Application of fresh osteochondral allografts to the patella. Surgical procedure
Aplicación de aloinjertos osteocondrales frescos en la rótula. Técnica quirúrgica
Resumen:
El tratamiento de las lesiones osteocondrales de la rodilla en pacientes jóvenes y activos continúa siendo un desafío para el cirujano ortopédico. Entre ellas, las lesiones osteocondrales de la rótula son particularmente difíciles de abordar, debido a sus peculiaridades biomecánicas, forma y tamaño. El tratamiento mediante trasplante de aloinjertos osteocondrales frescos en la rótula está indicado para el manejo de las lesiones osteocondrales de rótula mayores de 2 cm2 sin respuesta al tratamiento conservador, en pacientes jóvenes. Presentamos una técnica quirúrgica simple y reproducible para la realización de trasplante osteocondral fresco de la rótula. En lesiones situadas en la parte central de la rótula o que no afecten toda su superficie articular, es preferible emplear la técnica de cilindros osteocondrales. Estos cilindros se obtienen desde el aloinjerto fresco de la rótula, del tamaño adecuado a la lesión, y se introducen en la región de la lesión, obteniendo una fijación a presión pressfit dentro de un defecto creado de forma recíproca en la zona de la lesión. En caso de lesiones multifocales o que afecten toda la superficie patelar, debido a su asimetría, es preferible utilizar la técnica de la concha (shell technique), permitiendo una restauración homogénea de toda la superficie articular. Con la ayuda de una guía estándar de corte patelar de las prótesis de rodilla, en esta técnica se realiza una resección completa del cartílago y parte de su hueso subcondral afectado y de forma similar se utiliza para la obtención en el aloinjerto. Posteriormente, se realiza la fijación con pines bioabsorbibles de 1,5 mm de diámetro desde la superficie articular.
Abstract:
The treatment of osteochondral lesions of the knee in young, active patients remains a challenge for the orthopedic surgeon. Among them, osteochondral lesions of the patella are particularly difficult to manage, due to their biomechanical peculiarities, shape and size. In young patients, treatment based on fresh osteochondral allograft transplantation is indicated in osteochondral lesions of the patella larger than 2 cm2 in size that fail to respond to conservative management. We present a simple and reproducible surgical technique for performing fresh osteochondral transplantation of the patella. In lesions located in the central part of the patella or not affecting the entire articular surface, it is preferable to use the osteochondral cylinders technique. These cylinders are taken from the fresh patellar allograft, sized to match the lesion, and are inserted into the latter, resulting in press fit fixation within a reciprocally created defect in the lesion area. In the case of multifocal lesions or lesions affecting the entire patellar surface, due to its asymmetry, it is preferable to use the shell technique, allowing homogeneous restoration of the entire articular surface. With the aid of a standard patellar cutting guide for knee prostheses, this technique involves complete resection of the cartilage and part of its affected subchondral bone, and is similarly used in allograft harvesting. Subsequently, fixation is performed with 1.5-mm diameter bioabsorbable pins from the articular surface.
Introduction
The management of knee joint injuries in young, active patients remains a challenge for the orthopaedic surgeon(1). Among them, osteochondral lesions of the patella are particularly difficult to treat due to their biomechanical peculiarities, shape and size. In cases where conservative treatment fails, surgical management should be aimed at correcting kinematic alterations of the patellofemoral joint, reducing patellofemoral pressures and, where indicated, addressing osteochondral lesions according to their location, extent and size(2,3,4).
In the treatment of chondral and osteochondral lesions smaller than 2 cm2 there are numerous valid and widely known alternatives(5). In contrast, for the treatment of osteochondral lesions larger than 2 cm2, the alternatives are more limited. This is where the fresh osteochondral allograft transplantation technique finds its treatment target(6). This is defined by performing an en bloc transplant of cartilage and subchondral bone appropriate to the size of the osteochondral lesion, preserved at a specific temperature and preservation medium to allow for chondral cell viability(7,8,9,10).
In the patella, there are two types of techniques depending on the location and size of the lesion. In the case of lesions affecting a localised area of the articular surface, treatment using osteochondral cylinders(bone-dowel or bone-plug technique) is preferred. In the case of lesions affecting the entire patella or multifocal lesions, due to their asymmetry, the shell technique or resurfacing is performed, allowing precise restoration of the anatomy. The latter technique is also of choice in case of bipolar lesions also involving a dysplastic trochlea, as both surfaces should be replaced(11,12).
Surgical procedure
Indications
Osteochondral transplantation of the patella is indicated in young, active patients with osteochondral lesions of the patella larger than 2 cm2. Only patients with severe chronic pain that limits daily activities and without reasonable improvement with conservative management are candidates for this treatment.
Contraindications include advanced osteoarthritis, active infection, tumour pathology, rheumatic disease or vasculopathies that may affect graft integration. Body mass index (BMI) greater than 30 and age over 50 years are relative contraindications.
Instruments and needs
Pre-operative study
All patients undergo the following tests:
- Telemetric, lateral and axial radiographs of both knees.
- MRI to assess osteochondral involvement and associated lesions.
- Knee and torsional computed tomography (CT) scans to assess bone shape and condition, and to measure torsional alterations.
Extraction of the fresh allograft
The tissue bank supplies the allografts and performs all pre-operative processing of the graft. Osteochondral grafts are obtained from donors under 45 years of age. Once a donor is available, grafts are harvested within 12 hours of death. The osteochondral allograft is placed in a transport medium (lactated Ringer's solution) and stored and refrigerated at 4 to 8 °C.
On arrival at the tissue bank, the graft is prepared in a class A clean room where, after removal of the periosteum and soft tissues, it undergoes a pulsatile lavage. High pressure pulsatile washing and dry centrifugation are performed with sterile phosphate buffered saline. Microbiological tests are performed on both the graft and the final wash solution. The allograft is then placed in a solution containing Ringer's lactate and an antibiotic cocktail consisting of vancomycin (50 mg/mL), tobramycin (3 mg/mL), co-trimoxazole (160 mg/mL) and amphotericin (125 mg/mL).
Five days later, microbiological tests are performed again on both the preservation solution and the graft. The graft is kept refrigerated at 4-8°Cuntil implantation within a maximum of 3 weeks after harvesting. Alternatively, it can be maintained at 33 °C in a medium containing human serum for up to 8 weeks. Ideally a CT scan of the graft is requested to aim for a better match with the recipient patella.
Technique
Positioning
The patient is placed in the supine position with a foot support and a lateral thigh support, keeping the knee at 30-45° of flexion. The tourniquet is placed on the thigh and the other leg is placed in full extension.
Diagnostic arthroscopy and approach
Prior to the actual performance of the fresh osteochondral transplantation of the knee, an arthroscopy is performed for a complete evaluation of the knee and to confirm the location and size of the osteochondral lesions. It is also necessary to correct any anatomical alterations (misalignments of the limb or the patellofemoral joint) and/or associated instabilities by osteotomies or ligamentous reconstructions.
In the case of torsional alterations, a de-rotatory osteotomy is indicated; in the case of coronal misalignments, a varus osteotomy; in the case of an increase in the anterior tuberosity-trochlea throat (AT-TG) distance greater than 15 mm, an osteotomy of the anterior tibial tuberosity; and, in the case of patellofemoral instability, reconstruction of the patellofemoral ligament is indicated.
Osteochondral transplantation is preferably performed via a lateral parapatellar approach if only the patellofemoral joint is affected or medially if other areas are also affected or distal realignment is required.
Osteochondral cylinder treatment
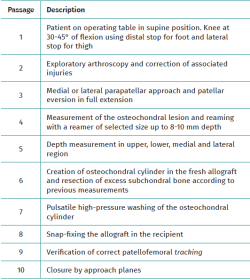
In the case of lesions in the central part of the patella, treatment is carried out using osteochondral cylinders(bone-dowel or bone-plug technique). After eversion of the patella in full extension, the osteochondral lesion is measured using JRF Ortho® (Englewood, CO) instruments (Figure 1A), a Steinmann® pin is placed in the central region of the lesion perpendicular to the surface and the lesion is reamed to a depth of 8-10 mm with a reamer of the appropriate diameter depending on the diameter of the lesion (Figure 1B) using copious saline irrigation to reduce the risk of thermal necrosis. This is followed by measuring the depth at the top, bottom, medial and lateral sides of the created lesion in order to recreate them in the graft (Figure 1C).
Then, holding the fresh allograft in place with the aid of a standard patellar knee prosthesis guide, an osteochondral cylinder is made to a depth of more than 15 mm using the circumferential cutter of the same diameter as the reamer previously used, using JRF Ortho® instruments (Figure 1D). A mark is then made with a sterile marker pen in the upper region of the cylinder for correct orientation and subsequent implantation, and the osteochondral cylinder is removed.
Subsequently, following the depth measurements previously obtained in the lesion created in the patient, these measurements are recreated in the fresh graft by marking the depth in the upper, lower, medial and lateral part with a sterile marker pen. The marks are then connected to create a circumferential depth mark.
Then, holding the cylinder with the specific support and flush with the circumferential depth mark, the excess subchondral bone is resected with a saw to obtain a cylinder of the same depth as the lesion created, to compensate for the defect created (Figure 1E) and that, once the cylinder is in place, it remains flush with the surrounding cartilage.
This is followed by a high-pressure pulsatile flushing of the osteochondral cylinder for 15 minutes to minimise any possible immunological reaction.
Finally, the osteochondral cylinder is inserted into the region of the lesion, usually resulting in a press-fit without the need for fixation (Figure 1F). A femoropatellar tracking test is performed. Closure of the approach can be accomplished by partial advancement of the vastus medialis over the patella to minimise pressure on the lateral facet or by lengthening the lateral flap if access was made on this side.
reacae.31282.fs2401004en-figure1.png
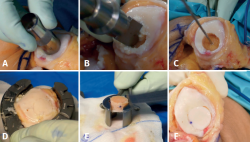
Figure 1. Steps in the technique of fresh osteochondral transplantation of bone-plug type cylinders or bone-plugs. A: measurement of the diameter of the defect; B: milling and preparation of the recipient site; C: defect already created in the patella; D: preparation of the cylinder in the fresh graft; E: reduction of the thickness to the desired thickness; F: final appearance.
The step-by-step technique is described in Table 1.
Treatment using the shell technique
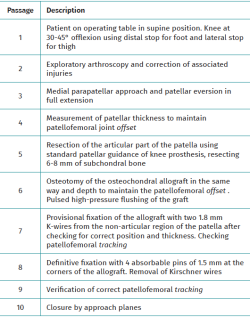
In the case of injuries affecting the entire patella, due to its asymmetry, the shell technique or resurfacing is performed, allowing precise restoration of the anatomy. After eversion of the patella in full extension, patellar thickness measurement is performed to maintain the offset of the patellofemoral joint, to avoid an increase in patellar thickness after osteochondral transplantation that would increase the pressure on the patellofemoral joint.
Circumferential denervation of the patella is performed. The patella is then clamped with the aid of a standard patellar knee prosthesis guide and the articular part of the patella is resected (Figure 2A). The positioning of the guide wire must be very careful to remove only 6-8 mm of subchondral bone. This is critical because the more donor subchondral bone that is transplanted, the greater the chance of immune reaction and lack of integration in the recipient.
Subsequently, using the same patellar guide and the same saw, the osteochondral graft is cut in order to obtain a final patellar thickness that matches the original patellar thickness. In this regard, it is very useful to perform measurement with calipers (Figure 2B), which are usually also found in the knee prosthesis instrument kit. Adherent soft tissues are removed to reduce immunogenicity.
The osteochondral graft is then flushed with a high-pressure pulse for 15 minutes to minimise any possible immunological reaction. Using a sterile marker pen, the top of the graft is marked to assist in its correct positioning.
After correct orientation of the osteochondral graft in the recipient bone and verification that the previous patellar thickness is maintained, temporary fixation is performed using 2 or 3 K-wires of 1.8 mm from the non-articular part of the patella (anterior to posterior), avoiding cartilage injury.
The femoropatellar tracking test is performed. Once satisfactory femoropatellar tracking is obtained, definitive fixation is performed using 1.5 mm absorbable pins (SmartNail®, Conmed, Largo, FL) positioned antegrade from the articular cartilage (Figure 2C). On occasions where the trochlea is very dysplastic and with degenerative changes, a similar procedure should also be performed on it (Figure 2D), in order to have perfect joint congruency. Placement of a pin at each corner of the patella is recommended to obtain proper fixation and to avoid damage to the cartilage surface involved in patellar friction with the trochlea (Figure 2E).
reacae.31282.fs2401004en-figure2.png
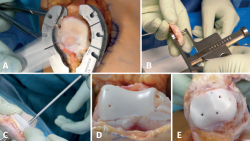
Figure 2. Steps of the shell-type fresh osteochondral transplantation technique. A: resection of the articular surface of the patella using standard forceps; B: measurement of the total thickness of the fresh allograft after preparation; C: fixation of the graft with 1.5 mm diameter resorbable pins from the articular side; D: sometimes the trochlea also needs to be replaced; E: final appearance.
Subsequently, the K-wires are removed and the femoropatellar tracking is rechecked. Closure of the approach can be accomplished by partial advancement of the vastus medialis over the patella to minimise pressure on the lateral facet.
The step-by-step technique is described in Table 2.
Postoperative management
Continuous controlled passive movement is initiated within the first hours after surgery. Unlimited joint balance is allowed from the start, as well as isometric exercises of the quadriceps and hamstrings. Full weight bearing of the extremity is only allowed with the knee brace blocked in extension. The knee brace is only needed for weight bearing and is completely removed after 4-6 weeks. After the first month, rehabilitation focuses on recovery of complete joint balance and strengthening. Athletic activities should be limited to light sports.
Postoperative CT and MRI scans are recommended after 6 months to assess cartilage integrity and osseointegration of the graft(13,14,15,16,17).
Discussion
Treatment of large osteochondral lesions of the patella in young patients by fresh osteochondral transplantation provides a high number of viable chondrocytes in the extracellular matrix of the cartilage and restores the normal shape of the patellofemoral joint and its biomechanics. This allows symptomatic and functional improvement with the possibility of delaying or eliminating the need for prosthetic surgery.
The disadvantage of fresh allografts is the logistical and economic limitation, as the storage time is limited to a few weeks after procurement and the cost is considerable.
The surgical techniques described are valid and perhaps the most appropriate options for the treatment of severe osteochondral lesions of the patella in young patients with disabling anterior knee pain.
Figuras
Figure 1. Steps in the technique of fresh osteochondral transplantation of bone-plug type cylinders or bone-plugs. A: measurement of the diameter of the defect; B: milling and preparation of the recipient site; C: defect already created in the patella; D: preparation of the cylinder in the fresh graft; E: reduction of the thickness to the desired thickness; F: final appearance.
Figure 2. Steps of the shell-type fresh osteochondral transplantation technique. A: resection of the articular surface of the patella using standard forceps; B: measurement of the total thickness of the fresh allograft after preparation; C: fixation of the graft with 1.5 mm diameter resorbable pins from the articular side; D: sometimes the trochlea also needs to be replaced; E: final appearance.
Tablas
Table 1. Step-by-step surgical technique: osteochondral transplantation of the patella using an osteochondral cylinder
Información del artículo
Cita bibliográfica
Autores
Pablo Eduardo Gelber Ghertner
Departamento de Cirugía Ortopédica. Hospital de la Santa Creu i Sant Pau. Universitat Autonoma de Barcelona (UAB). Barcelona
ReSport Clinic, Barcelona
Unidad de Artroscopia y Rodilla. ICATME-Institut Universitari Dexeus.
Eduard Ramírez Bermejo
Departamento de Cirugía Ortopédica. Hospital de la Santa Creu i Sant Pau. Universitat Autonoma de Barcelona (UAB). Barcelona
Ethical responsibilities
Conflicts of interest. The authors state that they have no conflicts of interest.
Financial support. This study has received no financial support.
Protection of people and animals. The authors declare that this research has not involved human or animal experimentation.
Data confidentiality. The authors declare that the protocols of their work centre referred to the publication of patient information have been followed.
Right to privacy and informed consent. The authors declare that no patient data appear in this article.
Referencias bibliográficas
-
1Chahla J, Stone J, Mandelbaum BR. How to Manage Cartilage Injuries? Arthroscopy. 2019;35(10):2771-3.
-
2Lording T, Lustig S, Servien E, Neyret P. Chondral Injury in Patellofemoral Instability. Cartilage. 2014;5(3):136-44.
-
3Mason JJ, Leszko F, Johnson T, Komistek RD. Patellofemoral joint forces. J Biomech. 2008;41(11):2337-48.
-
4Draper CE, Besier TF, Gold GE, et al. Is cartilage thickness different in young subjects with and without patellofemoral pain? Osteoarthr Cartil. 2006;14:931-7.
-
5Chahla J, Hinckel BB, Yanke AB, et al. An Expert Consensus Statement on the Management of Large Chondral and Osteochondral Defects in the Patellofemoral Joint. Orthop J Sport Med. 2020;8(3).
-
6Roselló-Añón A, Mirabet Lis V, Fariñas O, Gelber P, Sanchís-Alfonso V. Injerto de cartílago en fresco. Indicaciones, técnica quirúrgica y evidencia científica. Rev Esp Artrosc Cir Articul. 2021;28(1).
-
7Hangody L, Vásárhelyi G, Hangody LR, et al. Autologous osteochondral grafting--technique and long-term results. Injury. 2008;39:32-9.
-
8Niemeyer P, Albrecht D, Andereya S, et al. Autologous chondrocyte implantation (ACI) for cartilage defects of the knee: A guideline by the working group “Clinical Tissue Regeneration” of the German Society of Orthopaedics and Trauma (DGOU). Knee. 2016;23:426-35.
-
9Filardo G, Kon E, Andriolo L, Di Martino A, Zaffagnini S, Marcacci M. Treatment of “Patellofemoral” Cartilage Lesions With Matrix-Assisted Autologous Chondrocyte Transplantation. Am J Sports Med. 2013;42(3):626-34.
-
10Sherman SL, Garrity J, Bauer K, Cook J, Stannard J, Bugbee W. Fresh osteochondral allograft transplantation for the knee: Current concepts. J Am Acad Orthop Surg. 2014;22(2):121-33.
-
11Gelber PE, Ramírez-Bermejo E, Ibáñez M, Grau-Blanes A, Fariñas O, Monllau JC. Fresh Osteochondral Resurfacing of the Patellofemoral Joint. Arthrosc Tech. 2019;8(11):e1395-401.
-
12Gelber PE, Perelli S, Ibáñez M, et al. Fresh Osteochondral Patellar Allograft Resurfacing. Arthrosc Tech. 2018;7(6):e617-22.
-
13Gelber PE, Ramírez-Bermejo E, Grau-Blanes A, González-Osuna A, Fariñas O. Computerized tomography scan evaluation after fresh osteochondral allograft transplantation of the knee correlates with clinical outcomes. Int Orthop. 2022;46(7):1539-45.
-
14Gelber PE, Ramírez-Bermejo E, Fariñas O. Early Postoperative CT Scan Provides Prognostic Data on Clinical Outcomes of Fresh Osteochondral Transplantation of the Knee. Am J Sports Med. 2022;50(14):3812-8.
-
15Gelber PE, Ramírez-Bermejo E, Grau-Blanes A, González-Osuna A, Llauger J, Fariñas O. A new computed tomography scoring system to assess osteochondral allograft transplantation for the knee: inter-observer and intra-observer agreement. Int Orthop. 2021;45(5):1191-7.
-
16Meric G, Gracitelli GC, McCauley JC, et al. Osteochondral Allograft MRI Scoring System (OCAMRISS) in the Knee: Interobserver Agreement and Clinical Application. Cartilage. 2015;6(3):142-9.
-
17Chang EY, Pallante-Kichura AL, Bae WC, et al. Development of a Comprehensive Osteochondral Allograft MRI Scoring System (OCAMRISS) With Histopathologic, Micro-Computed Tomography, and Biomechanical Validation. Cartilage. 2014;5(1):16-27.
Descargar artículo:
Licencia:
Este contenido es de acceso abierto (Open-Access) y se ha distribuido bajo los términos de la licencia Creative Commons CC BY-NC-ND (Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional) que permite usar, distribuir y reproducir en cualquier medio siempre que se citen a los autores y no se utilice para fines comerciales ni para hacer obras derivadas.
Comparte este contenido
En esta edición
- Learning from the best
- Everyone's effort
- Inclusion of the long portion of the biceps in rotator cuff repairs
- Surgical technique of the arthroscopic Latarjet procedure with button fixation
- Arthroscopic lateral collateral ligament plication of the elbow
- Arthroscopy-assisted treatment of metacarpophalangeal joint fractures of the fingers
- Surgical technique of hip arthroscopy without perineal post
- Direct reattachment in anterior cruciate ligament ruptures
- Application of fresh osteochondral allografts to the patella. Surgical procedure
- Arthroscopic ligamentoplasty for lateral ankle instability
- Two handles to grasp: double bucket-handle meniscal lesion
Más en PUBMED
Más en Google Scholar
Más en ORCID


Revista Española de Artroscopia y Cirugía Articular está distribuida bajo una licencia de Creative Commons Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional.