Arthroscopic ligamentoplasty for lateral ankle instability
Ligamentoplastia artroscópica para la inestabilidad lateral de tobillo
Resumen:
El esguince de tobillo constituye aproximadamente el 25% de todas las lesiones agudas del aparato locomotor, destacando la afectación frecuente de los ligamentos talofibular anterior (LTFA) y calcaneofibular (LCF). Alrededor del 20% desarrolla inestabilidad crónica, requiriendo en ocasiones intervención quirúrgica.
El objetivo de este artículo es la descripción de la ligamentoplastia artroscópica para el tratamiento de la inestabilidad crónica lateral de tobillo.
Las indicaciones para la ligamentoplastia artroscópica incluyen inestabilidad persistente después de 6 meses y tras 10-12 semanas de recuperación funcional intensiva. La técnica implica la preparación de la plastia, seguida de la creación de túneles en el peroné, el astrágalo y el calcáneo para la fijación de la plastia.
La elección entre reparación directa y ligamentoplastia depende de factores como la duración de la lesión, la calidad del tejido remanente y la presencia de inestabilidad subtalar. Aunque la falta de estudios comparativos complica la elección entre técnicas, la ligamentoplastia puede ser beneficiosa en pacientes con lesiones crónicas, con escaso tejido remanente y lesiones concomitantes articulares.
A pesar de la falta de estudios prospectivos comparativos, la ligamentoplastia artroscópica se considera segura, con bajo riesgo de complicaciones. La técnica, aunque demandante, destaca por su utilidad en pacientes con inestabilidad crónica refractaria al tratamiento conservador, proporcionando una opción quirúrgica efectiva para mejorar la estabilidad del tobillo.
Abstract:
Ankle sprains account for approximately 25% of all acute musculoskeletal injuries, with frequent involvement of the anterior talofibular ligament (ATFL) and calcaneofibular ligament (CFL). Approximately 20% develop chronic instability, sometimes requiring surgical treatment.
The aim of this article is to describe arthroscopic ligamentoplasty for the treatment of chronic lateral ankle instability.
The indications for arthroscopic ligamentoplasty include persistent instability after 6 months and after 10-12 weeks of intensive functional recovery. The technique involves preparation of the plasty, followed by the creation of tunnels in the fibula, talus and calcaneus for fixation of the plasty.
The choice between direct repair and ligamentoplasty depends on factors such as the duration of the injury, the quality of the remaining tissue and the presence of subtalar instability. Although the lack of comparative studies complicates the choice between techniques, ligamentoplasty may be beneficial in patients with chronic injuries, with little remaining tissue, and with concomitant joint injuries.
Despite the lack of prospective comparative studies, arthroscopic ligamentoplasty is considered to be safe, with a low risk of complications. The technique, although demanding, is particularly useful in patients with chronic instability refractory to conservative management, affording an effective surgical option for improving ankle stability.
Introduction
Ankle sprains are the most common locomotor injury, accounting for 25% of all acute injuries(1). One of the possible consequences is ligament rupture, with the anterior talofibular ligament (ATFL) and calcaneofibular ligament (CFL) being the most frequently affected ligaments. Although most patients present a good clinical course with conservative management, up to 46% eventually develop chronic post-traumatic ankle instability, and surgical treatment is necessary in these cases(2,3).
Multiple surgical techniques have been described in patients suffering chronic instability, with direct repair or anatomical reconstruction techniques being the procedures of choice, either via open surgery or through minimally invasive techniques(4). In relation to the minimally invasive techniques, arthroscopy has gained popularity in recent years, mainly in the form of arthroscopic direct repair or reinsertion, known as the all-inside technique(5). Despite the good results reported with this technique, there is recently increasing interest in arthroscopic ligamentoplasty using allografts or autologous grafts, which may offer advantages in selected patients(5,6,7).
The present study describes the indications and surgical technique for arthroscopic ligamentoplasty of the ATFL and LCF in patients with chronic ankle instability.
Indications
Arthroscopic ligamentoplasty of the ATFL and CFL is indicated in patients with ankle instability, defined as persistent pain, repetitive failure or subjective failure sensation 6 months after the sprain episode and always after 10-12 weeks of intensive functional recovery(8). This is a fundamentally clinical diagnosis, as complementary tests, mainly radiography, ultrasound and magnetic resonance imaging (MRI) may prove negative or inconclusive, without ruling out chronic ankle instability(9). It is necessary to support the clinical diagnosis of this disorder not only by physical examination, but also by a detailed case history of the patient. Validated questionnaires are thus available for the diagnosis(10).
In patients with chronic ankle instability, we find no evidence of superiority of ligamentoplasty over direct repair. Despite this, a prolonged evolution time, poor quality of the remaining tissue, damage to both fascicles (ATFL + CFL), non-insertional or distal injury to the ATFL, or the presence of subtalar instability, may cause us to favor ligamentoplasty(11,12).
Surgical technique
Instruments and requirements
For arthroscopic ligamentoplasty of the ATFL and CFL, an arthroscopy tower, a water pump allowing work low pressures (20 mmHg) and 30° × 4 mm arthroscopic optics are required. In relation to the implants, an adjustable suture button system is needed for fixation of the plasty at fibular level, along with tenodesis implants 4-5 mm in diameter × 20 mm in length for fixation of the plasty in the blind talar and calcaneal tunnel.
Surgical technique
Ligamentoplasty is performed under intrathecal regional anesthesia and sedation with the ischemia cuff on the thigh. The patient is placed in the supine position with the aid of a gynecology leg support on which the limb to be operated upon will rest. In some cases it is necessary to place a support to raise the ipsilateral hip and reduce physiological external rotation (Figure 1). This position allows us to manage dorsal and plantar flexion of the ankle on demand during the surgical procedure. Traction systems are not necessary.
After draping and asepsis of the patient, we mark the anatomical landmarks (Figure 2), the most important being the anterior tibial tendon, the medial and lateral malleolus, the peroneus tertius muscle, the joint line and the superficial branch of the peroneal nerve - injury to the latter being one of the main risks when performing this procedure.
reacae.31282.fs2402008en-figure2.png
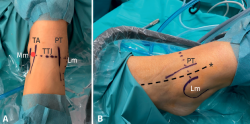
Figure 2. Portal references. A: anterior view. The tibialis anterior (TA), peroneus tertius (PT) are referenced and the tibiotalar joint line (TTJ) is drawn. We also mark the medial (Mm) and lateral malleolus (Lm); B: lateral view. The trajectory of the superficial peroneal nerve (*) between Lm and PT is referenced.
The procedure starts with the conventional anteromedial (AM) portal described by Van Dijk(13). For this purpose, a skin incision is made over the tibialis anterior or slightly medial to the tibialis anterior, and then, in maximum dorsal flexion, a mosquito clamp is introduced intra-articular and medial to the tendon. It is important to work in dorsal flexion when performing the arthroscopic portals and on inserting or exchanging instruments, in order to protect the talar dome and thus avoid iatrogenic chondral injuries during the procedure.
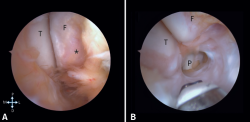
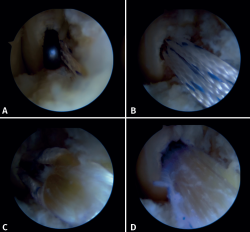
Once the AM portal has been established, we open the water pump, always working with pressures around 20 mmHg, and perform a complete arthroscopic assessment. To assess the lesion of the external lateral complex, through the AM portal, we follow the joint line to the lateral groove. In this regard, the anteroinferior tibiofibular ligament can be used as a reference, since the distal insertion of this ligament at the level of the fibula is the origin of the ATFL (Figure 3).
In cases of injury to the ATFL, we will observe a denudation or absence of the ATFL, known as a footprint, at this level on the anterior aspect of the fibula (Figure 3A). If, in addition to the ATFL, there is damage to the CFL, we can access the posterior compartment of the ankle with the optics and even see the peroneal tendons from the AM portal (Figure 3B).
Once the injury has been verified, we proceed to perform the ligamentoplasty.
Plasty preparation
Ligamentoplasty can be performed with autologous graft or allograft. When using autologous grafts, for size, length and morbidity reasons, we advise use of the palmaris longus tendon, although as a drawback this involves the need for two surgical fields. Other allograft options are gracilis tendon (it will have to be worked on to adapt it to the patient's needs) or the extensor digiti minimi. The latter may cause technical difficulties due to the length and diameter of the graft. In the case of an allograft, use of the flexor carpi radialis tendon is a good option, due to its characteristics in terms of length and thickness. Other options, such as the peroneal tendon may be useful, but will require preparation for our needs. In our case, we prefer to use the flexor carpi radialis tendon.
The graft is placed in 0.9% physiological saline solution (PSS) with vancomycin(14), after which the measurements will be made on it. To do this, we pass a loop suture through one of the ends and make the following consecutive marks on it, as shown in Figure 4:
- 20 mm (talar insertion = size of the implant of the blind talar tunnel).
- 15 mm (intra-articular segment of the graft).
- 15 mm (ascending segment of the fibular tunnel).
- 15 mm (descending segment of the fibular tunnel).
- Remainder plasty for insertion into the calcaneal tunnel.
We pass a second suture through the distal end of the plasty, which will later be used to recover the plasty through the distal calcaneal portal.
reacae.31282.fs2402008en-figure4.png
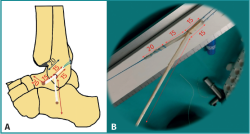
Figure 4. A: referenced drawing of the placement and measurement of the ankle plasty. Note the 15 mm loop in and out of the fibula, the 15 mm to the talus, and the 20 mm of plasty inserted in the talar tunnel. On the other side of the loop, we see the trajectory to the calcaneus and the tunnel; B: image of the preparation of the plasty. Note the 15 mm loop there and back at the calcaneus, the 15 mm trajectory to the talus and 20 mm of the tunnel. Towards the opposite side, the plasty we will use for the trajectory in calcaneofibular reconstruction.
Finally, we measure the loop or double plasty, this being the measurement of the tunnel that we will make at fibular level. It is recommended that it should be less than or equal to 5.5 mm in diameter.
Tunnelling and passing of the plasty
If necessary, a previous tibiotalar synovectomy will be made to prepare the surgical field. It is important not to be too aggressive with the arthroscopic synovectomy, as iatrogenic capsule rupture can cause us to lose our working compartment and thus make it difficult to perform the procedure.
Accessory anterolateral portal
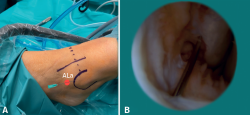
Once the AM portal described above has been prepared and the lesion has been checked, an accessory anterolateral portal (ALa) is made using an intramuscular guide needle with the desired orientation for preparing the fibular tunnel (Figure 5). This portal is usually located about 1.5 mm anterior and distal to the lateral malleolus. A conventional anterolateral (AL) portal is not necessary unless we want to perform some procedure combined with the ligamentoplasty, such as repair of an osteochondral lesion or reattachment of the deltoid ligament.
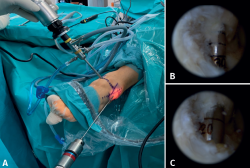
First, we prepare the fibular tunnel (Figure 6). Taking the footprint on the anterior surface of the fibula as a reference, a complete tunnel is made using the Kirschner wire (KW) with an eyelet, from medial to lateral, at about30° of inclination with respect to the horizontal plane formed by the sole of the foot with the ankle at0° and forcing a direction from medial to lateral to avoid the peroneal muscles. The diameter of the KW and of this complete tunnel is usually around 4.5 mm, but this will depend on the type of implant or suture button used. It is important at this point to make a small incision on the posterior surface of the fibula, in order to reflect the peroneal tendons from lateral to medial with a retractor, and thus protect them from possible injury on penetrating the posterior cortex with the wire (Figure 7). Then, we create the blind fibular tunnel over this first tunnel, the diameter of which will depend on the diameter of the double plasty (it should not to exceed 5.5 mm in diameter). In relation to the blind fibular tunnel, we create a tunnel 18-20 mm in depth. Bearing in mind that we will introduce 15 mm of plasty into the fibular tunnel, since we insert the 30 mm plasty folded in half, these extra 3-4 mm of drilling will allow us to tighten the plasty with the suture button system at the end of the procedure, if necessary. Finally, we pass a needleless suture through the fibular tunnel, which will be used later to ascend the plasty through the tunnel. Then, once the fibular tunnel has been made, a blind talar tunnel measuring 20 mm (implant length) × 5.5 mm is made through the ALa portal (Figure 8). This tunnel is located at the insertion of the ATFL. The point is found in the center of the craniocaudad axis of the lateral surface of the talus at the level of the start of the talar neck as an anatomical reference. Drilling is directed towards the tip of the internal malleolus, avoiding moving towards the articular surface of the talus.
Finally, with the help of a suture passer or mosquito clamp, we insert a needleless suture from the ALa portal. We advance this suture from proximal to distal along the lateral surface of the calcaneus, always deep to the peroneal tendons, until we reach the subcutaneous level at the calcaneal insertion of the CFL. This point is located 1 cm posterior and 1 cm inferior to the tip of the peroneal malleolus, so with the mosquito clamp we can subcutaneously palpate that we are in the correct position. It is at this point where we will make an incision to subsequently recover the plasty at this level and create the calcaneal tunnel under direct vision.
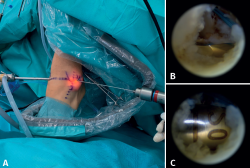
Fixing the plasty (Figures 9 and 10)
Once the fibular and talar tunnels have been made, the plasty is fixed with the suture button system at fibular level and a tenodesis implant in the 20 × 5.5 mm blind tunnel at talar level. It is important to insert the plasty 15 mm into the fibular tunnel, leaving a remaining 3-5 mm of tunnel to allow final tightening if necessary, as explained above. This will leave the extremity of the CFL free through our working portal or ALa. With the help of the suture that we have previously passed deep to the peroneal tendons, we retrieve the end of the plasty corresponding to the CFL through the distal incision. We discard the excess plasty calculating 15 mm of plasty from the skin. The distal end is prepared with a loop suture, the 20 × 5 mm blind calcaneal tunnel is made, and the plasty is fixed with a tenodesis implant like that used for fixation of the plasty in the talus. The plasty is fixed in neutral ankle flexion (Figure 11).
Postoperative management
Weight bearing is avoided with a Walker type orthopedic boot for 14 days. Subsequently, with this boot, full weight bearing is allowed and the intensive functional recovery process begins, protecting inversion and forced eversion movements. During this period, we allow active ankle extension and flexion according to tolerance. At four weeks (6 weeks after the procedure), the orthopedic boot is completely removed and intensive functional recovery continues, in this case, allowing free mobility.
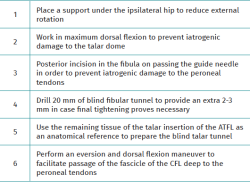
Although technically demanding, arthroscopic ligamentoplasty is a safe technique, with a low complications rate. Table 1 offers advice and recommendations for performing the plasty.
Discussion
The choice of surgical technique for the treatment of chronic ankle instability is still a controversial issue. We continue to debate whether it is better to perform repair or reconstruction techniques and whether these should be done arthroscopically or through open surgery.
reacae.31282.fs2402008en-figure10.png
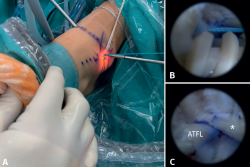
Figure 10. A: external view of insertion of the implant at talar level through the accessory anterolateral portal; B: arthroscopic view of insertion of the implant in the blind talar tunnel; C: arthroscopic view of the anterior talofibular ligament (ATFL) and the fascicle that we will use for the calcaneofibular ligament (CFL) (*).
Among the techniques reported in the literature, arthroscopic ligamentoplasty described by Guillo is an anatomical reconstruction technique indicated in patients with chronic ankle instability refractory to conservative treatment(15). In this regard, the superiority of anatomical techniques over non-anatomical techniques has been described in the literature, offering better outcomes in terms of patient satisfaction, joint stiffness and the incidence of complications, but the published studies lack sufficient quality(16,17,18,19).
reacae.31282.fs2402008en-figure11.png
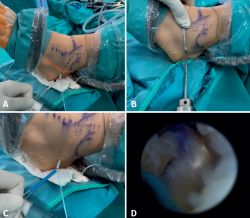
Figure 11. A: view of passage of the plasty under the peroneal tendons and retrieval of the plasty for its tunnel in the calcaneus; B: preparation of the calcaneal tunnel through the same incision for retrieval of the plasty; C: preparation of the plasty for insertion into the calcaneal tunnel; D: arthroscopic view through the anteromedial portal of the ATFL and CFL.
Arthroscopic techniques offer advantages over open repair procedures, such as the treatment of concomitant injuries in the same surgical procedure(20,21).
In this regard, Matsui reported better results with arthroscopic treatment during the first postoperative year, including superior postoperative pain management and a shorter recovery time(22). Subsequently, following a systematic review, the same author concluded that there is insufficient evidence to recommend one technique over the other, due to the lack of quality prospective studies comparing open versus arthroscopic techniques(23).
Despite the lack of evidence, arthroscopic ligamentoplasty may offer advantages over other surgical techniques. Firstly, arthroscopic techniques allow us to treat injuries associated with chronic instability, such as osteochondral lesions, which are present in 38.7% of the patients(24). Furthermore, the simultaneous treatment of osteochondral lesions in patients with chronic instability does not influence the outcome of instability treatment. What has been observed is that patients with osteochondral lesions and ankle instability have poorer outcomes than patients without cartilage lesions.
Some publications suggest that the reconstruction of both ligaments (ATFL and CFL) may offer advantages over repair. An example is the treatment of subtalar instability, which is common in patients diagnosed with chronic instability and damage to both fascicles(24,25). In addition, poorer outcomes in terms of talar tilt have been reported one year after surgery in patients without CFL repair, although these results did not have a clinical impact(26). This can be explained thanks to the study by Fernández-Marin et al., who described an increase in subtalar joint rotation in patients with tibiotalar instability(27). On the other hand, the use of grafting in ligamentoplasty allows the treatment of patients with long-standing injuries and little remaining tissue, or patients with injury to the ATFL at its talar insertion(28).
Regarding the use of autologous graft or allograft, we propose a technique using allograft, since it reduces surgery time, avoiding morbidity or complications in the donor zone. In this regard, Xu et al. found no statistically significant differences compared to autologous grafting in terms of clinical outcome, talar tilt and talar shift at 12 months(29). However, more long-term studies are needed to assess possible differences, such as re-rupture risk, infection rate and the recurrence of instability, in addition to cost-effectiveness studies.
The use of one technique or other must also consider the potential complications in each case. The most common arthroscopic repairs are third peroneal and extensor entrapment, and superficial peroneal nerve injuries.
On analyzing the technique described in the study, it is essential to assess how the distance of the ALa portal may influence the incidence of these complications. In reviewing the literature, we found no references to complications and their incidence in this specific technique. It therefore would be of great interest to carry out a study to investigate this hypothesis and thus contribute to knowledge on the prevention of such complications.
Conclusions
In conclusion, and following the review made, arthroscopic ligamentoplasty makes it possible to treat patients independently of the remaining ligament tissue, widening the group of patients who can benefit from this technique. It also allows us to treat concomitant ankle injuries in the same surgical procedure.
Knowing this, and considering that there is no quality evidence to recommend one technique over the other, we recommend the arthroscopic reconstruction technique because of the advantages it offers over open repair and non-anatomical reconstruction techniques.
Nevertheless, quality prospective studies are needed in order to shed light on the choice of one technique or the other.
Figuras
Figure 1. Positioning of the patient. A: lateral view; *: gynecology leg support; arrow: ipsilateral hip support to reduce external rotation; B: anterior view of leg positioning in the gynecology leg support.
Figure 2. Portal references. A: anterior view. The tibialis anterior (TA), peroneus tertius (PT) are referenced and the tibiotalar joint line (TTJ) is drawn. We also mark the medial (Mm) and lateral malleolus (Lm); B: lateral view. The trajectory of the superficial peroneal nerve (*) between Lm and PT is referenced.
Figure 3. Arthroscopic camera view through the medial portal. A: the lateral groove between the talus (T) and the fibula (F) is observed. We can see the denuded footprint of the ATFL (*); B: the tibia and fibula can be seen, and the peroneus longus (P) is marked at the bottom of the image.
Figure 4. A: referenced drawing of the placement and measurement of the ankle plasty. Note the 15 mm loop in and out of the fibula, the 15 mm to the talus, and the 20 mm of plasty inserted in the talar tunnel. On the other side of the loop, we see the trajectory to the calcaneus and the tunnel; B: image of the preparation of the plasty. Note the 15 mm loop there and back at the calcaneus, the 15 mm trajectory to the talus and 20 mm of the tunnel. Towards the opposite side, the plasty we will use for the trajectory in calcaneofibular reconstruction.
Figure 5. A: note the accessory anterolateral portal (ALa) through which a guide needle is introduced to ensure good orientation; B: arthroscopic view through the anteromedial portal where we can see the needle of the accessory anterolateral portal.
Figure 6. A: anterior view of the use of the instruments. Insertion of the drill through the accessory anterolateral portal (ALa); B: arthroscopic view of the drill at fibular level; C: drilling up to 20 mm for insertion of the plasty loop at fibular level.
Figure 8. A: view of instrument arrangement for the talar tunnel; B: arthroscopic view of the drill at talar level; C: image of drilling up to 20 mm, which is the length of the plasty that will go into the tunnel.
Figure 9. A: anteromedial (AM) arthroscopic view of introduction of the suture button through the fibular tunnel; B: same view with introduction of the suture through the fibular tunnel; C: arrival of the fibular loop in its tunnel; D: the loop is advanced up to the 15 mm mark.
Figure 10. A: external view of insertion of the implant at talar level through the accessory anterolateral portal; B: arthroscopic view of insertion of the implant in the blind talar tunnel; C: arthroscopic view of the anterior talofibular ligament (ATFL) and the fascicle that we will use for the calcaneofibular ligament (CFL) (*).
Figure 11. A: view of passage of the plasty under the peroneal tendons and retrieval of the plasty for its tunnel in the calcaneus; B: preparation of the calcaneal tunnel through the same incision for retrieval of the plasty; C: preparation of the plasty for insertion into the calcaneal tunnel; D: arthroscopic view through the anteromedial portal of the ATFL and CFL.
Tablas
Información del artículo
Cita bibliográfica
Autores
David Campillo Recio
Editor invitado de REACA
Institut Català de Traumatologia i Medicina de l’Esport.
Hospital Universitari Dexeus. Barcelona
ICATME. Hospital Universitari Quirón Dexeus. Barcelona
Juan Antonio Calle García
ICATME. Hospital Universitari Quirón Dexeus. Barcelona
Glòria Albertí Fitó
ICATME. Hospital Universitari Quirón Dexeus. Barcelona
Servicio de Cirugía Ortopédica y Traumatología. Hospital Universitari Germans Trias i Pujol. Badalona, Barcelona
Servicio de Cirugía Ortopédica y Traumatología. Hospital Universitario Quirón Dexeus. Barcelona
Jesús Vilá y Rico
Servicio de Cirugía Ortopédica y Traumatología. Hospital Universitario 12 de Octubre. Madrid
Departamento de Cirugía. Universidad Complutense de Madrid. Madrid
Complejo Hospitalario Quirón Ruber. Madrid
Presidente saliente de la Revista del Pie y Tobillo
Ethical responsibilities
Conflicts of interest. The authors state that they have no conflicts of interest.
Financial support. This study has received no financial support.
Protection of people and animals. The authors declare that this research has not involved human or animal experimentation.
Data confidentiality. The authors declare that the protocols of their work centre referred to the publication of patient information have been followed.
Right to privacy and informed consent. The authors declare that no patient data appear in this article.
Referencias bibliográficas
-
1Ekstrand J, Tropp H. The incidence of ankle sprains in soccer. Foot Ankle. 1990;11(1):41-4.
-
2De Vries JS, Krips R, Sierevelt IN, Blankevoort L, van Dijk CN. Interventions for treating chronic ankle instability. Cochrane Database Syst Rev. 2011;(8):CD004124.
-
3Lin CI, Houtenbos S, Lu YH, Mayer F, Wippert PM. The epidemiology of chronic ankle instability with perceived ankle instability- a systematic review. J Foot Ankle Res. 2021;14(1):41.
-
4Messer TM, Cummins CA, Ahn J, Kelikian AS. Outcome of the modified Broström procedure for chronic lateral ankle instability using suture anchors. Foot Ankle Int. 2000;21(12):996-1003.
-
5Guillo S, Odagiri H, van Rooij F, Bauer T, Hardy A. All-inside endoscopic anatomic reconstruction leads to satisfactory functional outcomes in patients with chronic ankle instability. Knee Surg Sports Traumatol Arthrosc. 2021;29(4):1318-24.
-
6Wang W, Xu GH. Allograft tendon reconstruction of the anterior talofibular ligament and calcaneofibular Ligament in the treatment of chronic ankle instability. BMC Musculoskelet Disord. 2017;18(1):150.
-
7Lui TH. Arthroscopic-assisted lateral ligamentous reconstruction in combined ankle and subtalar instability. Arthroscopy. 2007;23(5):554.e1-5.
-
8Aicale R, Maffulli N. Chronic Lateral Ankle Instability: Topical Review. Foot Ankle Int. 2020;41(12):1571-81.
-
9Salat P, Le V, Veljkovic A, Cresswell ME. Imaging in Foot and Ankle Instability. Foot Ankle Clin. 2018;23(4):499-522.e28.
-
10Ginés-Cespedosa A, Edo Llobet M, López Hernández G, Tejero S. Protocolo de inestabilidad crónica de tobillo de la SEMCPT. Rev Pie Tobillo. 2020;34(1). Disponible en: http://dx.doi.org/10.24129/j.rpt.3401.fs2003007.
-
11Song Y, Li H, Sun C, et al.; Chinese Society of Sports Medicine. Clinical Guidelines for the Surgical Management of Chronic Lateral Ankle Instability: A Consensus Reached by Systematic Review of the Available Data. Orthop J Sports Med. 2019;7(9):2325967119873852.
-
12De Vries JS, Krips R, Sierevelt IN, Blankevoort L, van Dijk CN. Interventions for treating chronic ankle instability. Cochrane Database Syst Rev. 2011;(8):CD004124.
-
13De Leeuw PAJ, van Sterkenburg MN, van Dijk CN. Arthroscopy and endoscopy of the ankle and hindfoot. Sports Med Arthrosc Rev. 2009;17(3):175-84.
-
14Xiao M, Sherman SL, Safran MR, Abrams GD. Significantly Lower Infection Risk for Anterior Cruciate Ligament Grafts Presoaked in Vancomycin Compared With Unsoaked Grafts: A Systematic Review and Meta-analysis. Arthroscopy. 2021;37(5):1683-90.
-
15Guillo S, Archbold P, Perera A, Bauer T, Sonnery-Cottet B. Arthroscopic anatomic reconstruction of the lateral ligaments of the ankle with gracilis autograft. Arthrosc Tech. 2014;3(5):e593-8.
-
16Sammarco VJ. Complications of lateral ankle ligament reconstruction. Clin Orthop. 2001;(391):123-32.
-
17Karlsson J, Bergsten T, Lansinger O, Peterson L. Lateral instability of the ankle treated by the Evans procedure. A long-term clinical and radiological follow-up. J Bone Joint Surg Br. 1988;70(3):476-80.
-
18Hennrikus WL, Mapes RC, Lyons PM, Lapoint JM. Outcomes of the Chrisman-Snook and modified-Broström procedures for chronic lateral ankle instability. A prospective, randomized comparison. Am J Sports Med. 1996;24(4):400-4.
-
19Van der Rijt AJ, Evans GA. The long-term results of Watson-Jones tenodesis. J Bone Joint Surg Br. 1984;66(3):371-5.
-
20Gregush RV, Ferkel RD. Treatment of the unstable ankle with an osteochondral lesion: results and long-term follow-up. Am J Sports Med. 2010;38(4):782-90.
-
21Li H, Hua Y, Ma K, Li S, Chen S. Activity level and function 2 years after anterior talofibular ligament repair: a comparison between arthroscopic repair and open repair procedures. Am J Sports Med. 2017;45(9):2044-51.
-
22Matsui K, Takao M, Miyamoto W, Matsushita T. Early recovery after arthroscopic repair compared to open repair of the anterior talofibular ligament for lateral instability of the ankle. Arch Orthop Trauma Surg. 2016;136(1):93-100.
-
23Matsui K, Burgesson B, Takao M, et al. Minimally invasive surgical treatment for chronic ankle instability: a systematic review. Knee Surg Sports Traumatol Arthrosc. 2016;24(4):1040-8.
-
24Kim YS, Kim TY, Koh YG. Demographic Predictors of Concomitant Osteochondral Lesion of the Talus in Patients With Chronic Lateral Ankle Instability. Foot Ankle Orthop. 2021;6(2):24730114211013344.
-
25Hanada M, Hotta K, Matsuyama Y. Comparison Between the Simultaneous Reconstructions of the Anterior Talofibular Ligament and Calcaneofibular Ligament and the Single Reconstruction of the Anterior Talofibular Ligament for the Treatment of Chronic Lateral Ankle Instability. J Foot Ankle Surg. 2022;61(3):533-6.
-
26Maffulli N, Del Buono A, Maffulli GD, et al. Isolated anterior talofibular ligament Broström repair for chronic lateral ankle instability: 9-year follow-up. Am J Sports Med. 2013;41(4):858-64.
-
27Fernández-Marín MR, González-Martín D, Herrera-Pérez M, Paulano-Godino F, Vilá-Rico J, Tejero S. Increased subtalar rotational motion in patients with symptomatic ankle instability under load and stress conditions. Knee Surg Sports Traumatol Arthrosc. 2023;31(11):5214-21.
-
28Choi HJ, Kim DW, Park JS. Modified Broström Procedure Using Distal Fibular Periosteal Flap Augmentation vs Anatomic Reconstruction Using a Free Tendon Allograft in Patients Who Are Not Candidates for Standard Repair. Foot Ankle Int. 2017;38(11):1207-14.
-
29Xu X, Hu M, Liu J, Zhu Y, Wang B. Minimally invasive reconstruction of the lateral ankle ligaments using semitendinosus autograft or tendon allograft. Foot Ankle Int. 2014;35(10):1015-21.
Descargar artículo:
Licencia:
Este contenido es de acceso abierto (Open-Access) y se ha distribuido bajo los términos de la licencia Creative Commons CC BY-NC-ND (Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional) que permite usar, distribuir y reproducir en cualquier medio siempre que se citen a los autores y no se utilice para fines comerciales ni para hacer obras derivadas.
Comparte este contenido
En esta edición
- Learning from the best
- Everyone's effort
- Inclusion of the long portion of the biceps in rotator cuff repairs
- Surgical technique of the arthroscopic Latarjet procedure with button fixation
- Arthroscopic lateral collateral ligament plication of the elbow
- Arthroscopy-assisted treatment of metacarpophalangeal joint fractures of the fingers
- Surgical technique of hip arthroscopy without perineal post
- Direct reattachment in anterior cruciate ligament ruptures
- Application of fresh osteochondral allografts to the patella. Surgical procedure
- Arthroscopic ligamentoplasty for lateral ankle instability
- Two handles to grasp: double bucket-handle meniscal lesion
Más en PUBMED
Más en Google Scholar
Más en ORCID


Revista Española de Artroscopia y Cirugía Articular está distribuida bajo una licencia de Creative Commons Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional.