RF, Engebretsen AH, Ly TV, Johansen S, Wentorf FA, Engebretsen L. The anatomy of the medial part of the knee. J Bone Joint Surg Am. 2007;89(9):2000-10.
-
3Phisitkul P, James SL, Wolf BR, Amendola A. MCL injuries of the knee: current concepts review. Iowa Orthop J. 2006;26:77-90.
-
4Bollier M, Smith PA. Anterior Cruciate Ligament and Medial Collateral Ligament Injuries. J Knee Surg. 2014;27(5):359-68.
-
5Ball S, Stephen JM, El-Daou H, Williams A, Amis AA. The medial ligaments and the ACL restrain anteromedial laxity of the knee. Knee Surg Sports Traumatol Arthrosc. 2020;28(12):3700-8.
-
6Svantesson E, HamrinSenorski E, Alentorn-Geli E, et al. Increased risk of ACL revision with non-surgical treatment of a concomitant medial collateral ligament injury: a study on 19,457 patients from the Swedish National Knee Ligament Registry. Knee Surg Sports Traumatol Arthrosc. 2019;27(8):2450-9.
-
7Funchal LFZ, Astur DC, Ortiz R, Cohen M. The Presence of the Arthroscopic “Floating Meniscus” Sign as an Indicator for Surgical Intervention in Patients With Combined Anterior Cruciate Ligament and Grade II Medial Collateral Ligament Injury. Arthroscopy. 2019;35(3):930-7.
-
8Figueroa F, Figueroa D, Calvo R, Vaisman A, Espregueira-Mendes J. Graft choice in combined anterior cruciate ligament and medial collateral ligament reconstruction. EFORT Open Rev. 2020;5(4):221-5.
-
9Kremen TJ, Polakof LS, Rajaee SS, Nelson TJ, Metzger MF. The Effect of Hamstring Tendon Autograft Harvest on the Restoration of Knee Stability in the Setting of Concurrent Anterior Cruciate Ligament and Medial Collateral Ligament Injuries. Am J Sports Med. 2018;46(1):163-70.
-
10Svantesson E, Hamrin Senorski E, Östergaard M, et al. Graft Choice for Anterior Cruciate Ligament Reconstruction With a Concomitant Non-surgically Treated Medial Collateral Ligament Injury Does Not Influence the Risk of Revision. Arthroscopy. 2020;36(1):199-211.
-
11Rao R, Bhattacharyya R, Andrews B, Varma R, Chen A. The management of combined ACL and MCL injuries: A systematic review. J Orthop. 2022;34:21-30.
-
12Denisov D, Chen DS, Motamedi D. Stener-like lesion of the medial collateral ligament of the knee. Radiol Case Rep. 2023;18(3):913-6.
Descargar artículo:
Licencia:
Este contenido es de acceso abierto (Open-Access) y se ha distribuido bajo los términos de la licencia Creative Commons CC BY-NC-ND (Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional) que permite usar, distribuir y reproducir en cualquier medio siempre que se citen a los autores y no se utilice para fines comerciales ni para hacer obras derivadas.
Comparte este contenido
En esta edición
- We are living a golden age in Spanish arthroscopic surgery
- Alteration of the coronal and sagittal axes of the knee and its implication in the failure of anterior cruciate ligament reconstruction. A systematic review
- Arthroscopic acetabular microfractures of the hip: survival and clinical outcome of the technique with a minimum follow-up of 5 years
- Hip arthroscopy provides medical personnel with an early and complete return to work. A multicentre study
- Novel articles on combined ligamentous injury of the anterior cruciate ligament and medial ligament complex of the knee
- Anteroinferior shoulder instability. Essential articles
- Treatment of shoulder instability with bone defects using a combination of arthroscopic bone block and <em>remplissage</em> techniques
- Reconstruction of the rotator cuff using a triple-row arthroscopic technique. Surgical technique
- Endoscopic treatment of calcific tendinitis of the gluteus maximus. A case report
- Incomplete discoid medial meniscus presenting coalescence with the anterior cruciate ligament
Más en PUBMED
Más en Google Scholar


Revista Española de Artroscopia y Cirugía Articular está distribuida bajo una licencia de Creative Commons Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional.