Evolution of glenohumeral bone defects following failed arthroscopic Bankart repair. Study of a case series
Evolución de los defectos óseos glenohumerales tras el fracaso de la reparación de Bankart artroscópica. Estudio de una serie de casos
Resumen:
Objetivo: estudiar la evolución del tamaño de los defectos óseos en pacientes con inestabilidad glenohumeral en los que la primera cirugía ha fracasado.
Material y métodos: se estudiaron 9 pacientes intervenidos por inestabilidad anterior mediante reparación artroscópica de lesión de Bankart que recurrieron tras la operación. Mediante resonancia magnética se analizó el tamaño de los defectos óseos y el tracking glenohumeral antes de la cirugía y después de que esta fracasase. Se determinó el tamaño y la profundidad de la lesión de Hill-Sachs y el porcentaje del defecto glenoideo.
Resultados: tras fracasar la cirugía, tanto la lesión de Hill-Sachs como el defecto glenoideo aumentaron de tamaño. El diámetro del Hill-Sachs pasó de 1,37 cm de media a 1,54 cm (p = 0,004); la profundidad del defecto humeral pasó de 0,38 a 0,48 cm (p = 0,1). El defecto óseo glenoideo aumentó del 9,62% al 18,7% (p = 0,006). No se encontró correlación entre el tamaño del defecto glenoideo y el tamaño de la lesión de Hill-Sachs. El número de lesiones off track aumentó de 1 a 7 al fracasar la cirugía.
Conclusiones: los defectos óseos presentes en pacientes con inestabilidad de hombro aumentan de tamaño al fracasar la cirugía de reparación de Bankart artroscópica y se produce una mayor incidencia de lesiones off track al fracasar el tratamiento.
Nivel de evidencia: nivel de evidencia IV (serie de casos).
Relevancia clínica: el presente estudio evalúa cómo aumentan de tamaño los defectos óseos presentes en casos de inestabilidad anterior de hombro cuando se producen recidivas tras el fracaso de la operación. El fracaso de la intervención artroscópica de Bankart lleva a una mayor afectación secundaria de la glena en comparación con las lesiones de la cabeza humeral, modificando drásticamente el tracking glenohumeral respecto al previo a la intervención.
Abstract:
Objective: To evaluate the evolution of bone defect size in patients with glenohumeral instability in which first surgery has failed.
Material and methods: The study involved 9 patients subjected to arthroscopic Bankart repair due to anterior instability and who suffered recurrence after the operation. Magnetic resonance imaging was used to analyse the size of the bone defects and glenohumeral tracking before surgery and after surgical failure. The size and depth of the Hill-Sachs lesion and the glenoid defect percentage were determined.
Results: Following surgical failure, both the Hill-Sachs lesion and the glenoid defect increased in size. The diameter of the Hill-Sachs lesion increased from a mean of 1.37 cm to 1.54 cm (p = 0.004), and the depth of the humeral defect increased from 0.38 cm to 0.48 cm (p = 0.1). The glenoid bone defect increased from 9.62% to 18.7% (p = 0.006). No correlation was found between the size of the glenoid defect and the size of the Hill-Sachs lesion. The number of off-track lesions increased from 1 to 7 after surgical failure.
Conclusions: Bone defects in patients with shoulder instability increase in size after failed arthroscopic Bankart repair surgery, with an increased incidence of off-track lesions secondary to treatment failure.
Level of evidence: level of evidence IV (case series).
Clinical relevance: the present study evaluates the increase in bone defect size in patients with anterior shoulder instability when relapse occurs following surgical failure. Failed arthroscopic Bankart repair results in greater secondary glenoid cavity involvement compared with humeral head lesions, drastically modifying glenohumeral tracking with respect to the situation prior to surgery.
Introduction
The prevalence of bone lesions associated to anterior glenohumeral instability has been widely described in the literature. Bone lesions associated to anterior instability comprise Hill-Sachs lesion, or posterolateral humeral head compression fracture, and bony Bankart lesion, characterised by fracture or substance loss at the anteroinferior glenoid margin(1). The presence of these bone defects is a cause for concern among surgeons when treating patients with anterior shoulder instability.
In order to explain the role of these bone defects, in recent years the concept of the "engaging" Hill-Sachs lesion, in which the bone defect extends beyond the glenoid cavity protective margin, has evolved into the concept of glenoid tracking – based on the contact area between the glenoid cavity and the humeral head, and the interaction between them(2,3). Specifically, those defects which despite their size maintain good contact between bone surfaces are considered to be on-track lesions, while those characterised by contact loss favouring dislocation are regarded as off-track lesions(4,5). Application of the glenohumeral tracking model has been shown to be a reliable predictor of the recurrence of instability(6), and there is a direct relationship between off-track lesions and arthroscopic surgery failure(7).
Although the success rate of the arthroscopic management of instability is high, failure can occur, with the need for revision surgery. The reported relapse rate ranges between 6-35%(8). The approach may vary from new arthroscopic revision surgery of the soft tissue lesions to open or arthroscopic surgical techniques to manage the bone defects.
Little is known about the evolution of bone defects in cases where new dislocations appear following a first arthroscopic operation. Some authors have compared patients subjected to primary surgery versus patients subjected to revision surgery, with the observation of a greater prevalence of defects in the latter(9). Nevertheless, it is not fully clear how these defects progress following dislocation recurrence or whether there is a possible relationship between increased glenoid bone damage and the humeral head defects.
The present study evaluates the changes in the presence and size of shoulder bone lesions in a series of patients subjected to arthroscopic Bankart repair due to shoulder instability and who subsequently suffered recurrence of instability, performing a quantitative analysis based on magnetic resonance imaging data.
Material and methods
A retrospective review was made of those patients operated upon at our centre due to traumatic anterior shoulder instability between 2014 and 2020. The study inclusion criteria were patients with shoulder instability and clinical manifestations of relapsing luxation of traumatic origin, subjected to arthroscopic Bankart repair surgery, and who suffered recurrence of instability at some point during postoperative follow-up. Patients over 55 years of age, as well as individuals with atraumatic instability, with previous revision surgeries, or with missing radiological data were excluded.
Descriptive parameters
The study data comprised the patient age at the time of the first operation, whether the dominant or the non-dominant arm was involved, the presence of shoulder laxity at physical examination, the number of dislocations experienced before first surgery, and the total number of dislocations at the end of follow-up. We also recorded the number of times the patients required assisted reduction in the operating room. Retrospective application was made of the Instability Severity Index Score (ISIS)(10) before Bankart repair. The intraoperative findings and the associated lesions were recorded from the surgical records of the patients. The moment during follow-up in which surgical failure occurred was documented, along with the number of luxation episodes and reductions under anaesthesia after failure of the first operation.
Measurement of bone defects and glenohumeral tracking
The magnitude of the bone defects and glenohumeral tracking of the shoulders was determined both before primary stabilisation surgery and after the recurrence of instability. The measurements were made by adapting the magnetic resonance imaging-based glenoid tracking measurements described by Gyftopoulos et al.(11,12). The magnitude of the glenoid cavity bone defect was determined from the coronal acquisitions based on the best-fit circle technique(13). The critical bony Bankart threshold was defined as a defect of over 25% of the diameter of the glenoid cavity. However, since the most recent literature lowers this threshold(14), we define a subcritical threshold with a detect of 15-25% of the glenoid cavity. Examination of the axial acquisitions determined the anteroposterior diameter of the defect of the humeral head, defining it as the Hill-Sachs interval (HSI), together with the depth of the lesion. The relationship between the HSI and the glenoid defect measurements determined whether the lesion was on-track or off-track(15). We reviewed the preoperative magnetic resonance images as well as the surgical records of the first operation in search of other associated lesions.
The statistical analysis was performed using the PSPP 1.4.1 package. All quantitative variables were assessed for normal data distribution using the Kolmogorov-Smirnov test. Paired sample comparisons were made, seeking correlations between independent quantitative variables. Statistical significance was considered for p < 0.05.
Results
Out of 70 patients with anterior shoulder instability, we identified 11 cases of failed first surgery (15.7%). Two of these subjects were excluded due to a lack of test data before the first operation, thus leaving a total of 9 patients for evaluation in the study (Table 1).
The mean patient age at the time of first surgery was 23.7 years (range 18-37). All of the patients were routinely involved in some sports activity, with one military professional who performed frequent high-demand exercise, and 7 federated athletes. The mean ISIS score was 5 points (range 2-8) before the operation.
The mean time from first surgery to the recurrence of instability was 12.4 months (range 3-36), and in three of the 9 patients instability occurred while practicing their usual sports. Of the 9 patients, 7 suffered new shoulder dislocations, while two subjects experienced repeated subluxation episodes. Five patients suffered dislocation during activities other than sports. One patient experienced relapse as a consequence of an epileptic crisis. The mean number of dislocation episodes after surgical failure was 1.3 (range 0-5). Revision surgery was performed in 7 of the 9 cases. In four cases arthroscopic revision of the Bankart lesion was made, and in three of them ligamentoplasty was performed according to the technique described by Cimiano and Sánchez(16), while in the fourth patient an open Latarjet procedure was carried out with arthroscopic remplissage of the humeral head. An open Latarjet procedure was decided in the remaining three cases. Three patients subjected to arthroscopic surgery resumed their sports activity at the same level as before relapse. One of the patients had to abandon the sport entirely, while the rest were able to resume their sports activities albeit at a lower level.
Evolution of the bone defects and glenohumeral tracking
A comparative analysis was made of the dimensions of the shoulder bone defects before and after primary surgery failure. An increase in lesion size was recorded for both the humeral head and the glenoid cavity following failure of the previous operation (Figure 1).
The mean HSI prior to surgery was 1.4 cm (range 0.8-1.8). The mean HSI after surgical failure was 1.8 cm (range 0.9-2.6 ); the difference proved statistically significant (p = 0.004). The mean depth of the Hill-Sachs lesion was 0.4 cm (range 0.2-0.8) before the operation, versus 0.5 cm (range 0.25-0.8) after relapse. The differences were not significant (p=0.1).
The bony Bankart lesion showed the greatest increase in size between primary surgery, with a mean preoperative defect of 9.6% (range 0-29%), and surgical failure, with a mean defect of 18.7% (range 8-36%). The differences were statistically significant (p=0.006). Only two of the 9 patients had a preoperative glenoid defect of over 15%, while after surgical failure 6 patients had bone defects of over 15% and two subjects presented substance losses in excess of 25% (Figure 2).
reacae.29377.fs2202002en-figure2.png
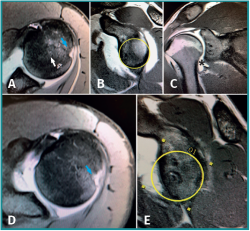
Figure 2. Magnetic resonance imaging view of a 19-year-old patient with glenohumeral instability and associated inferior glenohumeral ligament damage (asterisk). A and B: preoperative axial and sagittal views. Note the integrity of the glenoid cavity and the Hill-Sachs lesion (arrow). The ligament lesion went unnoticed and only arthroscopic Bankart repair was carried out. The patient suffered a new dislocation episode 6 months after the operation. D and E: axial and sagittal magnetic resonance imaging views after Bankart surgery failure. Note the increase in size of the Hill-Sachs lesion and important anterior glenoid cavity defect with respect to the presurgical magnetic resonance imaging study.
Before primary Bankart surgery, only one of the 9 shoulders presented an off-track lesion according to the head-glenoid cavity index. However, following the failure of Bankart repair, 7 of the 9 lesions were considered to be off-track.
On comparing the humeral bone defect with respect to the glenoid bone defect after surgical failure, no correlation was found between the size or depth of the Hill-Sachs lesion and the size of the bony Bankart lesion. The correlation coefficients between HSI and the bony Bankart defect, between HSI and the depth of the Hill-Sachs lesion, and between the depth of the Hill-Sachs lesion and the bony Bankart defect were -0.19, 0.15 and 0.05, respectively, i.e., all very low and with p > 0.05. The number of episodes experienced or the number of reductions performed under anaesthesia likewise showed no correlation to the size of the observed bone defects. In contrast, a moderate positive correlation was found between the number of luxation episodes and the preoperative ISIS (r = 0.77; p = 0.02).
Soft tissue lesions
Three of the 9 patients presented inferior glenohumeral ligament (IGHL) damage: in two cases this corresponded to humeral avulsion of the glenohumeral ligaments (HAGL) and in the third case to tearing of the glenoid insertion. Two patients presented type V superior labrum anterior and posterior (SLAP) tear, while one patient presented type IV SLAP tear. The remaining three patients had no additional lesions. In two of the cases with damage to the IGHL, the lesion was not initially detected or taken into account in the preoperative images, while in the third case the lesion was obviated in the arthroscopic treatment and only repair of the anteroinferior labrum was carried out. The SLAP lesions were detected during the surgical procedure and treated by re-anchoring with implants. The patients with IGHL lesions presented the greatest degree of damage to the anterior glenoid cavity after surgical failure in the entire sample, with an increase from 5.4% on average (range 3.1-30) to 28.9% (range 20-36).
Discussion
The present study describes 9 cases of recurrent anterior shoulder instability following first surgery, in which the bone lesions increased in size at both humeral level (Hill-Sachs lesion) and in the anterior glenoid cavity region (bony Bankart lesion). Each lesion evolved independently (no correlation being observed between the increase in size of the Hill-Sachs lesion and the increase in size of the bony Bankart lesion), and the increase in size was more significant in the case of the anterior glenoid cavity lesion, which almost doubled its initial size.
The incidence of bone lesions in anterior shoulder instability is very high. Edwards et al., in a radiographic study of 160 patients, found the incidence of bone lesions to be up to 95%(17). Although studies have been made of the mechanism underlying the bone lesions, the concrete moment in which these defects are produced is not fully clear. While some authors consider that the defects occur at the time of luxation, others are of the opinion that they can appear during reduction or some time after the luxation episode. It seems that the size of the humeral head lesions in instability is greater in patients with a chronic course, several luxation episodes, and in cases with a longer interval between luxation and reduction(18). Other studies have found adolescence and a history of multiple luxations to be factors associated to the appearance of off-track lesions and thus to a greater size of the pre-existing bone defects(19). Duchman et al.(9) found the bone defects to be more frequent and of greater size in patients subjected to instability revision surgery than in subjects with primary instability. However, to our knowledge, no studies have focused on the natural evolution of these defects in a series of patients in which arthroscopic Bankart surgery has failed.
In our series, instability relapse after the operation resulted in an increased size of the bone lesions compared with the size at the time of primary surgery. This increase in bone defects occurred with a low number of repeat luxation episodes (1.3 on average), and in two cases was recorded simply in subluxation episodes, with no clear luxation as such.
The HSI was seen to increase significantly in all patients, suggesting that the diameter of the Hill-Sachs lesion increases as a result of the recurrence of instability. However, the depth of the lesion did not vary significantly with respect to the previous situation. We consider that this may be consistent with the mechanism causing the lesion through compression of the head against the glenoid cavity at shoulder dislocation(4).
With regard to the glenoid cavity, a very significant increase in the size of the glenoid lesion was recorded with the appearance of new instability episodes. This increase in size was more notorious than that seen in the Hill-Sachs lesion. While the presurgical HSI ranged between 0.5-2 cm, and its increase was relatively uniform in all the patients, the size of the glenoid defect varied greatly from one patient to another, with some subjects presenting defects of < 10% and others of 10-20%. Although the size of the glenoid defect increased with the presence of relapses in the same way as was seen with the HSI, in the glenoid cavity the increase in lesion size almost doubled the initial size, resulting in defects of up to 15% in two-thirds of the patients. Damage of the glenoid cavity is important within the lesion mechanism, since a sufficiently large glenoid defect can produce instability over moderate motion ranges, particularly in the presence of a sufficiently extensive Hill-Sachs lesion(4), while the Hill-Sachs lesion appears to be more associated to the abduction and external rotation mechanism, producing instability at the end of the arc of motion(20). Traditionally, a glenoid defect threshold of 25% was accepted as an indication for bone stop surgery instead of isolated Bankart repair. However, the evidence produced by the literature in recent years supports the advisability of lowering this threshold. Dickens et al. carried out a study in university American football players subjected to arthroscopic surgery for shoulder instability, and recorded a greater risk of relapse in those patients with a bony Bankart lesion of over 13.5%(21). Arciero et al.(14), in a meta-analysis, reported that glenoid defects of over 15% should be considered for open repair instead of laparoscopic repair. Accordingly, in our study the critical threshold of the glenoid defect was taken to be the traditional percentage of > 25%, and we defined a "subcritical" interval of 15-25% where an increased risk of recurrence could be estimated, according to these authors. Before undergoing surgery for the first time, only two of the patients in our series presented a glenoid defect of over 15%. However, following the recurrence of instability, 6 of the 9 patients exceeded the subcritical threshold. This progression clearly affects the relationship of the joint surfaces, altering glenoid tracking. Compared with a single patient with an off-track lesion at the time of primary arthroscopy, a total of 7 patients presented off-track lesions following the recurrence of instability, due to the increase in the extent of the bone lesions.
The different evolution of each of the lesions confirms the findings of other authors. Ciais et al.(22) analysed the bone lesions of the radiographs of 30 patients with shoulder instability and found no correlation between the size of the Hill-Sachs lesion and the loss of substance of the glenoid cavity. Our findings suggest that the Hill-Sachs lesion progresses to a lesser degree in cases of instability failure, while the glenoid cavity is affected to a much greater extent.
In our series, the three patients with glenoid defects of 20% or more corresponded to individuals with associated humeral avulsion of the glenohumeral ligaments (HAGL) or inferior glenohumeral ligament (IGHL) damage. The relapses of these three patients with IGHL damage occurred earlier than in the rest of the patients: in all cases failure manifested within 6 months after the first operation (3, 6 and 6 months). Humeral avulsion of the glenohumeral ligaments has been described as a cause of instability recurrence even after successful Bankart surgery(23,24). Significant differences cannot be established in view of the limited sample size. However, we consider that this type of lesion should be taken into account, due to the early relapses and large glenoid defect sizes observed. Itoi et al. suggested that in the presence of a significant bone defect of the glenoid cavity, beyond a certain degree of abduction, the head ceases to be contained by it, and the anteroinferior capsule becomes the only structure that can counter instability(4). We believe that loss of the retaining capacity of the capsule might generate much greater impact of the humeral head on the anteroinferior margin of the glenoid cavity, which could lead to greater substance loss in the event of relapse.
The main limitation of the present study is the fact that it is a retrospective case series review, with a very small sample size. This implies that although we may offer a detailed description of the evolution of the bone defects in the event of failed arthroscopic Bankart surgery, no solid conclusions can be drawn, as this would require a larger sample size. This is particularly true in the case of the associated lesions, where IGHL damage is seen to potentially have more serious consequences for the anterior glenoid cavity lesion, but no significant differences can be established due to the very small sample size (n = 3) that precludes comparative statistical testing.
Magnetic resonance imaging was used in our study to evaluate the bone lesions. This may come into conflict with the current recommendations, since computed tomography (CT) is considered to be the gold standard for the evaluation of bone defects and glenohumeral tracking(4). However, Gyftopoulos et al.(11,12,25) have shown that magnetic resonance imaging offers good diagnostic precision and can be used to predict glenoid tracking on planning management of the instability.
The present study confirms that glenohumeral luxation relapse after surgery due to anteroinferior shoulder instability produces an increase in size of the bone lesions already present at the time of first surgery, affecting especially the glenoid cavity and producing substance losses of sufficient relevance to alter glenoid tracking. Likewise, although the sample size is very small, the findings of our series suggest that the presence of IGHL damage can lead to increased glenoid bone loss and to early relapse. It is therefore very important to detect such damage and to take it into account when planning first surgical treatment.
Conclusions
The bone defects found in patients with anterior shoulder instability present at the time of arthroscopic Bankart repair surgery increase in size upon failure of surgery, with new luxation episodes. A significant increase in the diameter of the Hill-Sachs lesion and of the size of the bony Bankart defect occurs. The increase in size of these bone defects results in an increased incidence of off-track lesions secondary to treatment failure.
Tablas
Figuras
Figure 1. Evolution of the bone defects before surgery and following surgical failure. A: depth of the Hill-Sachs lesion; B: Hill-Sachs interval (HSI); C: Bony Bankart lesion as percentage.
Figure 2. Magnetic resonance imaging view of a 19-year-old patient with glenohumeral instability and associated inferior glenohumeral ligament damage (asterisk). A and B: preoperative axial and sagittal views. Note the integrity of the glenoid cavity and the Hill-Sachs lesion (arrow). The ligament lesion went unnoticed and only arthroscopic Bankart repair was carried out. The patient suffered a new dislocation episode 6 months after the operation. D and E: axial and sagittal magnetic resonance imaging views after Bankart surgery failure. Note the increase in size of the Hill-Sachs lesion and important anterior glenoid cavity defect with respect to the presurgical magnetic resonance imaging study.
Información del artículo
Cita bibliográfica
Autores
Ricardo Jesús Escribano Rey
Unidad de Traumatología Deportiva. Clínica San Miguel. Pamplona
Jesús Alfaro Adrián
Unidad de Traumatología Deportiva. Clínica San Miguel. Pamplona
Ethical responsibilities
Conflicts of interest. The authors state that they have no conflicts of interest.
Financial support. This study has received no financial support.
Protection of people and animals. The authors declare that this research has not involved human or animal experimentation.
Data confidentiality. The authors declare that the protocols of their work centre referred to the publication of patient information have been followed.
Right to privacy and informed consent. The authors declare that no patient data appear in this article.
Referencias bibliográficas
-
1Yates J, Choudhry MN, Waseem M. Managing Bony Defects of the shoulder joint that occur in association with Dislocation. Open Orthop J. 2017; 10(11):1245-57.
-
2Momaya A, Tokish J. Applying the glenoid track concept in the management of patients with anterior Shoulder instability. Curr Rev Musculoskelet Med. 2017;10:463-8.
-
3Di Giacomo, de Gasperis N, Scarso P. Bipolar bone defect in the shoulder anterior dislocation. Knee Surg Sports Traumatol Arthrosc. 2016 Feb;24(2):479-88.
-
4Itoi E. “On track” and “off track” shoulder lesions. EFORT Open Rev. 2017;2:343-51.
-
5Di Giacomo G, Itoi E, Burkhart SS. Evolving concept of bipolar bone loss and the Hill-Sachs lesion: from "engaging/non-engaging" lesion to "on-track/off-track" lesion. Arthroscopy. 2014 Jan;30(1):90-8.
-
6Shaha JS, Cook JB, Rowles DJ, Bottoni CR, Shaha SH, Tokish JM. Clinical Validation of the Glenoid Track Concept in Anterior Glenohumeral Instability. J Bone Joint Surg (Am.) 2016 Nov 16;98(22):1918-23.
-
7Locher J, Wilken F, Beitzel K, et al. Hill-Sachs Off-track Lesions as Risk Factor for Recurrence of Instability After Arthroscopic Bankart Repair Arthroscopy. 2016 Oct;32(10):1993-9.
-
8Waterman B, Leroux T, Frank R, Romeo A. The evaluation and management of the failed primary arthroscopic Bankart repair. J Am Acad Orthop Surg. 2020 Aug 1;28(15):607-16.
-
9Duchman K, Hettrich C, Glass N, et al. The Incidence of Glenohumeral Bone and Cartilage Lesions at the Time of Anterior Shoulder Stabilization Surgery: A Comparison of Patients Undergoing Primary and Revision Surgery. Am J Sports Med. 2018 Aug; 46(10):2449-56.
-
10Balg F, Boileau P. The instability severity index score. A simple pre-operative score to select patients for arthroscopic or open shoulder stabilisation. J Bone Joint Surg Br. 2007 Nov;89(11):1470-7.
-
11Gyftopoulos S, Hasan S, Bencardino J, et al. Diagnostic accuracy of MRI in the measurement of glenoid bone loss. AJR Am J Roentgenol. 2012;199(4):873-8.
-
12Gyftopoulos S, Yemin A, Beltran L, Babb J, Bencardino J. Engaging Hill-Sachs lesion: is there an association between this lesion and findings on MRI? AJR Am J Roentgenol. 2013;201(4):633-8.
-
13Saliken DJ, Bornes TD, Bouliane MJ, Sheps DM, Beaupre LA. Imaging methods for quantifying glenoid and Hill-Sachs bone loss in traumatic instability of the shoulder: a scoping review. BMC Musculoskelet Disord. 2015;16:164.
-
14Levy B, Grimm N, Arciero R. When to Abandon the Arthroscopic Bankart Repair: A Systematic Review. Sports Health 2020;12(5):425-30.
-
15Yang TC, Chen KH, Chiang ER, Chang MC, Ma HL. Using the Hill-Sachs interval to glenoid track width ratio for prediction of recurrent instability after arthroscopic Bankart repair. Orthop Traumatol Surg Res. 2018;104(6):797-801.
-
16Cimiano F, Sánchez M. Ligamentoplastia de hombro. Nueva técnica. Cuad Artroscop. 2011;18(1);44:28-30.
-
17Edwards T, Bouhalia A, Walch G. Arthroscopy. Radiographic analysis of bone defects in chronic anterior shoulder instability. Arthroscopy. 2003 Sep;19(7):732-9.
-
18Yamamoto N, Itoi E. Osseus defects seen in patients with recurrent shoulder instability. Clin Orthop Surg. 2015 Dec;7(4):425-9.
-
19Lau BC, Conway D, Curran PF, Feeley BT, Pandya NK. Bipolar Bone Loss in Patients With Anterior Shoulder Dislocation: A Comparison of Adolescents Versus Adult Patients. Arthroscopy. 2017;33(10):1755-61.
-
20Fox A, Sánchez A, Tajacz T, Provencher M. Understanding the Hill Sachs lesion. Curr Rev Musculoskelet Med. 2017;10:469-79.
-
21Dickens JF, Owens BD, Cameron KL, et al. The Effect of Subcritical Bone Loss and Exposure on Recurrent Instability After Arthroscopic Bankart Repair in Intercollegiate American Football. Am J Sports Med. 2017;45(8):1769-75.
-
22Ciais G, Klouche S, Fournier A, Rousseau B, Bauer T, Hardy P. Bony defects in chronic anterior posttraumatic dislocation of the shoulder: Is there a correlation between humeral and glenoidal lesions? Eur J Orthop Surg Traumatol. 2016 Aug;26(6):581-6.
-
23Schippinger G, Vasiu PS, Fankhauser F, Clement HG. HAGL lesion occurring after successful arthroscopic Bankart repair. Arthroscopy. 2001 Feb;17(2):206-8.
-
24Celik H, Seckin MF, Kara A, Akman S. Isolated HAGL lesion after arthroscopic Bankart repair in a professional soccer player. Phys Sportsmed. 2017 May;45(2):199-202.
-
25Gyftopoulos S, Beltran L, Bookman J, Rokito A, MRI Evaluation of Bipolar Bone Loss Using the On-Track Off-Track Method: A Feasibility Study. J Roentgenol. 2015;205(4):848-52.
Descargar artículo:
Licencia:
Este contenido es de acceso abierto (Open-Access) y se ha distribuido bajo los términos de la licencia Creative Commons CC BY-NC-ND (Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional) que permite usar, distribuir y reproducir en cualquier medio siempre que se citen a los autores y no se utilice para fines comerciales ni para hacer obras derivadas.
Comparte este contenido
En esta edición
- <em>REACA</em>, the journal of everyone
- Applicability of consensus methods in hip arthroscopy: a systematic review
- Evolution of the indication of arthroscopic treatment for femoroacetabular impingement and of the indication of total hip arthroplasty in patients under 60 years of age
- Evolution of glenohumeral bone defects following failed arthroscopic Bankart repair. Study of a case series
- Important articles for the surgical treatment of lateral ankle instability
- Posterolateral elbow instability with osteochondral defect of the <em>capitellum</em>; how to deal with this combination?
- Arthroscopic treatment of a femoral osteochondroma as a cause of femoroacetabular impingement. A case report
- Arthrofibrosis in the mirror
Más en PUBMED
Más en Google Scholar


Revista Española de Artroscopia y Cirugía Articular está distribuida bajo una licencia de Creative Commons Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional.







